When you pick up a generic pill at the pharmacy, you’re not just saving money-you’re relying on a hidden science that keeps you safe. That science is bioequivalence. It’s the reason your doctor can confidently switch you from brand-name Lipitor to a generic version of atorvastatin without worrying you’ll have a heart attack, or that your thyroid medication won’t suddenly stop working after a refill. But how do we know these cheaper pills do the same job? And why does it matter so much for your health?
What Bioequivalence Really Means
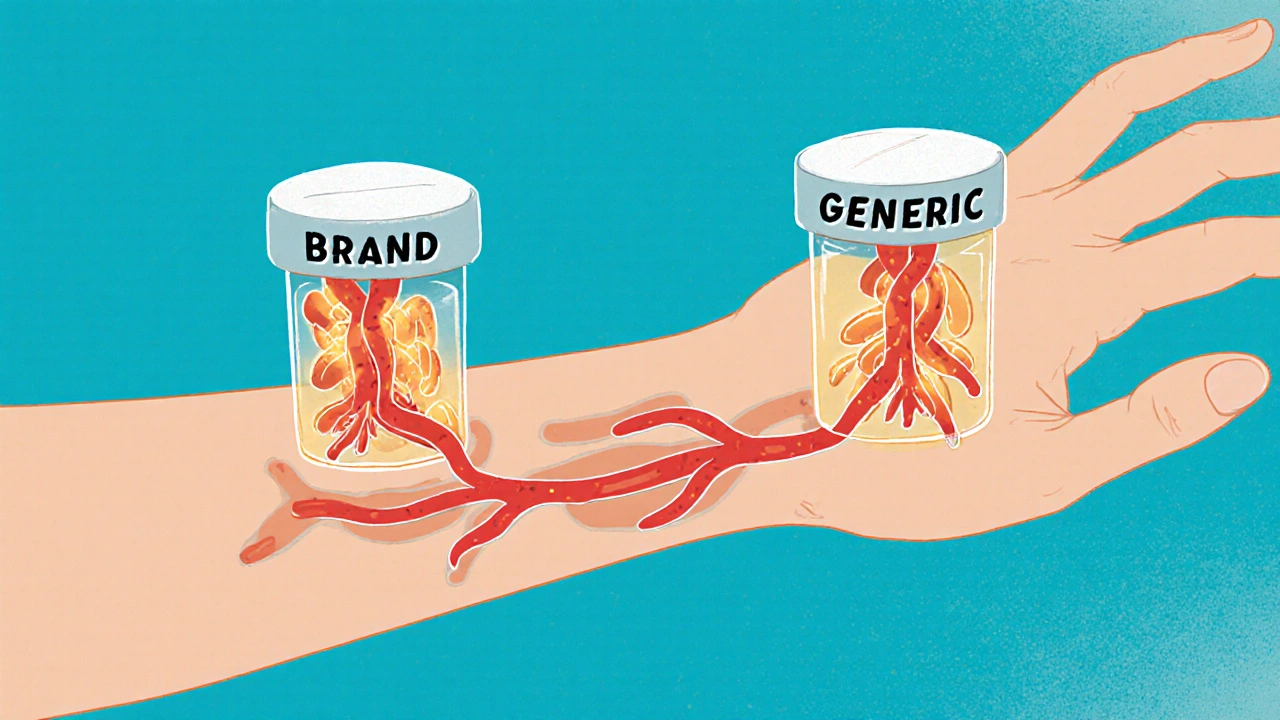
Bioequivalence isn’t just about two drugs looking the same or having the same active ingredient. It’s about proving they behave the same way in your body. That means the drug gets absorbed at the same speed and to the same level. If a generic drug releases too slowly, you won’t get enough medicine in your system. If it releases too fast, you could overdose. Either way, your treatment fails.
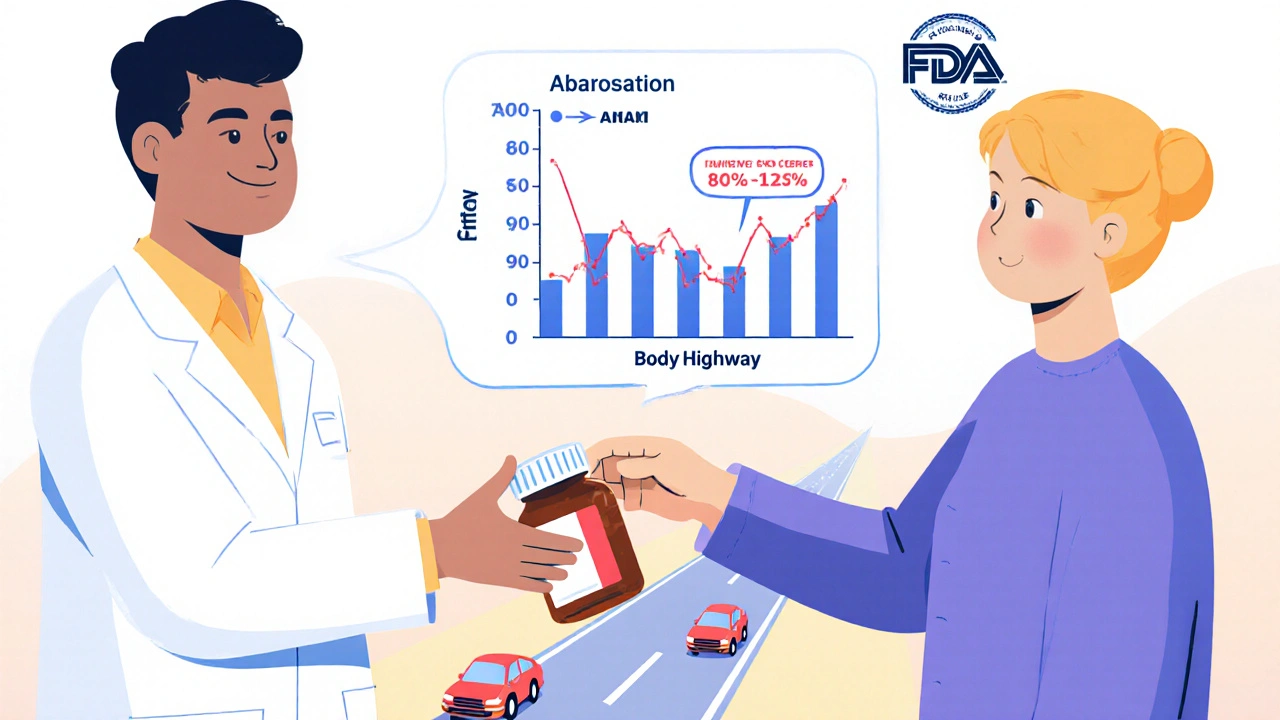
The gold standard for proving this is a pharmacokinetic study. Healthy volunteers take the brand-name drug and the generic version, usually in separate sessions, with blood samples taken over hours to track how much drug enters the bloodstream. The key numbers? AUC (total exposure over time) and Cmax (peak concentration). For most drugs, the generic’s AUC and Cmax must fall within 80% to 125% of the brand’s values. That’s not a guess-it’s a strict, science-backed limit approved by the FDA, EMA, and health agencies worldwide.
Think of it like two cars driving the same route. One’s a Honda, the other a Toyota. They don’t have to be identical. But if they both get you to the destination at the same time, with the same amount of fuel used, you can trust either one. Bioequivalence is that same logic-but for your body.
Why This Testing Protects Your Life
Some drugs have a narrow therapeutic window. That means the difference between a helpful dose and a dangerous one is tiny. Warfarin, for example, is a blood thinner. Too little, and you risk a clot. Too much, and you bleed internally. Even small differences in absorption can be life-threatening.
That’s why regulators apply tighter rules for these drugs. For warfarin, lithium, and levothyroxine, the acceptable range is narrowed to 90-111%. After the FDA updated its guidelines for levothyroxine in 2012, manufacturers had to prove their generics matched the brand’s absorption profile with far greater precision. Patient reports on Drugs.com show that since then, complaints about switching have dropped significantly-even though the generic version costs 90% less.
And it’s not just about pills. Topical creams, inhalers, and eye drops need bioequivalence testing too. A generic asthma inhaler that delivers 10% less medication per puff might seem harmless. But over weeks, that small drop can mean more ER visits. The EMA’s 2023 guidelines now require new in-vitro and in-vivo tests for these complex products, because you can’t just measure blood levels with a spray or ointment.
How the System Prevents Dangerous Switches
It’s easy to assume that if a drug has the same chemical name, it’s the same. But that’s not true. Two versions of metformin can have different fillers, coatings, or particle sizes-and those changes can alter how the drug dissolves in your stomach.
Bioequivalence studies force manufacturers to test those differences before approval. The FDA doesn’t just accept claims. They require labs to validate their analytical methods down to nanogram levels. If a generic drug’s dissolution profile doesn’t match the brand’s under different pH conditions (like with or without food), it’s rejected.
And if something goes wrong after approval? The FDA’s Adverse Event Reporting System (FAERS) tracks every reported problem. Between 2020 and 2023, only 0.07% of all adverse drug events involved generics with confirmed bioequivalence. Meanwhile, brand-name drugs accounted for 2.3%. That’s not because generics are safer by nature-it’s because the testing blocks dangerous products before they reach shelves.
When Bioequivalence Isn’t Enough
Not all drugs are created equal. Biologics-like insulin, rheumatoid arthritis drugs, or cancer treatments-are made from living cells. You can’t just copy them like a chemical pill. That’s why biosimilars need a whole different process. They must prove similarity through structural analysis, immune response tests, and clinical trials-not just blood concentration curves.
Even with small-molecule generics, challenges remain. Highly variable drugs (HVDs) like some anticonvulsants or statins behave differently in different people. For these, regulators use scaled bioequivalence, which allows a wider range (75-133%) but adds a safety net: the average difference between the generic and brand can’t exceed 10%. This prevents a product that’s wildly inconsistent from slipping through.
And then there’s the issue of metabolites. Take losartan, a blood pressure drug. Its main effect comes not from the pill itself, but from a metabolite called EXP-3174. So bioequivalence studies for losartan must measure both the parent drug and the metabolite. If the generic produces less of that active metabolite, it’s not bioequivalent-even if the original drug looks fine.
What Patients Really Experience
Some people swear their generic version doesn’t work as well. Reddit threads are full of stories: “Switched to generic sertraline and felt foggy for weeks.” “My cholesterol went up after the switch.”
These aren’t made up. But they’re rare-and usually not caused by bioequivalence failure. More often, it’s psychological (the nocebo effect), or a change in fillers causing stomach upset, or a patient who was stable on one brand and suddenly got a different generic from a different manufacturer. The FDA doesn’t approve multiple generics as identical-they’re all approved to match the original brand. But if you switch between two different generics, you’re switching between two different products, even if both are “bioequivalent” to the brand.
That’s why pharmacists are trained to stick with the same generic manufacturer unless a switch is necessary. And why many states now require pharmacies to notify patients before substituting generics.
Still, the data is clear: 87% of U.S. patients report no difference in effectiveness between brand and generic. And with generic drugs making up 90% of prescriptions but only 23% of drug spending, the system is working. In 2020 alone, generics saved the U.S. healthcare system $313 billion. That’s money that keeps insulin, cancer drugs, and heart medications affordable for millions.

The Future of Bioequivalence Testing
The field is evolving. In 2022, the FDA accepted 17 submissions using physiologically-based pharmacokinetic (PBPK) modeling-computer simulations that predict how a drug behaves in the body without needing human trials. This could cut study costs and time, especially for complex products.
Artificial intelligence is also entering the picture. Researchers are training AI to predict bioequivalence based on dissolution profiles alone. If a generic dissolves the same way as the brand in lab tests, could we skip the human study? The FDA is exploring this-but only for well-understood drugs. For anything complex, they still want human data.
Global harmonization is another big push. Right now, Japan requires fasting studies even if the brand is taken with food. The EU and U.S. don’t. That means a company making a generic for worldwide sale has to run multiple studies. The International Pharmaceutical Regulators Programme (IPRP) is working to align rules across 16 countries. That will speed up access to affordable drugs everywhere.
But the core hasn’t changed. Whether it’s a tablet, inhaler, or cream, the goal is the same: make sure the medicine in your body behaves exactly as it should. Because when your health is on the line, there’s no room for guesswork.
Are generic drugs as safe as brand-name drugs?
Yes, when they pass bioequivalence testing. Regulatory agencies like the FDA and EMA require generic drugs to prove they deliver the same amount of active ingredient at the same rate as the brand. Once approved, they’re considered therapeutically equivalent. Adverse event data shows generic drugs with confirmed bioequivalence have significantly lower rates of serious side effects than brand-name drugs.
Can switching to a generic drug cause side effects?
It’s possible, but usually not because of bioequivalence failure. Side effects after switching are more often due to different inactive ingredients (like fillers or dyes), psychological expectations, or switching between two different generics. If you notice new symptoms, talk to your pharmacist or doctor-they can help determine if it’s the drug or something else.
Why do some drugs need tighter bioequivalence limits?
Drugs with a narrow therapeutic index-like warfarin, lithium, or levothyroxine-have a small window between effective and toxic doses. Even small differences in absorption can lead to serious harm. So regulators require tighter bioequivalence ranges (90-111%) for these drugs to ensure safety.
Do bioequivalence studies always use healthy volunteers?
Most do, because it’s easier to control variables. But for drugs where stopping treatment is dangerous-like epilepsy or heart medications-studies are done in patients. This ensures the results reflect real-world use without putting people at risk.
How long does bioequivalence testing take?
A typical bioequivalence study takes 12 to 18 months and costs between $1 million and $2 million. This includes designing the trial, recruiting volunteers, conducting blood tests, analyzing data, and submitting results to regulators. Complex drugs like inhalers or topical creams can take longer and cost more.
Can I trust a generic drug approved in another country?
It depends. Countries like the U.S., EU members, Canada, Japan, and Australia have strict bioequivalence standards. But not all countries do. If you’re buying medication from outside your country’s regulatory system, there’s no guarantee it was tested properly. Always use generics approved by your local health authority.
What You Can Do
You don’t need to be a scientist to protect yourself. Here’s what matters:
- Ask your pharmacist if your generic is from the same manufacturer as your last refill. If it changed, ask if it’s the same formulation.
- Don’t assume all generics are identical. Even if they’re both approved, they can come from different factories with different fillers.
- If you feel different after switching-fatigue, dizziness, worsening symptoms-don’t ignore it. Talk to your doctor. It might be nothing. But it might be a sign.
- Use trusted sources. Check the FDA’s Orange Book or your country’s drug database to see which generics are approved for your medication.
- Remember: the goal isn’t just to save money. It’s to save lives. Bioequivalence testing makes that possible.
Generic drugs aren’t a compromise. They’re a triumph of science and regulation working together. And as long as bioequivalence remains the gatekeeper, you can trust that your next pill-no matter the price tag-is doing exactly what it’s supposed to.





Paige Lund
November 19, 2025 AT 06:39 AMYeah sure, generic drugs are fine… until your anxiety meds suddenly make you feel like a zombie for two weeks. Then you realize ‘bioequivalence’ is just corporate jargon for ‘close enough’.
Reema Al-Zaheri
November 20, 2025 AT 09:19 AMBioequivalence is not a suggestion-it is a regulatory requirement grounded in pharmacokinetic principles; the 80–125% confidence interval is statistically validated, not arbitrarily chosen. The data is transparent, the methods are peer-reviewed, and the outcomes are reproducible across global agencies.
Derron Vanderpoel
November 21, 2025 AT 21:39 PMI switched to generic levothyroxine last year and my heart started racing like I’d downed three espressos… I thought I was losing my mind. Took me three months to figure out it was the filler-corn starch, not lactose. My doc switched me back to the same generic but a different batch. Now I’m fine. Don’t ignore your body. It knows.
Timothy Reed
November 23, 2025 AT 10:49 AMThe science behind bioequivalence is robust, and the regulatory frameworks in place ensure patient safety without compromising affordability. The data consistently shows that generics, when properly tested, perform equivalently to brand-name drugs in real-world settings. This is not a cost-cutting measure-it is a public health success story.
Angela Gutschwager
November 23, 2025 AT 21:09 PMMy pharmacist switched my generic without telling me. Now I’m tired all the time. 😒
Dion Hetemi
November 25, 2025 AT 13:20 PMLet’s be real: the FDA approves generics based on studies with 24 healthy college kids who’ve never had a chronic condition. Meanwhile, real patients with liver disease, kidney failure, or metabolic disorders are being told ‘it’s the same.’ That’s not science-it’s a gamble with your life.
Codie Wagers
November 27, 2025 AT 08:08 AMThere is a metaphysical dimension to pharmacology that the FDA refuses to acknowledge: the soul of the medicine. When you ingest a pill, you are not merely absorbing a molecule-you are engaging with the intention of its creation. A brand-name drug is forged in the crucible of corporate accountability; a generic is the ghost of that intention, diluted by cost-cutting and bureaucratic indifference. The 80–125% window is not a scientific standard-it is a moral compromise. We have traded certainty for convenience, and in doing so, we have severed the sacred bond between patient and remedy.
And yet, we call this progress.
Consider the patient who, after switching to a generic, reports a change in mood, cognition, or physical sensation. The system dismisses this as the nocebo effect. But what if the body remembers? What if the subtle differences in excipients, in dissolution profiles, in the very texture of the tablet, resonate at a cellular level that blood tests cannot quantify? We measure AUC and Cmax, but we ignore the silence between the peaks-the hollow where trust used to live.
Generics are not inferior by design. They are inferior by necessity. And necessity, as history has shown, is the mother of compromise. We must ask: at what cost do we quantify safety? At what point does ‘close enough’ become ‘dangerously inadequate’?
The answer lies not in pharmacokinetics, but in philosophy. If a drug performs identically in a lab, but not in a life-does it still work?
Kara Binning
November 28, 2025 AT 00:57 AMUSA makes the best medicine in the world. Why are we letting foreign companies make our pills? This bioequivalence nonsense is just a cover for letting China and India run our healthcare. We used to make our own drugs. Now we’re trusting some factory in Bangalore to get our thyroid levels right? No. Just no. This isn’t science-it’s surrender.