When you pick up a generic pill, you’re counting on it to do the same job as the brand-name version. That’s where bioequivalence, the scientific standard proving two drug versions release the same amount of active ingredient at the same rate in your body. Also known as therapeutic equivalence, it’s the invisible rule that keeps generic drugs safe, effective, and affordable. Without bioequivalence, generics could be weaker, slower, or even unsafe—no matter how cheap they are.
The FDA, the U.S. agency that sets and enforces drug safety and effectiveness standards requires every generic to prove bioequivalence before it hits the shelf. That means testing blood levels after taking the drug—making sure the amount absorbed and how fast it gets there matches the brand. It’s not about looking the same or tasting the same. It’s about what happens inside you. If a generic fails this test, it doesn’t get approved. Period. This isn’t just bureaucracy—it’s why your blood pressure med, your antidepressant, or your cholesterol pill works the same whether it’s branded or generic.
But bioequivalence doesn’t mean every generic is identical in every way. Fillers, coatings, and release mechanisms can differ—and those can matter for people with sensitive stomachs or complex drug regimens. That’s why some patients still notice differences, even when the science says they shouldn’t. The drug absorption, how quickly and completely a medicine enters your bloodstream can shift slightly between brands, especially with time-release pills or narrow-therapeutic-index drugs like warfarin or thyroid meds. That’s why your doctor might stick with one brand if you’ve been stable on it.
And here’s the real impact: bioequivalence is what makes the first generic approval, the 180-day exclusivity granted to the first company to challenge a brand-name patent so powerful. That one company gets to sell the cheapest version alone, forcing prices down fast. When that exclusivity ends, more generics flood in—and prices drop even further. That’s how drugs like Eliquis and Keytruda go from $1,000 a month to under $50. It’s not magic. It’s bioequivalence in action.
You’ll find posts here that dig into how generics get approved, why some drugs are harder to copy than others, and how to talk to your doctor if you feel a switch isn’t working right. You’ll also see how acid-reducing meds can mess with absorption, why monitoring levels matters for drugs like digoxin, and how patent expirations unlock cheaper options. This isn’t theory. It’s what’s in your medicine cabinet—and what’s in your bank account.

Patients often doubt generic drug safety despite FDA approval. Learn why perceptions differ from science and how healthcare providers can address concerns to improve adherence and reduce costs.
read more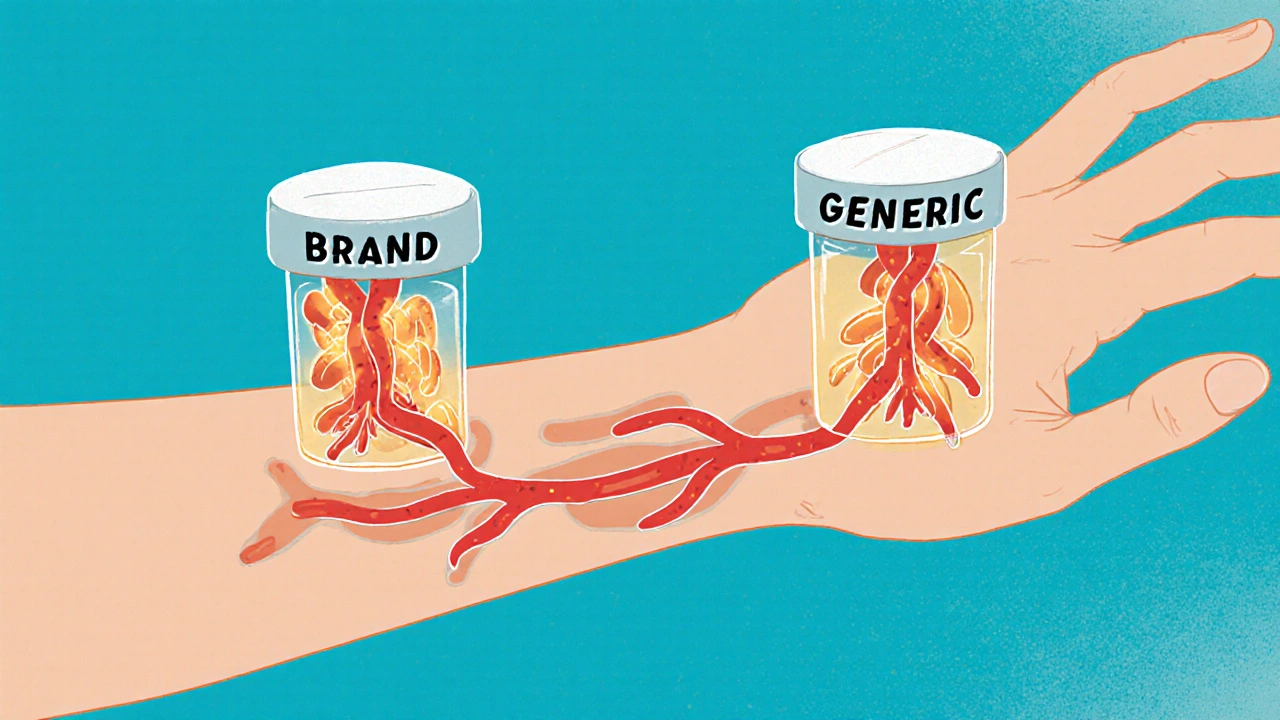
Bioequivalence testing ensures generic drugs work the same as brand-name versions. Learn why this science is critical for patient safety, how regulators enforce it, and what you should know when switching medications.
read more