Medication-Food Interaction Checker
Enter your medication to see how certain foods might affect it. Based on research from JAMA and NIH studies in the article "Lifestyle Changes to Reduce Medication Side Effects".
Potential Interactions
What You Can Actually Do to Cut Down on Medication Side Effects
You’re taking your pills on time. You read the label. You even set reminders. But still, you feel off-nauseous, tired, dizzy, or just plain drained. And no one ever told you that lifestyle changes could be the missing piece. Turns out, how you eat, move, sleep, and handle stress doesn’t just support your health-it directly changes how your body reacts to medicine.
A 2021 study in JAMA Internal Medicine found that side effects from medications lead to nearly 7 out of every 100 hospital visits. That’s not just inconvenient-it’s dangerous. But here’s the good news: you don’t have to just suffer through them. Real, research-backed lifestyle tweaks can slash side effects by 30% or more, sometimes even letting you take lower doses. And no, this isn’t about replacing your meds. It’s about making them work better-with fewer headaches.
How Food Changes How Your Meds Work
What you eat isn’t just fuel-it’s a chemical partner to your medication. Some foods boost drug effects. Others block them. And a few can turn a safe pill into a problem.
Take warfarin, a blood thinner. If you suddenly start eating a bunch of kale, spinach, or broccoli-foods high in vitamin K-you’re undoing its effect. One study showed vitamin K intake above 150 micrograms a day can cut warfarin’s power by up to half. That’s not a minor bump-it’s a risk of clots.
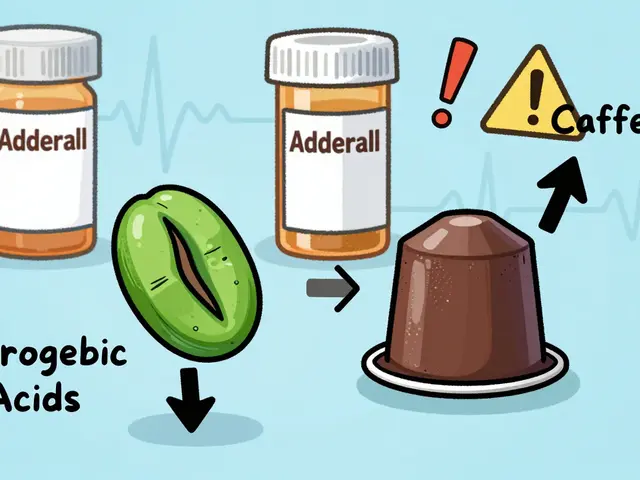
Then there’s grapefruit juice. It sounds healthy, right? But it messes with an enzyme in your gut called CYP3A4. That enzyme normally breaks down drugs like statins (atorvastatin, simvastatin), certain blood pressure meds, and even some anxiety pills. When grapefruit juice blocks it, your body absorbs way more of the drug. One study found just 200ml of grapefruit juice daily could spike statin levels by 15% to 50%. That’s enough to trigger muscle pain or liver stress.
For diabetes meds like metformin, which often cause stomach upset, timing matters more than you think. A 2022 analysis of 27 studies showed that keeping your carb intake steady-around 30 grams per meal-reduced nausea and diarrhea by 37%. Eating large, carb-heavy meals? That’s when your gut rebels.
And don’t forget salt. If you’re on blood pressure meds, your sodium intake can undo their work. The DASH diet, backed by the NIH since the 90s, proves that cutting sodium to 1,500 mg a day (down from the average 3,400 mg) lowers blood pressure as much as one pill. That means your doctor might be able to reduce your dose-or even take you off one.
Move More, Feel Better, Need Less
Exercise isn’t just for weight loss. It’s a powerful tool to help your body handle meds better.
For people on beta-blockers-meds that slow the heart rate and often cause fatigue-just 10 minutes of walking twice a day, slowly building up to 30 minutes five days a week, improved energy levels by 41% within eight weeks, according to the American Heart Association. Same goes for statins. Muscle aches? That’s common. But adding two days a week of light resistance training-like lifting light weights or doing bodyweight squats and lunges-cut muscle pain in half. Add 200mg of coenzyme Q10 daily, and the drop was even bigger: from 29% of users reporting pain to just 11%.
For those on GLP-1 drugs like semaglutide (Ozempic, Wegovy), nausea is the #1 complaint. But research shows you can cut that by more than half. How? Eat slower. Take at least 20-30 minutes per meal. Eat smaller portions-under 500 calories. Avoid spicy, greasy, or acidic foods. And never eat within three hours of bedtime. Add in 2.2 to 3 liters of water daily, and nausea dropped from 73% to 29% during dose increases.
And for antidepressants? Weight gain is a real issue. One study found people gained an average of 7.3 pounds in the first year. But those who did 150 minutes of moderate exercise weekly (like brisk walking or cycling) and ate enough protein (1.6 grams per kilogram of body weight) cut that gain by 68%.
Sleep: The Secret Medication Booster
You think your pill does all the work? Think again. Your liver, which breaks down most meds, runs on a clock. And that clock runs best when you sleep.
The National Sleep Foundation found that people who got 7-9 hours of quality sleep each night metabolized drugs like statins, antidepressants, and painkillers 22% faster. Why? Because liver enzymes-especially CYP3A4-work more efficiently when your circadian rhythm is stable.
But if you’re tossing and turning, your body doesn’t clear the drug properly. That means higher levels build up overnight, increasing side effects like dizziness, grogginess, or even liver strain. A consistent sleep schedule-even on weekends-makes a measurable difference. No screens an hour before bed. Keep your room cool. Stick to the same bedtime and wake-up time. It’s not magic. It’s biology.
Stress Is Making Your Meds Less Effective
Chronic stress floods your body with cortisol. And cortisol doesn’t just make you feel anxious-it interferes with how your brain and body respond to meds.
A 2021 study in JAMA Psychiatry showed that people who did 30 minutes of mindfulness meditation daily lowered their cortisol levels by 27%. For those on antidepressants, that meant a 31% improvement in how well the drugs worked-and fewer side effects like weight gain, fatigue, or emotional numbness.
Stress also messes with digestion. If you’re on a med that causes nausea or constipation, stress makes it worse. That’s why simple practices like deep breathing, walking in nature, or even journaling for 10 minutes a day can help your body absorb and process meds more smoothly.
One program at the Cleveland Clinic combined twice-daily 10-minute mindfulness sessions with other lifestyle changes. The result? A 72% reduction in medication use among patients with metabolic conditions-because their bodies started working better on their own.
What Your Doctor Should Be Asking (But Probably Isn’t)
Here’s the frustrating part: most doctors don’t ask about your lifestyle when adjusting your meds. A 2023 survey found only 38% of primary care visits included any kind of lifestyle check-even though 76% of patients take two or more drugs with known lifestyle interactions.
But the evidence is clear. The American College of Physicians now says: before increasing a dose or switching meds, check the lifestyle factors first. Why? Because 22% of cases where a drug seems to “stop working” are actually caused by poor sleep, high stress, or bad eating-not the medicine itself.
Ask your doctor these questions:
- Could my diet be interfering with this medication?
- Is there a specific time I should take this relative to meals?
- Could exercise help reduce the side effects I’m having?
- Should I be checking my sleep or stress levels?
Don’t wait for them to bring it up. Bring it up yourself. You’re not being difficult-you’re being smart.

Real People, Real Results
Meet Maria, 58. She was on four meds: blood pressure, cholesterol, diabetes, and an antidepressant. She felt exhausted, bloated, and emotionally flat. Her doctor wanted to add another pill.
Instead, she started working with a health coach. She began walking 30 minutes five days a week. She ate three balanced meals a day with 30g of protein each. She cut out grapefruit juice and switched to herbal tea. She went to bed at 10:30 p.m. and woke at 6:30 a.m. every day. She did 10 minutes of breathing exercises before bed.
Eight weeks later, her blood pressure dropped enough that her doctor reduced one pill. Her cholesterol improved without increasing her statin dose. Her blood sugar stabilized. And her depression symptoms? They lifted-not because she got a new drug, but because her body finally had the support it needed.
That’s not rare. That’s repeatable.
Don’t Skip the Supervision
Let’s be clear: none of this means you stop or change your meds on your own. The FDA, the American Medical Association, and every major medical group warn against it. Stopping blood pressure meds suddenly can cause rebound spikes. Skipping insulin can lead to dangerous highs. Even small changes need medical oversight.
The goal isn’t to ditch your prescriptions. It’s to make them safer, more effective, and gentler on your body. Work with your doctor. Track your symptoms. Keep a journal of what you eat, how much you move, how you sleep, and how you feel. Bring it to your next appointment.
Medications are powerful. But your daily habits? They’re the silent force that determines whether those pills help you-or hurt you.
Quick Start: 5 Lifestyle Moves to Try This Week
- Track your sodium. Use a free app like MyFitnessPal to log your salt intake. Aim for under 1,500 mg daily if you’re on blood pressure meds.
- Swap grapefruit juice. Replace it with water, green tea, or orange juice (if you’re not on statins).
- Move for 10 minutes twice a day. Walk, stretch, dance-just get moving. Build up to 30 minutes five days a week.
- Eat your last meal 3 hours before bed. Especially if you’re on GLP-1 drugs or have acid reflux.
- Try 10 minutes of deep breathing before bed. Inhale for 4 counts, hold for 4, exhale for 6. Repeat five times.
These aren’t big changes. But over time, they change everything.





Elaine Douglass
December 17, 2025 AT 13:45 PMI started doing the 10-minute breathing before bed and honestly? My anxiety meds finally stopped making me feel like a zombie. No joke.
Changed my life.
Aadil Munshi
December 18, 2025 AT 00:17 AMWow, another ‘lifestyle hack’ article that ignores the fact that most people can’t afford organic kale, don’t have 3 hours to prep meals, or work three jobs.
It’s not that we’re lazy-it’s that capitalism doesn’t care if your statins give you muscle pain.
Matt Davies
December 18, 2025 AT 20:00 PMThis is the kind of post that makes me wanna hug my pharmacist. Seriously. I’ve been on metformin for 5 years and the only thing that tamed the gut chaos was eating carbs in 30g chunks like a nerd with a food scale.
And yes, I now call grapefruit juice ‘the silent saboteur’. Thanks for the science-backed pep talk.
Carolyn Benson
December 20, 2025 AT 06:50 AMYou people treat lifestyle like it’s a magic wand. Meanwhile, I’m on 12 meds, can’t walk more than 10 minutes without passing out, and my ‘sleep schedule’ is whatever’s left after my kid’s seizures stop.
Stop glorifying wellness culture like it’s a moral obligation. Some of us are just surviving.
Dikshita Mehta
December 21, 2025 AT 01:23 AMI’m a nurse in Mumbai and I see this every day. Patients stop their BP meds because they think ‘eating less salt is enough’. Then they end up in ER.
But I also see people who combine meds with walking, sleep, and no grapefruit-side effects drop like a stone.
It’s not either/or. It’s both. And yes, doctors should ask more. They just don’t have time.
Alana Koerts
December 22, 2025 AT 08:11 AM37% reduction in nausea from steady carbs? Where’s the p-value?
And ‘22% faster metabolism with sleep’-which study? I read the whole thing and didn’t see a single citation for that number.
This reads like a sponsored blog post dressed as science.
Vicki Belcher
December 23, 2025 AT 01:01 AMI did ALL the things 🙌 Walked. Breathed. Cut grapefruit. Slept like a baby.
My doc reduced my antidepressant dose last month. I cried. Not because I was sad. Because I finally felt like ME again. 💖
Emily P
December 23, 2025 AT 05:15 AMSo if I sleep 8 hours and eat 30g carbs, does that mean I can drink 200ml grapefruit juice and still be fine? Or is it one of those ‘all or nothing’ things?
Just trying to understand the boundaries.
Aboobakar Muhammedali
December 23, 2025 AT 23:43 PMI tried the breathing thing and honestly it felt silly at first but now I do it without thinking. My dad who’s on blood pressure meds started doing it too. He said he stopped feeling dizzy after meals.
Small things matter man. Really.
Laura Hamill
December 25, 2025 AT 16:51 PMThis is all a distraction. Big Pharma doesn’t want you to know you can fix this with diet and sleep. That’s why they push more pills.
They make billions off side effects. The FDA is in their pocket.
Don’t be fooled. The real cure? Get off all meds. Go primal. Eat meat. Sleep in the dark.
They’ll call you crazy. That’s how they silence the truth.
Kinnaird Lynsey
December 27, 2025 AT 04:52 AMI appreciate the effort here. But I’m just gonna say this gently:
Some of us have chronic pain, autoimmune flares, or mental health days where ‘eat 30g carbs’ feels like climbing Everest.
Let’s not shame people for not being able to optimize their lives into a wellness influencer’s dream.
Small steps are still steps.
mark shortus
December 28, 2025 AT 23:06 PMI WAS THE ONE WHO DIDN’T BELIEVE THIS UNTIL I STARTED TRACKING MY SODIUM AND NOW I’M OFF ONE MEDICATION
MY DOCTOR SAID I’M A MIRACLE
MY KIDS SAID I’M NOT AS GRUMPY
MY CATS SEEM TO LIKE ME MORE
THIS ISN’T JUST HEALTH
THIS IS A REBIRTH
AND IF YOU’RE NOT DOING THIS YOU’RE JUST LETTING BIG PHARMA WIN
Janelle Moore
December 30, 2025 AT 00:28 AMWait… so if I sleep better and stop eating grapefruit… does that mean the government is hiding this from us? Why aren’t they broadcasting this on TV? Why do we still have to Google this? Something’s not right.