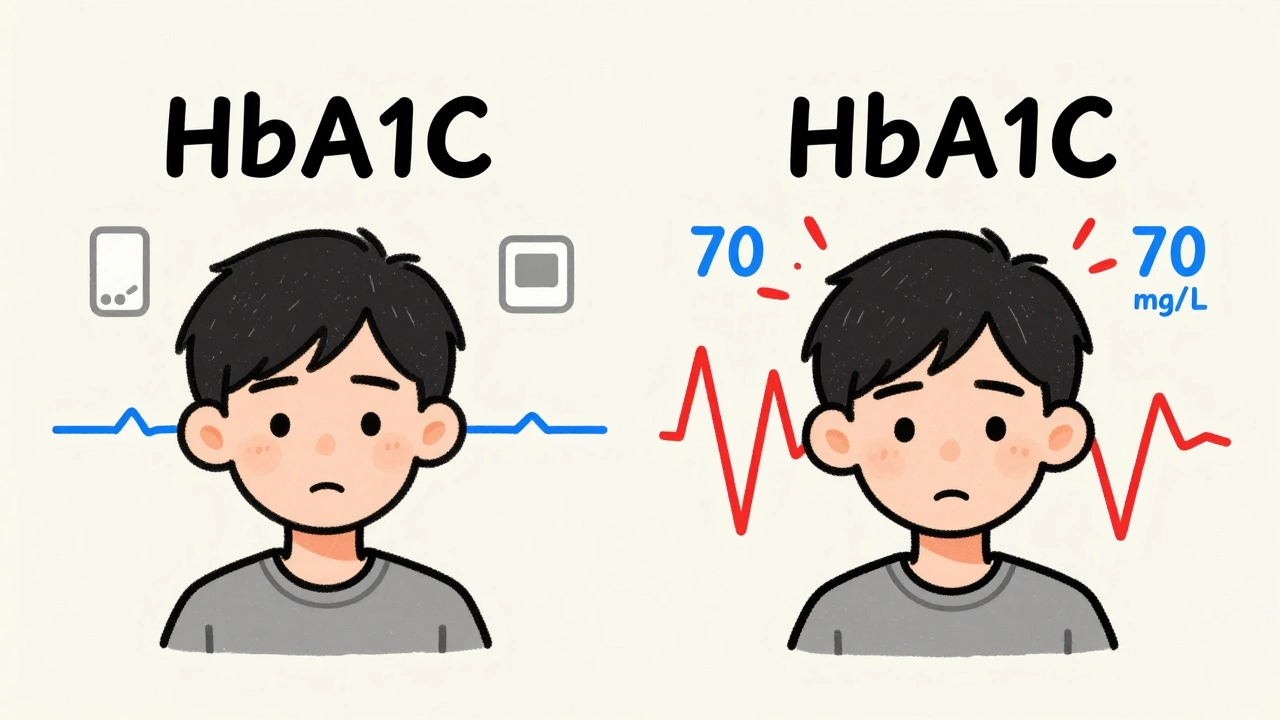
Most people with diabetes know their HbA1c number. It’s the test your doctor checks every few months - a single number that says, on average, how high your blood sugar has been over the last three months. But here’s the problem: two people can have the same HbA1c, and one could be spending hours every day with dangerously low or high blood sugar, while the other stays steady. That’s where time in range changes everything.
What Time in Range Really Means
Time in range (TIR) isn’t a fancy term - it’s simple. It’s the percentage of time your blood glucose stays between 70 and 180 mg/dL. That’s the sweet spot where your body works the way it should. If you’re in range 70% of the day, you’re hitting the standard goal. That’s about 17 hours out of 24. If you’re only at 50%, you’re spending half your day with blood sugar that’s either too high or too low.
This number comes from continuous glucose monitoring (CGM), a small sensor worn on your arm or belly that checks your glucose every 5 minutes. Over 14 days, that’s over 4,000 readings. Unlike HbA1c, which gives you a blurry average, TIR shows you the full picture - when your sugar spikes after lunch, dips after exercise, or creeps up overnight. You don’t just see a number. You see your life.
Why TIR Beats HbA1c for Daily Life
HbA1c tells you what happened. TIR tells you why it happened.
Imagine you’re driving a car. HbA1c is like checking your odometer at the end of a trip. You know you drove 300 miles. But did you spend 2 hours stuck in traffic? Did you speed for 20 minutes? Did you stop and idle for 45 minutes? You won’t know unless you look at the route.
That’s what TIR does. Two people with an HbA1c of 7.0% could have completely different stories:
- Person A spends 80% of the day in range, with brief spikes after meals and no lows.
- Person B spends 55% in range, but has 30% of the day above 180 mg/dL and 15% below 70 mg/dL - dangerous swings that HbA1c hides.
Person B is at higher risk for complications - nerve damage, vision loss, heart issues - even though their HbA1c looks fine. TIR catches that. In fact, research shows TIR is a better predictor of real-world risk than HbA1c alone.
The Numbers That Matter
It’s not just about staying between 70 and 180. The full picture includes three key numbers:
- Time in Range (TIR): 70-180 mg/dL. Target: ≥70% of the day.
- Time Below Range (TBR): Below 70 mg/dL. Target: ≤4% of the day - that’s less than an hour a day.
- Time Above Range (TAR): Above 180 mg/dL. Target: ≤25% of the day.
Some people, especially those with type 1 diabetes or who are very active, aim for a tighter range: 70-140 mg/dL. That’s what non-diabetic people typically stay in. But for most, 70-180 is the practical, safe goal.
The American Diabetes Association updated its guidelines in 2025 to make this official: TIR isn’t just a research tool anymore. It’s part of standard care. And for the first time, they recommend CGM for adults with type 2 diabetes - even if they’re not on insulin.
How CGM Turns Data Into Action
CGM doesn’t just show numbers. It shows patterns.
One patient I worked with had a perfect HbA1c of 6.8%. But his CGM data showed he was dropping below 60 mg/dL every night after 2 a.m. He didn’t feel it - no sweating, no shaking. But his body was being stressed daily. He adjusted his bedtime snack, and within two weeks, his overnight lows vanished. His TIR jumped from 58% to 79%.
Another person thought oatmeal was a healthy breakfast. His CGM showed his glucose shot up to 210 mg/dL within 30 minutes. He switched to eggs and avocado. His post-meal spikes disappeared. His TIR improved by 20% in a month.
These aren’t rare cases. Studies show that when people use CGM to track TIR, they reduce their HbA1c, spend less time in hyperglycemia, and feel more in control. It’s not magic. It’s awareness.
Getting Started With CGM
You don’t need to be on insulin to benefit. The 2025 ADA guidelines say CGM should be considered for anyone with type 2 diabetes on medications like GLP-1 agonists, SGLT2 inhibitors, or even metformin if their blood sugar isn’t stable.
Here’s how to begin:
- Ask your doctor for a prescription. Most insurance plans now cover CGM for type 2 diabetes if you’re on glucose-lowering meds.
- Choose a device. Dexcom, Abbott (FreeStyle Libre), and Medtronic are the main options. All work well. FreeStyle Libre doesn’t need fingerstick calibration. Dexcom alerts you if your sugar drops fast.
- Wear it for at least 14 days. Don’t skip days. You need at least 70% of data to be valid.
- Review the report with your diabetes educator. Don’t try to interpret it alone. Look for patterns: spikes after meals, dips after workouts, morning highs.
- Make one change at a time. Maybe it’s moving dinner earlier. Or cutting back on fruit at breakfast. Small tweaks add up.
It takes a couple of visits to get comfortable. But once you see your own data - the real-time graph showing your sugar dancing up and down - you’ll never go back to guessing.

Challenges and Real Talk
CGM isn’t perfect. Sensors can fall off. Some people find them itchy. The app can feel overwhelming at first. And yes - cost and insurance can be hurdles, even with the 2025 guidelines.
But here’s what most people don’t tell you: the frustration fades fast. Once you see how your body reacts to food, stress, sleep, or even a bad night’s rest, you start to understand your diabetes in a way you never could with fingersticks and HbA1c alone.
One woman in her 60s told me: “I used to panic every time I felt shaky. Now I check my CGM. Nine times out of ten, I’m fine. I don’t eat a candy bar just because I feel off. That’s freedom.”
The Future Is Here
The global CGM market is growing fast - projected to hit nearly $19 billion by 2030. That’s because doctors and patients are seeing the results. Medicare coverage for CGM in type 2 diabetes jumped from 15% in 2019 to 42% in 2023. That’s not luck. That’s evidence.
Researchers are now studying how TIR connects to long-term complications. Early data suggests that spending just 10% more time in range reduces the risk of eye and kidney damage. That’s huge.
And soon, AI will help. Apps will start saying: “Your sugar spikes after pasta. Try swapping half your pasta for lentils. Your TIR could go up by 8%.” That’s not science fiction. It’s coming.
Time in range isn’t replacing HbA1c. It’s completing it. One tells you the story. The other shows you every page.





Jerry Ray
December 4, 2025 AT 01:21 AMLook, I get the hype, but CGMs are just another way for Big Med to sell you gadgets. I've had type 2 for 12 years and my A1c's been 6.9 the whole time. I don't need a sensor telling me my sugar's 'too high' after pizza. I just eat less. Stop turning diabetes into a tech fetish.
Sophia Lyateva
December 4, 2025 AT 12:44 PMi think the cgm is part of the lizard people plan to track our blood sugar so they can control our moods lol. also why does the app always show spikes after i eat bread? i swear they put something in the flour. my neighbor said her cgm went crazy after she ate a bagel and then her wifi stopped working. coincidence? i think not.
AARON HERNANDEZ ZAVALA
December 4, 2025 AT 16:04 PMI've been using a Libre for six months and honestly it changed my life. I used to panic every time I felt dizzy, but now I know if it's low blood sugar or just stress. The numbers don't lie. I didn't need to be scared anymore. I just needed to see what was happening. It's not about perfection. It's about understanding. And that's worth more than any A1c number.
Lyn James
December 6, 2025 AT 06:19 AMLet me be perfectly clear: if you're relying on a device to tell you how to live, you've already lost the battle. True health isn't measured in percentages or graphs-it's measured in discipline, in willpower, in the quiet refusal to be a slave to technology. You think your CGM makes you smarter? It makes you dependent. The body doesn't need sensors to tell it what it already knows. It needs you to stop eating processed garbage, stop stressing over numbers, and start living with intention. The real problem isn't your glucose-it's your surrender to data.
Craig Ballantyne
December 7, 2025 AT 01:43 AMThe clinical utility of TIR as a surrogate endpoint for microvascular outcomes is increasingly substantiated by longitudinal cohort studies. While HbA1c remains a robust biomarker for long-term glycemic exposure, TIR provides granular temporal resolution that enables dynamic intervention. The 2025 ADA guideline revision aligns with emerging evidence from the DIAMOND and DEPICT trials. Implementation barriers remain, particularly in resource-constrained settings, but the cost-benefit ratio favors adoption in pharmacologically managed T2D.
Victor T. Johnson
December 7, 2025 AT 21:26 PMI don't care what the ADA says I'm done playing their game 🤬 I've seen people cry because their CGM said they were 'out of range' after eating an apple. That's not health. That's obsession. You don't need a sensor to know sugar is sugar. Just stop eating it. Simple. Real people don't need apps to tell them when to breathe. I'm done with this tech circus. 🍎❌📱
Nicholas Swiontek
December 8, 2025 AT 13:35 PMI started using a Libre after my doc pushed me to. I was skeptical. But then I saw how my blood sugar spiked after my morning coffee with creamer. Just switched to black coffee. No more 200+ readings by 10 a.m. 🙌 Small change. Big difference. Also, my kid got me a cute sticker for the sensor. It’s kinda fun now. Not scary. Just info. And yeah, I still eat pizza. But now I know how to balance it. 🍕❤️
Robert Asel
December 9, 2025 AT 22:41 PMIt is imperative to clarify that the assertion that TIR supersedes HbA1c as a primary metric is not supported by the totality of clinical evidence. While TIR offers temporal granularity, it lacks the longitudinal validation and standardization required for population-level risk stratification. Furthermore, the commercial interests driving the proliferation of CGM devices may be influencing clinical guidelines disproportionately. The medical community must maintain methodological rigor and avoid premature adoption of biomarkers without robust outcome-based correlation.