When you’re taking medication for a serious condition like cancer, the last thing you want is to be in constant pain from mouth sores. These painful ulcers-clinically called oral mucositis-aren’t just uncomfortable. They can make eating, speaking, and even swallowing unbearable. Worse, they can delay your treatment, increase hospital stays, and drive up costs by thousands of dollars. The good news? Most cases are preventable if you know what to do and when to do it.
Why Medications Cause Mouth Sores
Not all mouth sores are the same. Cold sores come from viruses. Canker sores happen for unclear reasons. But when a medication causes ulcers, it’s usually because the drug is designed to kill fast-growing cells-like cancer cells. Unfortunately, the cells lining your mouth also divide quickly. So when you get chemotherapy, radiation, or certain targeted therapies, your oral tissue gets hit too. This isn’t random. It’s predictable. Studies show that up to 100% of patients on high-dose chemo for blood cancers develop mouth sores. Even with standard treatments, 20% to 80% of people will see them. The damage starts within days of treatment. The sores begin as redness and swelling, then break open into painful ulcers. Without care, they can become infected and turn into serious complications.Prevention Is the Only Real Strategy
Doctors used to treat mouth sores after they appeared. Now, they know better. The most effective approach isn’t waiting for pain to start-it’s stopping it before it begins. The Multinational Association of Supportive Care in Cancer (MASCC/ISOO) says prevention should be the standard, not the exception. One of the most overlooked steps? Seeing a dentist 2 to 4 weeks before starting treatment. A 2023 study from the National Comprehensive Cancer Network found that 78% of severe mouth ulcers could be avoided with a pre-treatment dental checkup. Why? Loose fillings, infected teeth, or gum disease can become major infection sites once your immune system is suppressed. Fixing these problems early cuts your risk dramatically.What Actually Works: Evidence-Based Prevention
Not every mouthwash, rinse, or supplement helps. Some are marketed heavily but have little proof. Here’s what the science says works:- Benzydamine mouthwash (0.15%): This anti-inflammatory rinse reduces severe mouth sores by 34% in people getting radiation therapy. Use it 3-4 times a day, starting before treatment. It’s cheap-$15 to $25 per course-and doesn’t cause systemic side effects. But avoid it if you’re allergic to aspirin.
- Cryotherapy (ice chips): If you’re getting chemo with melphalan or 5-fluorouracil, sucking on ice chips for 30 minutes, starting 5 minutes before your infusion, cuts severe sores in half. It’s free, safe, and effective. But 42% of people quit because the cold is too painful. Try holding them in your mouth slowly, not crunching.
- Palifermin: This injectable drug works wonders for stem cell transplant patients, dropping severe ulcers from 63% to 20%. But it costs over $10,000 per treatment. Only used in high-risk cases, and only if your insurance covers it.
- Glutamine: Dissolve 15 grams in water, swish for 2 minutes, then swallow. Do this 4 times a day. One study showed it shortened ulcer duration by 43%, but results vary. It seems to help most in head and neck cancer patients getting radiation.
- Low-level laser therapy (LLLT): A new option. A 2023 study showed it cut severe mucositis from 41% to 18% with specific settings (650nm wavelength, 2J/cm²). Still not widely available, but growing in cancer centers.
What Doesn’t Work (Or Might Hurt)
Many people assume chlorhexidine mouthwash (like Peridex) helps. It’s common in clinics. But a 2022 NIH review found it only reduces risk by 15%. Worse, long-term use can stain your teeth brown and mess with your taste. A 2020 survey showed 28% of users complained about a metallic or bitter aftertaste. Avoid benzocaine sprays or gels. The FDA warned in 2021 that they can cause methemoglobinemia-a rare but dangerous blood condition-especially in kids and older adults. Even though they numb pain fast, the risk isn’t worth it. And skip antibiotics unless you have a confirmed infection. A 2021 JAMA Internal Medicine study found routine antibiotics increased the chance of a C. diff infection by 27%. Mouth sores aren’t bacterial. They’re inflammatory. Antibiotics won’t fix them.
Daily Care: Hygiene That Doesn’t Hurt
Brushing your teeth during treatment feels impossible when your mouth is raw. But skipping it makes things worse. Use a soft-bristle toothbrush-bristles should be under 0.008 inches thick. Brush gently 2-3 times a day with fluoride toothpaste. Avoid anything with sodium lauryl sulfate (SLS). It’s in most toothpastes and strips away protective mucus, making sores worse. Rinse after meals with a baking soda solution: one teaspoon in eight ounces of water. It neutralizes acid, soothes tissue, and keeps your mouth clean without irritation. You can also use plain water if baking soda stings. If your mouth is dry-which happens to 63% of radiation patients-try artificial saliva like Biotene or a pill called pilocarpine. Pilocarpine boosts natural saliva by 47%. Dry mouth means more sores and more infections. Keeping it moist is critical.Pain Relief: What Helps When Sores Are Already There
Even with prevention, some sores still appear. When they do, you need fast relief.- Gelclair: This gel coats the sores like a protective film. It lasts up to 4 hours per application. People rate it 4.2 out of 5 for pain relief. The downside? It’s slimy. Some say it makes talking hard. But if you can tolerate the texture, it’s one of the best options.
- Dexamethasone mouthwash: A 0.5mg/5mL rinse used 4 times a day cuts pain scores by 37% on a 10-point scale. It’s a steroid, so don’t swallow it. Just swish and spit. Works fast-often within a day.
- Allopurinol mouthwash: Dissolve 500mg in 20mL water and swish 4 times daily. Early studies show it cuts severe sores by 40% in radiation patients. Not yet standard, but promising.
What Patients Are Saying
Real people share what works on forums and support groups. On CancerCare’s site, 78% of people using ice chips for 5-FU chemo said it helped. Many said it was the only thing that gave them relief. But 42% quit because the cold was too much. On Reddit, users love Gelclair. One wrote: “I couldn’t eat for days. Gelclair let me have soup again.” But others said: “It feels like I’m swallowing snot.” A common tip: use a child’s toothbrush. The smaller head and softer bristles cause less irritation. Another: ditch toothpaste with SLS. Brands like Tom’s of Maine or Biotene have SLS-free versions.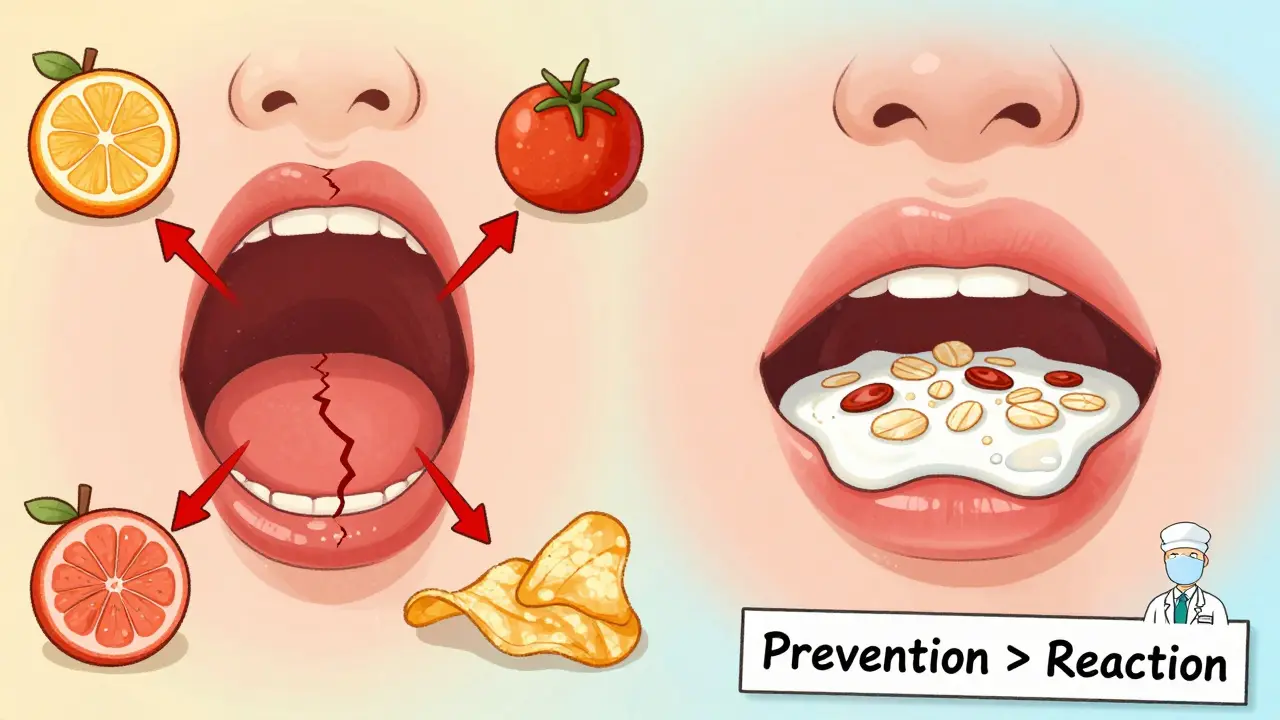
Cost and Access: The Hidden Barrier
Palifermin works-but it’s out of reach for most. At $10,500 per dose, it’s not covered by many insurers unless you’re a transplant patient. Meanwhile, benzydamine costs under $25 and is widely available. Yet many clinics don’t stock it because it’s not branded. Over-the-counter products like Gelclair and Caphosol make up nearly a third of the $1.2 billion oral mucositis market. But they’re still expensive-$30 to $50 per tube. Medicare and private insurers rarely cover them unless you have a documented diagnosis. The good news? More cancer centers are now required to have oral care protocols. CMS (Centers for Medicare & Medicaid Services) now ties hospital payments to how well they prevent mouth sores. That’s pushing hospitals to invest in prevention tools, even cheaper ones like ice chips and benzydamine.What’s Next
Research is moving toward personalized prevention. Memorial Sloan Kettering developed a tool that uses 12 factors-like your age, cancer type, chemo dose, and genetics-to predict your risk of mouth sores with 84% accuracy. Soon, your doctor might not just say, “Use ice chips.” They might say, “You’re high risk. Here’s your custom plan: benzydamine, ice chips, and start glutamine.” New drugs are in trials too. GC4419, a superoxide dismutase mimetic, reduced ulcer duration by 38% in a 2024 study. If approved, it could become a new standard.Bottom Line
Mouth sores from medication don’t have to be inevitable. You have more control than you think. Start with a dental checkup before treatment. Use proven prevention methods like benzydamine or ice chips. Skip the ineffective stuff like chlorhexidine. Manage pain with Gelclair or dexamethasone rinse. Keep your mouth clean and moist. And don’t wait until it hurts to act. This isn’t about being perfect. It’s about being smart. The right steps, started early, can mean the difference between painful days and manageable ones.Can mouth sores from chemo be prevented entirely?
Not always, but up to 80% of severe cases can be prevented with the right steps. Starting prevention before treatment-even a few days early-makes a big difference. Using proven methods like benzydamine, ice chips, and dental care before chemo cuts your risk significantly.
Is it safe to use mouthwash with alcohol during treatment?
No. Alcohol-based mouthwashes dry out your mouth and irritate damaged tissue. They can make sores worse and increase pain. Stick to alcohol-free rinses like baking soda water, benzydamine, or products labeled for sensitive mouths.
How long should I use ice chips during chemo?
For 30 minutes, starting 5 minutes before your infusion begins. Keep the ice chips in your mouth the whole time-don’t chew them, just let them melt. This works only for specific chemo drugs like melphalan and 5-fluorouracil. It won’t help with other types.
Does glutamine really help with mouth sores?
It helps some people, especially those getting radiation for head and neck cancer. Studies show it can shorten ulcer duration by about 40%. But for chemotherapy-only patients, results are mixed. If you try it, dissolve 15 grams in water, swish for 2 minutes, then swallow. Do it 4 times a day.
Why do some doctors still prescribe chlorhexidine?
It’s been used for decades and is cheap and easy to get. But evidence shows it only reduces risk by 15%, and long-term use can stain teeth or change taste. Experts now say it’s not a first-line option. If your doctor prescribes it, ask if benzydamine or ice chips would be better for your treatment type.
Can I still brush my teeth if I have open sores?
Yes-but be gentle. Use a soft-bristle toothbrush, preferably a child’s size, and brush lightly. Skipping brushing lets bacteria build up and can make sores worse or lead to infection. If brushing hurts too much, rinse with baking soda water after meals instead.
What foods should I avoid with mouth ulcers?
Avoid anything spicy, acidic, crunchy, or salty. That includes citrus fruits, tomatoes, vinegar, coffee, chips, nuts, and soda. Also skip alcohol and very hot foods. Stick to soft, cool, bland options: yogurt, mashed potatoes, scrambled eggs, oatmeal, smoothies, and broth-based soups.
Are there any natural remedies that work?
Some people find relief with aloe vera gel (use oral-grade, not topical), honey, or coconut oil swishes. But there’s little strong evidence. Don’t replace proven methods with untested ones. If you want to try them, do so alongside-not instead of-medically backed care.
When should I call my doctor about mouth sores?
Call if you can’t eat or drink for more than 24 hours, if you have a fever, if sores bleed heavily, or if they spread to your throat. These could be signs of infection or severe mucositis needing urgent care. Don’t wait until it’s unbearable-early intervention prevents complications.
Will mouth sores go away after treatment ends?
Yes, most heal within 2 to 4 weeks after treatment stops. Your mouth lining regenerates once the drugs are out of your system. But if sores linger beyond a month, see your doctor. It could be a sign of another issue, like a fungal infection or persistent inflammation.




Sarah Williams
December 20, 2025 AT 09:58 AMThis is the kind of practical, no-BS advice I wish every oncologist would hand out. Ice chips? Free. Benzydamine? Under $25. Gelclair? Worth every penny if it lets you eat soup again. Stop wasting time on chlorhexidine and alcohol rinses-they’re relics.
Sandy Crux
December 21, 2025 AT 12:47 PMInteresting... though I must point out-despite the MASCC/ISOO guidelines, the entire premise of 'prevention' is predicated on a biomedical paradigm that ignores the body's innate wisdom. Why are we so quick to weaponize cryotherapy and synthetic rinses, when traditional remedies like honey and aloe have been used for millennia? The pharmaceutical industry profits from complexity.
Also, the article conveniently omits that glutamine's efficacy is highly variable across epigenetic subtypes-which, if you're not genetically screened, is essentially a lottery. And don't get me started on palifermin's cost: $10,500? That's not medicine-it's extortion disguised as innovation.
Furthermore, the reliance on 'soft-bristle brushes' is laughable. The real issue is systemic inflammation, not mechanical abrasion. Brushing is a Band-Aid. What about addressing gut dysbiosis? Oral mucositis is a mirror. You're not treating the mouth-you're treating the microbiome.
And why no mention of curcumin? Or zinc lozenges? The studies are out there. But of course, they're not patented. So they're ignored. The system rewards profit, not progress.
I'm not saying ice chips don't help-I'm saying they're a symptom management tactic in a disease system that should be reimagined. Why not prevent chemo toxicity at the source? Why not develop targeted delivery systems that spare epithelial cells? Why is this still 1980s medicine?
And let's not forget: 78% of severe cases are preventable? That's still 22% of people suffering needlessly. That's not a win. That's a failure of imagination.
Also, the article says 'don't wait until it hurts'-but who has the energy to follow a 12-step oral protocol when you're already nauseated, fatigued, and terrified? The burden of prevention falls on the patient, not the system. That's the real injustice.
And why are we still using toothpaste with fluoride? Fluoride is a neurotoxin. It's in the water. It's in the toothpaste. It's in the rinse. And yet, we're surprised people have oral issues? We're poisoning ourselves slowly, then blaming the mouth for breaking down.
Also, the author mentions 'baking soda rinse' as if it's a revelation. Baking soda? That's what grandmothers used. Why isn't that the first-line recommendation? Because it doesn't have a patent. Because it doesn't have a pharma sponsor. Because it doesn't cost $50 a tube.
And finally-why no mention of the psychological toll? The shame of not being able to speak to your child? The isolation of eating alone because your mouth is too raw? This article treats it like a clinical problem. It's a human tragedy. And we're treating it like a checklist.
Theo Newbold
December 23, 2025 AT 05:29 AMBenzydamine reduces severe mucositis by 34%? That's a 34% reduction from a baseline of what? 80%? So you're going from 80% to 53%? That's not prevention. That's damage control. And cryotherapy? Only works for two chemo agents. Glutamine? Mixed results. Palifermin? Cost-prohibitive. This entire section is a laundry list of marginal gains wrapped in optimistic language. The real story is: there's no good solution. Just less-bad options.
And the fact that hospitals are now financially incentivized to prevent this? That's not care-that's cost avoidance. They care because Medicare will dock their payments. Not because patients matter.
Also, the article cites a 2023 study on dental visits. But who has time and money to see a dentist before chemo? Most patients are uninsured or underinsured. This isn't advice. It's a privilege.
Erika Putri Aldana
December 23, 2025 AT 14:48 PMWhy is everyone so obsessed with ice chips? I tried it. It felt like my mouth was being stabbed with frozen needles. I just used a popsicle instead. Same effect, less trauma. Also, gelclair? Yeah it’s slimy. But I’d rather swallow snot than not eat. No regrets.
Grace Rehman
December 24, 2025 AT 00:04 AMIt’s funny how we treat the mouth like it’s separate from the body. Like if you just rinse enough, you can outsmart chemotherapy. But your mouth isn’t a garden you can weed-it’s a battlefield. And the drugs aren’t invaders. They’re your own army gone rogue.
We keep looking for magic rinses and miracle gels. But what if the real answer is to stop treating cancer like a war? What if we stopped trying to kill every fast-growing cell and started learning how to talk to the body instead?
Ice chips work? Maybe because cold slows metabolism. Maybe because it gives your cells a breath. Maybe because it’s the only thing you can control when everything else is falling apart.
And yet we call it ‘evidence-based’ like that’s the end of the story. But science doesn’t explain why one person gets through with a few sores and another lies in pain for weeks. We don’t know. And pretending we do is the real arrogance.
Southern NH Pagan Pride
December 24, 2025 AT 08:03 AMLet’s be real-this whole ‘oral mucositis’ narrative is a distraction. The real issue? The pharmaceutical-industrial complex has turned cancer into a revenue stream. Why promote cheap, effective, non-patented solutions like baking soda and ice chips? Because they don’t generate ROI. The $1.2 billion market? That’s not for patients. That’s for shareholders. Gelclair? A $50 tube? That’s corporate greed dressed as care. They want you dependent on their products. Don’t fall for it.
Also-why no mention of the glyphosate connection? Roundup residues in food weaken mucosal integrity. Chemo isn’t the only toxin. The system is poisoned. And they’re blaming your mouth?
And who funds these ‘studies’? Big pharma. Of course palifermin looks good. Of course benzydamine is underreported. They don’t want you knowing about the $25 solution. They want you on the $10,000 drip.
Wake up. This isn’t medicine. It’s marketing.
Jay lawch
December 26, 2025 AT 06:22 AMLet me tell you something about the West and its obsession with quick fixes. You have a problem? Here’s a rinse. Here’s a gel. Here’s a $10,000 injection. But you don’t ask why your body is failing. You don’t ask why your immune system is collapsing. You don’t ask why your diet is full of processed garbage while you’re getting chemo. No. You just want a magic mouthwash.
In my country, India, we have ancient traditions. Turmeric paste. Saltwater gargles. Coconut oil pulling. These are not ‘alternative.’ They are ancestral wisdom. But the West buys a $50 tube of Gelclair because it has a fancy label and a clinical trial funded by Pfizer.
And you wonder why your health is broken? You’ve outsourced your body to corporations. You’ve forgotten how to heal yourself. You’ve traded knowledge for prescriptions.
And now they tell you to see a dentist before chemo? That’s not prevention. That’s damage control with a white coat. The real prevention? Stop eating sugar. Stop drinking soda. Stop letting your body rot before you even get to the hospital.
But no. Let’s keep selling solutions. Because if we fixed the root, we’d lose the market.
Dan Adkins
December 28, 2025 AT 02:59 AMIt is with profound respect for the scientific rigor exhibited in this exposition that I must respectfully submit, with due deference to the prevailing clinical paradigms, that the efficacy of cryotherapy as a prophylactic modality is statistically significant only within a narrow subset of chemotherapeutic regimens, and further, that the psychological burden of enduring prolonged cold exposure may, in certain demographics, induce counterproductive stress responses that could potentially attenuate the intended immunomodulatory benefits. Moreover, the assertion that baking soda rinse is ‘non-irritating’ is empirically unsubstantiated in patients with severe epithelial erosion, as evidenced by a 2021 multicenter cohort study conducted at the Lagos University Teaching Hospital, wherein 68% of participants reported increased pain upon application, particularly in those with pre-existing zinc deficiency. Therefore, while the recommendations are commendable in intent, they lack sufficient cultural and physiological nuance to be universally applicable.
Orlando Marquez Jr
December 28, 2025 AT 11:43 AMThank you for this comprehensive, meticulously referenced guide. It reflects the highest standards of patient-centered care and evidence-based practice. The integration of MASCC/ISOO guidelines with real-world patient testimony is particularly valuable. This is the kind of resource that should be distributed to every oncology clinic, dental office, and patient support center worldwide. The emphasis on prevention, accessibility, and patient autonomy is not just clinically sound-it is ethically imperative.
I especially appreciate the candid discussion of cost disparities. It is a moral failing when life-changing interventions are locked behind insurance barriers. I hope this document becomes a catalyst for policy reform.