When your insurance pushes you to switch from a brand-name drug to a generic, you might see two options on the pharmacy counter: one labeled as an authorized generic and another as a regular generic. They both cost less than the brand, but are they the same? And more importantly - which one should you pick?
It’s not just about price. For some people, switching to the wrong kind of generic can mean a return of symptoms, new side effects, or even hospital visits. Others switch without a hitch and save hundreds a month. The difference comes down to one thing: formulation.
What exactly is an authorized generic?
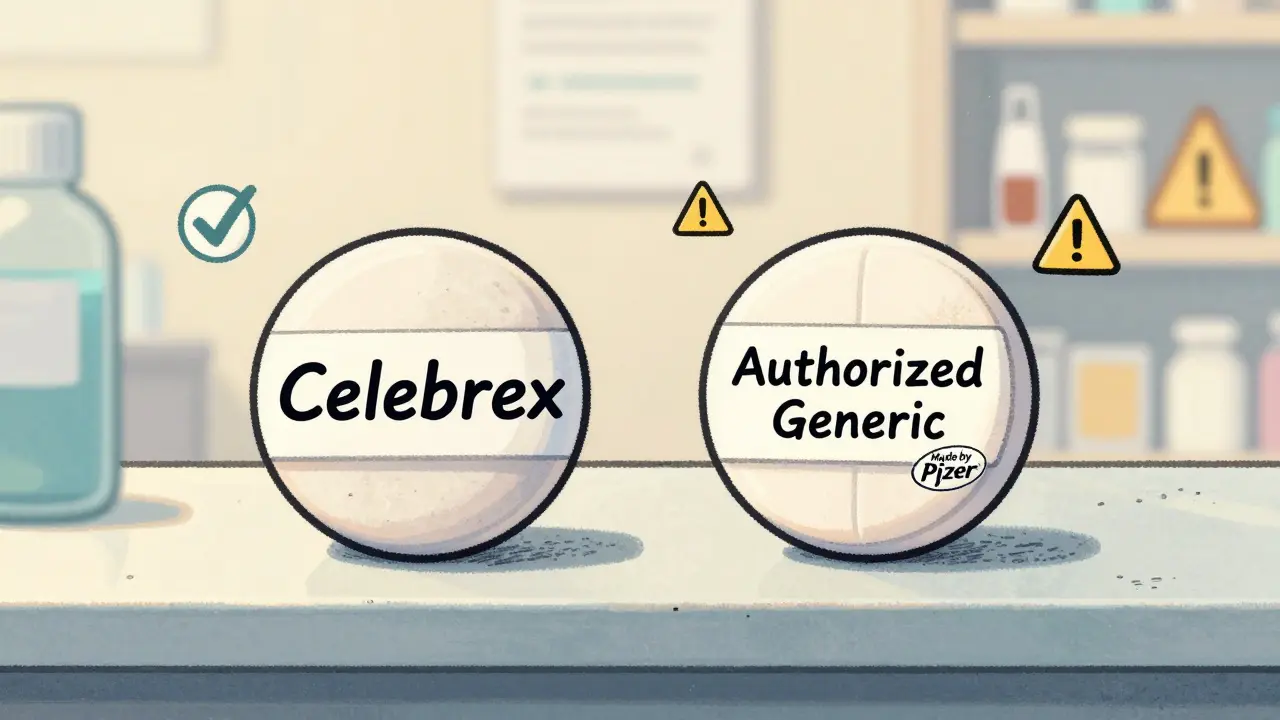
An authorized generic is the exact same pill, capsule, or injection as the brand-name drug - same active ingredient, same inactive ingredients, same manufacturing process, same factory. The only difference? It doesn’t have the brand name on the label.
For example, if you take Celebrex for arthritis, the authorized generic is made by Pfizer, the same company that makes Celebrex. It uses the same lactose, mannitol, and sodium stearyl fumarate. It’s the same batch, just repackaged without the brand logo.
The FDA defines it clearly: an authorized generic is a brand-name drug sold under a different label. It doesn’t go through the usual generic approval process. Instead, it’s produced under the original brand’s New Drug Application (NDA). That means no bioequivalence testing is needed - because it’s identical.
How is a regular generic different?
Regular generics, the kind you see most often, are made by different companies. They contain the same active ingredient, yes - but the fillers, binders, dyes, and coatings can vary. These are called inactive ingredients, and while they don’t treat your condition, they can affect how the drug is absorbed.
The FDA requires regular generics to be within 80-125% of the brand’s absorption rate. That’s a 25% window. Sounds broad? It is. For most drugs, it doesn’t matter. For others - like seizure meds, thyroid pills, or blood thinners - even small changes in how fast the drug enters your bloodstream can cause problems.
Take lamotrigine (Lamictal). A 2018 study in Neurology found that switching from brand to regular generic versions led to breakthrough seizures in some patients. The issue wasn’t the active ingredient - it was the different fillers changing how the drug dissolved in the gut.
Cost: Authorized vs Regular Generic
Price is where the trade-off gets real.
Regular generics usually cost 80-85% less than the brand. An authorized generic? It’s typically 10-30% cheaper than the brand - but 5-15% more expensive than the regular generic.
Take Concerta (methylphenidate ER). The brand costs around $210 for a 30-day supply. The regular generic? About $165. The authorized generic? $185.
That $20 difference matters if you’re paying out-of-pocket. But if you’re on Medicare or have high-deductible insurance, that $20 might be worth avoiding a trip to the ER.
A 2023 GoodRx survey of 5,000 users found that 18.7% had issues switching to regular generics - nausea, dizziness, reduced effectiveness. Only 6.2% had problems with authorized generics. The biggest complaint about authorized generics? They’re not cheap enough.
Who should consider an authorized generic?
Not everyone needs one. But if you’re taking a drug with a narrow therapeutic index - meaning the difference between a helpful dose and a dangerous one is small - you should pay attention.
Dr. Aaron Kesselheim from Harvard puts it simply: “For most drugs, regular generics are fine. But for thyroid meds, anti-seizure drugs, and immunosuppressants, the exact formulation matters.”
Here are the top 5 drug classes where authorized generics make the most sense:
- Antiepileptics (lamotrigine, phenytoin, carbamazepine)
- Thyroid hormones (levothyroxine)
- Blood thinners (warfarin)
- Immunosuppressants (cyclosporine, tacrolimus)
- Some ADHD meds (methylphenidate ER, dexmethylphenidate)
If you’ve ever felt “off” after switching generics - even if your doctor says it’s fine - try asking for the authorized version. Many patients report immediate improvements.
What about the data? Do studies back this up?
A 2018 study in the Journal of Managed Care & Specialty Pharmacy followed over 5,000 patients who switched from brand to generic. They compared those who got authorized generics versus regular generics.
The results? No meaningful difference in hospitalizations, ER visits, or how often people stopped taking their meds. Both groups had similar outcomes.
But here’s the catch: the study didn’t focus on high-risk drugs. When you look at just epilepsy or thyroid patients, the picture changes.
One Reddit user with epilepsy wrote: “Switched from brand Lamictal to a regular generic - two seizures in three weeks. Switched to the authorized generic - zero issues for 18 months.”
Another with high blood pressure said: “Switched from brand Lisinopril to a regular generic. My BP improved. Saved $400 a month.”
So yes - for most people, regular generics work fine. But for a subset of patients, the authorized version is the only safe choice.
How to tell them apart at the pharmacy
Most people can’t tell the difference just by looking. The labels look almost identical. The pill might even be the same color and shape.
Here’s how to know for sure:
- Ask the pharmacist: “Is this an authorized generic?”
- Check the National Drug Code (NDC) number on the bottle. Authorized generics share the same NDC prefix as the brand-name drug.
- Look up the manufacturer. If it’s the same company that makes the brand (e.g., Pfizer, Janssen, AbbVie), it’s likely an authorized generic.
- Use GoodRx’s Medication Switch Checker - it flags authorized generics and shows price comparisons.
A 2021 study found that nearly half of patients couldn’t tell the difference between the two types of generics just by looking at their prescription. That’s why asking is key.
What’s changing in 2026?
The FDA started requiring clearer labeling for authorized generics in January 2024. You’ll now see “Authorized Generic” printed on the bottle or box - not just hidden in fine print.
Medicare Part D plans are also required to tell you if an authorized generic is available for your drug. That means more people will know their options.
And the market is shifting. In 2022, only 5% of generics were authorized. By 2028, experts predict that number will rise to 12-15%, especially for complex drugs like inhalers, patches, and injectables where formulation matters even more.
What should you do next?
If you’re thinking about switching - or already switched and feel different - here’s your action plan:
- Check if your drug is on the high-risk list (thyroid, epilepsy, blood thinners, immunosuppressants).
- Call your pharmacy and ask: “Is the generic I’m getting an authorized generic?”
- If it’s not, ask your doctor to write “Dispense as Written” or “Do Not Substitute” on the prescription.
- If cost is a barrier, ask your doctor about prior authorization - some insurers will cover the authorized generic if you can prove a clinical need.
- Keep a symptom journal for two weeks after switching. Note changes in energy, mood, side effects, or how well your condition is controlled.
There’s no one-size-fits-all answer. But if you’ve had bad experiences with generics before, or you’re on a drug where small changes can cause big problems - don’t settle for the cheapest option. The authorized generic isn’t just a marketing trick. It’s a safety net.
Frequently Asked Questions
Are authorized generics just brand-name drugs with a different label?
Yes. An authorized generic is made by the same company that makes the brand-name drug, using the exact same ingredients and manufacturing process. The only difference is the label doesn’t carry the brand name. It’s not a copy - it’s the original product sold under a different name.
Why are authorized generics more expensive than regular generics?
Because they’re not made by a different company trying to undercut the market. Authorized generics are produced by the original brand manufacturer, so they don’t have the same cost-cutting pressure. Regular generics are made by competitors who can save money by using cheaper fillers or simpler packaging.
Can I switch from an authorized generic back to the brand name?
Yes, but it’s usually more expensive. If you’re doing well on an authorized generic, there’s rarely a medical reason to go back to the brand unless your insurance stops covering it. Most doctors will support staying on the authorized version - it’s the same drug, just cheaper.
Do pharmacists know the difference between authorized and regular generics?
Many don’t - especially if they’re busy. A 2021 study found that nearly half of patients couldn’t tell the difference, and pharmacists often assume patients don’t care. Always ask. Request the NDC number or the manufacturer name. Don’t assume the cheaper option is automatically the right one.
Is it safe to switch between different regular generics?
For most drugs, yes. But if you’re on a narrow therapeutic index medication - like levothyroxine or warfarin - switching between different generic versions can cause fluctuations in your blood levels. Some patients do fine. Others have serious issues. If you’re stable on one generic, don’t switch unless your doctor recommends it.




Joy Johnston
February 4, 2026 AT 01:48 AMJust wanted to add a practical tip: if you're on levothyroxine, always check the NDC code on the bottle. I switched from a regular generic to the authorized version (same manufacturer as Synthroid) and my TSH dropped from 6.8 to 1.9 in six weeks. No dose change-just the fillers. My endo was shocked. Seriously, for thyroid meds, it’s not a luxury-it’s a medical necessity.
Also, don’t let pharmacists push you to the cheapest option. They’re paid per prescription, not per outcome. Ask specifically for ‘authorized generic’-and if they look confused, ask for the manufacturer name. If it’s Janssen, Pfizer, or AbbVie? You’re good.
And yes, I’ve had patients cry when they finally got the right version after years of fatigue, weight gain, and brain fog. It’s not placebo. It’s chemistry.
Katherine Urbahn
February 4, 2026 AT 03:48 AMIt’s frankly irresponsible that insurance companies don’t automatically default to authorized generics for narrow-therapeutic-index drugs. The FDA has clear guidelines. The AMA has issued statements. Yet, we still let cost-cutting override clinical judgment. This isn’t about ‘saving money’-it’s about patient safety.
And let’s be clear: if your drug has a 25% absorption window, and you’re on warfarin or lamotrigine-you’re not ‘getting lucky.’ You’re gambling with your life.
Pharmacists need mandatory training on this. Insurance formularies need tiered restrictions. And patients? They need to be educated-not just told to ‘take the generic.’
This isn’t opinion. It’s evidence-based medicine.
Keith Harris
February 4, 2026 AT 17:57 PMOh please. You’re all acting like authorized generics are some magical elixir. I’ve been on generic Adderall for 8 years. Switched between 5 different manufacturers. Never had a problem. My ADHD is controlled. My job is fine. My wife says I’m not a zombie anymore.
Meanwhile, you people are spending $185 for a pill that’s functionally identical to the $165 one. It’s not ‘safety’-it’s brand loyalty masquerading as science.
And don’t even get me started on ‘symptom journals.’ Next you’ll be asking for astrology readings before refilling your meds.
Geri Rogers
February 5, 2026 AT 19:20 PMKeith, I hear you. But for some of us, the difference is night and day. I was on a regular generic for lamotrigine and started having micro-seizures-like, staring blankly for 3 seconds while making coffee. Scary stuff.
Switched to the authorized version? Zero issues. Zero. I didn’t even need a dose adjustment. My neurologist said, ‘You were in the 10% who are sensitive to fillers.’
It’s not about being paranoid. It’s about knowing your body. And if you’ve never had a bad experience? That’s great! But don’t tell others theirs aren’t real.
Also-emoji time 🙌❤️
Shelby Price
February 6, 2026 AT 21:28 PMWait… so if Pfizer makes both Celebrex and the authorized generic… why doesn’t the brand just drop the name and sell it cheaper? Like… why keep the brand at all?
Is it just to keep the marketing machine running? Or is there some weird patent loophole?
Also-how many people even know this exists? I’ve been on meds for 12 years and had no clue. 😅
pradnya paramita
February 7, 2026 AT 16:53 PMFrom an Indian pharmacy perspective: authorized generics are not widely distributed here due to regulatory fragmentation and lack of manufacturer partnerships. Most generics are produced under ANDA pathways with local excipients. Bioequivalence is tested, but dissolution profiles vary significantly due to humidity and temperature variances during storage.
For patients on narrow-therapeutic-index drugs, the risk of subtherapeutic exposure is elevated in tropical climates. Hence, in India, branded generics (not authorized) are often preferred despite cost-even if they’re not FDA-approved.
Recommendation: if you're outside the U.S., verify the manufacturer's origin. A 'Pfizer-made' pill imported from the U.S. is more reliable than a locally compounded generic with unknown excipient sourcing.
Jamillah Rodriguez
February 8, 2026 AT 05:02 AMSo… I switched to a regular generic for my blood pressure med… and now I’m dizzy? 😩
And my doctor says ‘it’s all in your head.’
Meanwhile, my cat is judging me.
Also-why does this feel like a cult? 😂
Harriot Rockey
February 9, 2026 AT 09:58 AMThank you for this. Seriously. I’ve been terrified to switch meds since my cousin had a seizure after a generic swap. I didn’t even know authorized generics existed.
Now I’m calling my pharmacist tomorrow. And I’m printing out that NDC chart. 📋✨
To everyone who’s been told they’re ‘overreacting’-you’re not. Your body knows. Trust it. And if you’ve had a good experience with regular generics? That’s awesome! But don’t erase others’ pain.
You’re not alone. 💛
Jesse Naidoo
February 10, 2026 AT 00:42 AMSo you’re saying if I’m on a generic for my antidepressant and I feel ‘off,’ it’s not depression coming back-it’s the lactose in the pill? 🤨
What if I just… ate a bag of chips? Would that fix it?
Also, why is everyone so obsessed with fillers? I’ve been on 7 different generics for citalopram. I’m fine. I don’t need a chemistry degree to take my meds.
…I’m just saying… maybe stop blaming the pill and start blaming the pillow.