When someone is struggling with depression, taking pills every day can feel impossible-not because they don’t care, but because depression rewires motivation, memory, and even how the body feels pain. It’s not laziness. It’s biology. And it’s one of the most overlooked reasons people stop taking their medications, even when those meds are life-saving.
Depression Doesn’t Just Affect Mood-It Breaks Routine
Think about your own routine. You set an alarm for your blood pressure pill. You keep your insulin in the fridge. You refill your antidepressant before it runs out. Now imagine waking up with no energy, no focus, and a voice in your head saying, “What’s the point?” That’s what depression does to medication adherence. Studies show depressed patients are 2.3 times more likely to miss doses than those without depression, even after accounting for age, income, or other health problems. This isn’t just about forgetting. It’s about losing the mental bandwidth to manage complex routines. A person with heart failure might be told to take four different pills at different times of day. Depression makes that feel like climbing a mountain.Here’s What Non-Adherence Looks Like in Real Life
You won’t always hear someone say, “I stopped taking my meds because I’m depressed.” Instead, you’ll see patterns:- Missing doses for several days in a row, then suddenly taking two at once
- Running out of pills weeks before the next refill is due
- Saying, “I feel worse since I started this,” even when lab results show improvement
- Avoiding doctor visits or skipping follow-ups
Side Effects Feel Worse When You’re Depressed
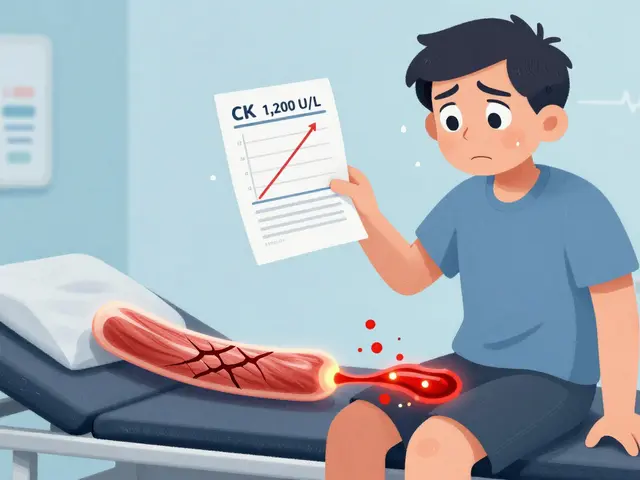
Depression doesn’t just make you tired. It makes every side effect feel heavier. A patient on an SSRI like sertraline might experience dry mouth, drowsiness, or loss of appetite. To someone feeling fine, these are minor inconveniences. To someone battling depression, they become proof the medication is “making things worse.” In Turkey, 83% of patients on SSRIs stopped taking them because of these effects. In Ethiopia, 57% stopped antidepressants due to weight gain, constipation, or insomnia. And here’s the twist: depression amplifies how you perceive side effects. The same nausea or headache that a non-depressed person might ignore becomes unbearable when you’re already feeling broken. One study found non-adherent patients reported significantly higher severity of side effects-even when doctors couldn’t find any new physical problems.Tools That Actually Work to Spot the Problem
You can’t guess who’s struggling. You need tools. The PHQ-9 is the most widely used depression screen. A score of 10 or higher means moderate to severe depression-and that’s the red zone for medication adherence. For every 5-point increase on the PHQ-9, adherence drops by about 23%. Pair that with the MMAS-8, which asks questions like:- “Do you ever forget to take your medicine?”
- “Have you ever stopped taking your medicine because you felt worse?”
- “Do you sometimes skip doses if you feel better?”

Early Warning Signs You Can’t Ignore
The first two weeks of treatment are critical. In the STAR*D trial, patients who missed more than 20% of their doses in the first 14 days were nearly five times more likely to have treatment fail completely. That’s not a coincidence. It’s a pattern. The brain needs consistency to respond to medication. One missed day here and there? Maybe not a big deal. But a string of missed doses? That’s the start of a downward spiral. That’s why clinics are now asking: “Did you take your pills yesterday? The day before?” Not just once a year. At every visit.What Happens When You Don’t Recognize the Link?
If you assume someone isn’t taking their meds because they’re “non-compliant,” you miss the real issue. A patient with heart failure who skips their beta-blocker because they’re too tired to remember? Their risk of hospitalization jumps. A diabetic who stops insulin because they feel hopeless? Their blood sugar spikes, leading to nerve damage, kidney problems, even amputations. Depression doesn’t just make people feel sad. It makes them more likely to die prematurely from preventable causes.How Clinicians Are Fixing This
The American Heart Association now recommends screening every heart failure patient for depression using a two-question screen (PHQ-2) at every visit. If it’s positive, they follow up with the full PHQ-9 and MMAS-8. In Spain, doctors started asking patients to keep a daily log: one column for depression symptoms, one for side effects. They found clear patterns-like when a patient’s mood dropped, their pill-taking dropped too. This simple “side effect mapping” helped patients and doctors adjust treatment before adherence collapsed. In Colombia, the MAPDep program trained both patients and doctors to track adherence together. The result? A 28.5% increase in consistent medication use after one year.What’s Next? Digital Tools Are Helping
New smartphone apps are now syncing mood tracking with pill reminders. One study found these apps predicted missed doses 72 hours in advance with 82% accuracy. That’s not science fiction. That’s happening now. And research is even looking at brain scans. Scientists at Icahn School of Medicine found that people with depression and poor adherence show less activity in the dorsolateral prefrontal cortex-the part of the brain responsible for planning and self-control. This isn’t just about willpower. It’s neurobiology.What You Can Do Right Now
If you’re taking medication and feeling down:- Don’t blame yourself. Depression isn’t weakness.
- Track your doses-even just a checkmark on your phone.
- Write down how you feel each day: mood, side effects, energy.
- Ask your doctor: “Could my depression be making it harder to take my meds?”
- Screen for depression at every visit-not just once.
- Use PHQ-9 and MMAS-8 together.
- Ask open questions: “What’s been hardest about taking your pills lately?”
- Don’t assume refusal. Assume difficulty.
It’s Not About Compliance-It’s About Connection
Medication adherence isn’t a test of discipline. It’s a test of support. Depression steals the ability to care for yourself. But with the right tools, the right questions, and the right empathy, that ability can come back. The data is clear. The tools exist. The solutions are simple-but not easy. They require us to look past the missed pill and see the person behind it.How do I know if depression is affecting my medication adherence?
Look for patterns: missing doses during low-mood episodes, stopping meds because you feel worse, or avoiding refills. Use the PHQ-9 (a 9-question depression screen) and MMAS-8 (an 8-question adherence tool). A PHQ-9 score of 10+ and an MMAS-8 score below 6 strongly suggest depression is interfering with your medication routine.
Can depression make side effects feel worse?
Yes. Depression lowers your tolerance for discomfort. A mild headache or dry mouth that someone else might ignore can feel overwhelming when you’re already emotionally drained. Studies show patients with depression report higher severity of side effects-even when clinical exams show no change in physical condition.
What’s the difference between forgetting and intentional non-adherence?
Forgetting is random-missing a pill once or twice. Intentional non-adherence is a decision: “I’m not taking this because it’s not helping” or “I feel worse on it.” Depression often drives intentional non-adherence. People don’t skip pills because they’re rebellious-they do it because they believe the meds are making their suffering worse.
Are there tools doctors use to measure adherence?
Yes. The MMAS-8 is the gold standard-it’s a short, validated questionnaire that scores adherence from 0 to 8. The PHQ-9 measures depression severity. Together, they’re far more accurate than either alone. Some clinics also use pill counts, electronic caps on pill bottles, or smartphone apps that log when doses are taken.
How can I improve adherence if I’m depressed?
Start small. Use a pill organizer. Set phone alarms. Write down how you feel each day alongside your doses. Talk to your doctor about adjusting medications if side effects are too harsh. And remember: it’s okay to ask for help. You don’t have to fix this alone. Support systems, therapy, and even a trusted friend checking in can make a huge difference.
Is this problem only for people with heart disease or depression?
No. Depression affects adherence across all chronic conditions: diabetes, HIV, epilepsy, asthma, and more. The link is universal. Any condition requiring daily medication is at risk when depression is present. It’s not about the disease-it’s about the mental state.
What’s the best way to talk to my doctor about this?
Say something like: “I’ve been struggling to take my meds consistently, and I think my mood might be part of it. Can we talk about how depression affects adherence?” Most doctors aren’t trained to ask this-but they’re trained to listen. Bringing it up opens the door to better care.




Joel Deang
December 3, 2025 AT 11:15 AMman i so get this 😔 i’ve been on antidepressants for 3 years and some days i just… forget. not because i dont care, but because my brain feels like it’s wrapped in cotton. then i take two the next day and feel like a failure. its not laziness. its my brain being broken. thanks for saying this.
Steve World Shopping
December 3, 2025 AT 13:13 PMFrom a clinical epidemiological standpoint, the conflation of behavioral non-adherence with neurobiological impairment is a critical diagnostic blind spot in primary care. The MMAS-8, while validated, lacks dynamic temporal resolution and fails to account for circadian dysregulation in depressive phenotypes. We must integrate neurocognitive biomarkers-particularly prefrontal cortex activation metrics-into adherence protocols to move beyond self-report bias.
Paul Keller
December 4, 2025 AT 00:59 AMThis is one of the most important pieces I’ve read in years. The idea that depression isn’t just a mood disorder but a cognitive and executive function disorder is still underappreciated in medicine. When patients miss doses, we label them non-compliant. But what if they’re not refusing treatment-they’re incapable of initiating it? That’s a neurological deficit, not a moral failing. We need to redesign healthcare around this reality, not punish people for having a brain that’s been hijacked by illness.
Shannara Jenkins
December 5, 2025 AT 10:48 AMThank you for writing this. I’ve been there. I used to feel so guilty for skipping my meds, like I was letting everyone down. But once I started tracking my mood and doses together, I saw the pattern-low mood = skipped pills. Now I use a pill box with alarms and tell my best friend to text me if I don’t check in. It’s not perfect, but it’s helping. You’re not alone.
Elizabeth Grace
December 6, 2025 AT 22:14 PMOMG YES. I stopped my SSRI because I thought it was making me more tired and emotional. Turns out I was just depressed. The meds were working. I just couldn’t tell the difference anymore. I cried for an hour when my therapist pointed that out. It’s not you-it’s the depression lying to you.
Steve Enck
December 7, 2025 AT 22:23 PMThe entire premise of this article is a dangerous anthropomorphization of biological dysfunction. To ascribe intentionality to a neurological deficit is to romanticize pathology. One does not ‘lose mental bandwidth’-one experiences executive dysfunction due to dysregulated serotonin and cortisol pathways. The solution is not empathy-it is pharmacological optimization and behavioral conditioning through operant reinforcement protocols. Compassion without clinical rigor is merely emotional theater.
Jay Everett
December 8, 2025 AT 12:21 PMBro this hit different 🙌 I used to think I was just lazy for not taking my meds. Then I read about the dorsolateral prefrontal cortex thing and was like… ohhh. So it’s not that I don’t care-it’s that my brain literally can’t plan ahead when I’m in a depressive episode. Now I use a dumb pill app that pings me + lets me log my mood. It’s not magic, but it’s the closest thing to a lifeline I’ve had in years. You’re not broken. Your brain’s just on vacation.
मनोज कुमार
December 8, 2025 AT 15:51 PMPHQ-9 MMAS-8 useless. People forget meds because they dont care. Depression is excuse. Take pills or dont. No need for apps or journals. Just do it. Simple.
Roger Leiton
December 9, 2025 AT 23:50 PMJust wanted to say I’ve been using the daily mood + pill tracker from the article and it’s been a game-changer. I didn’t realize how much my energy levels dropped right before I skipped a dose. Now I set a 7am alarm and a 7pm reminder. I still miss some, but I catch myself faster. Also-telling my doctor about the pattern made them switch my med. I feel 40% better. You’re not failing. You’re just fighting a silent war.
Laura Baur
December 10, 2025 AT 15:39 PMIt’s fascinating how society has pathologized non-adherence as a symptom of mental illness rather than a moral failing. The normalization of this behavior under the banner of ‘biological impairment’ erodes personal responsibility. If one’s neurochemistry excuses non-compliance, then what prevents the erosion of accountability across all domains of health? This isn’t compassion-it’s abdication of the very concept of self-discipline. The human spirit is not a passive recipient of neurotransmitter fluctuations. We are agents. Even in darkness, we must choose to rise.
Jack Dao
December 11, 2025 AT 22:27 PMEveryone’s just looking for an excuse now. I’ve been on 5 different meds for 12 years. I take them. Every. Single. Day. No apps. No journals. No therapy. Just discipline. If you can’t do that, maybe you’re not ready for the real world. Depression doesn’t make you special. It makes you weak. Stop using it as a crutch.