Why Medications Can Fail on the Road
You packed your pills, grabbed your insulin pen, and hit the road-only to find your medication doesn’t work when you need it most. This isn’t rare. In fact, 41.3% of travelers report medication problems during trips, and more than two-thirds of those issues come from heat or cold exposure. A car glove compartment can hit 158°F (70°C) on a sunny day. Checked luggage can drop below freezing. Neither is safe for most medicines.
Medications aren’t just pills in a bottle. They’re complex chemicals that break down under extreme temperatures, light, or moisture. Insulin, thyroid meds, epinephrine auto-injectors, and even some antibiotics lose potency fast when exposed to heat above 86°F (30°C). A University of Michigan study found that meds kept above that temp for just two hours lost 37.2% of their effectiveness. That’s not a small risk-it’s life-threatening for people with diabetes, severe allergies, or heart conditions.
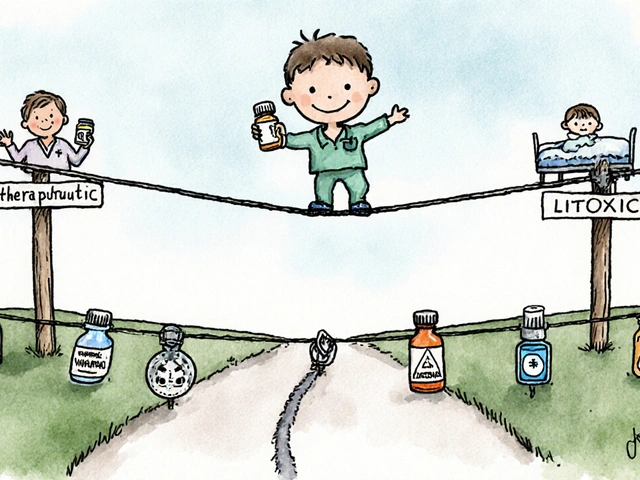
What You Need to Know About Temperature Rules
Most medications are designed to stay stable between 68-77°F (20-25°C). That’s room temperature. But about 12.7% of prescriptions-mostly biologics like insulin, injectables, and some migraine meds-need refrigeration: 36-46°F (2-8°C). This isn’t optional. It’s science.
Insulin is the most common example. If it gets too hot, it clumps. If it freezes, it loses its structure. Either way, it won’t lower your blood sugar. Frio Wallets and TempAid MedCoolers are two FDA-cleared options that keep insulin at safe temps for up to 72 hours without ice. They use phase-change materials that stay cool longer than regular gel packs. And yes, you need to freeze those packs for 12 hours at 0°F (-18°C) before use.
Don’t store meds in the car. Not in the glove box. Not in the trunk. Even on a 70°F day, a car’s interior can hit 110°F in minutes. One Reddit user shared how their insulin failed after being left in a trunk for three hours at 95°F. They ended up in the ER. That story isn’t unique.
Original Containers Are Non-Negotiable
Forget those pretty pill organizers. TSA and international customs require medications to be in their original pharmacy bottles. Why? Because they have the National Drug Code (NDC), your name, the doctor’s info, and exact dosage. If you transfer pills to a daily pill box, you risk being pulled aside at security-or worse, denied entry in another country.
TSA agents see hundreds of bags daily. If your meds aren’t labeled, they assume the worst. That means extra screening, delays, and sometimes confiscation. According to TSA data, secondary screening for unlabeled meds adds an average of 22.7 minutes per traveler. That’s a missed flight.
Pharmacists at Johns Hopkins Hospital say keeping meds in original containers cuts identification errors by 92.4% during emergencies abroad. If you’re hospitalized overseas and can’t prove what you’re taking, doctors can’t treat you safely. That’s not hypothetical. There are documented cases of travelers being given wrong meds because their pills weren’t labeled.
Liquid Meds and TSA Rules: What’s Allowed
The TSA’s 3-1-1 rule for liquids applies to meds too-but there’s a key exception. If you need more than 3.4 oz (100ml) of liquid medication, you can bring it in your carry-on. You just need to declare it. That means telling the agent at the checkpoint and having your prescription or doctor’s note ready.
Don’t rely on memory. Print out TSA Form TSA-1400 (Medical Notification Form) and fill it out ahead of time. It’s free and available on the TSA website. Some travelers skip this and get caught in long lines. Others carry a doctor’s letter on letterhead, which works even better. That letter should list your name, medication names, dosages, and why you need them. It’s required in 92 countries.
For insulin pens, syringes, or auto-injectors: you can bring unlimited supplies as long as they’re labeled. No need to put them in the plastic bag. Just have them ready to show. Same goes for nebulizers, inhalers, and liquid antibiotics.

Electronics, Batteries, and Air Travel
If you use an insulin pump, glucose monitor, or portable nebulizer, you’re dealing with electronics-and strict FAA rules. Each device can have a battery up to 100 watt-hours. Most pumps are under 20. But you still need to carry them in your carry-on. Checked bags get crushed, tossed, and exposed to extreme temps.
For insulin pumps, you may need FAA Form 8110-3 if asked. It’s not always required, but having it prevents delays. Some airlines ask for it anyway. The same goes for lithium batteries in glucose meters. Never pack them in checked luggage. Lithium fires have grounded flights. Don’t risk it.
Pro tip: Bring an extra battery. And don’t forget to pack your charger. Power outlets aren’t always available at layovers. A portable power bank (under 27,000mAh) is a smart addition.
Planning Ahead: The 14-Day Rule
Don’t wait until the night before to pack your meds. Start 14 days before departure. Why? Insurance rules. Medicare Part D and most private plans let you refill prescriptions up to 5 days early. That’s your window to get extra supplies in case of lost luggage or flight delays.
Ask your pharmacist for a travel pack. Many now offer it free. They’ll give you a small, labeled container with a 10- to 14-day supply, plus your original bottles for backup. That way, if your checked bag vanishes, you still have your meds.
Also, talk to your doctor about time zones. If you’re crossing more than three zones, your dosing schedule needs adjusting. For example, if you take a pill at 8 a.m. EST and fly to London (5 hours ahead), you can’t just take it at 8 a.m. local time. That’s 3 a.m. your body’s clock. The American Academy of Sleep Medicine recommends adjusting doses by 15 minutes per day over several days before travel to avoid disruption.
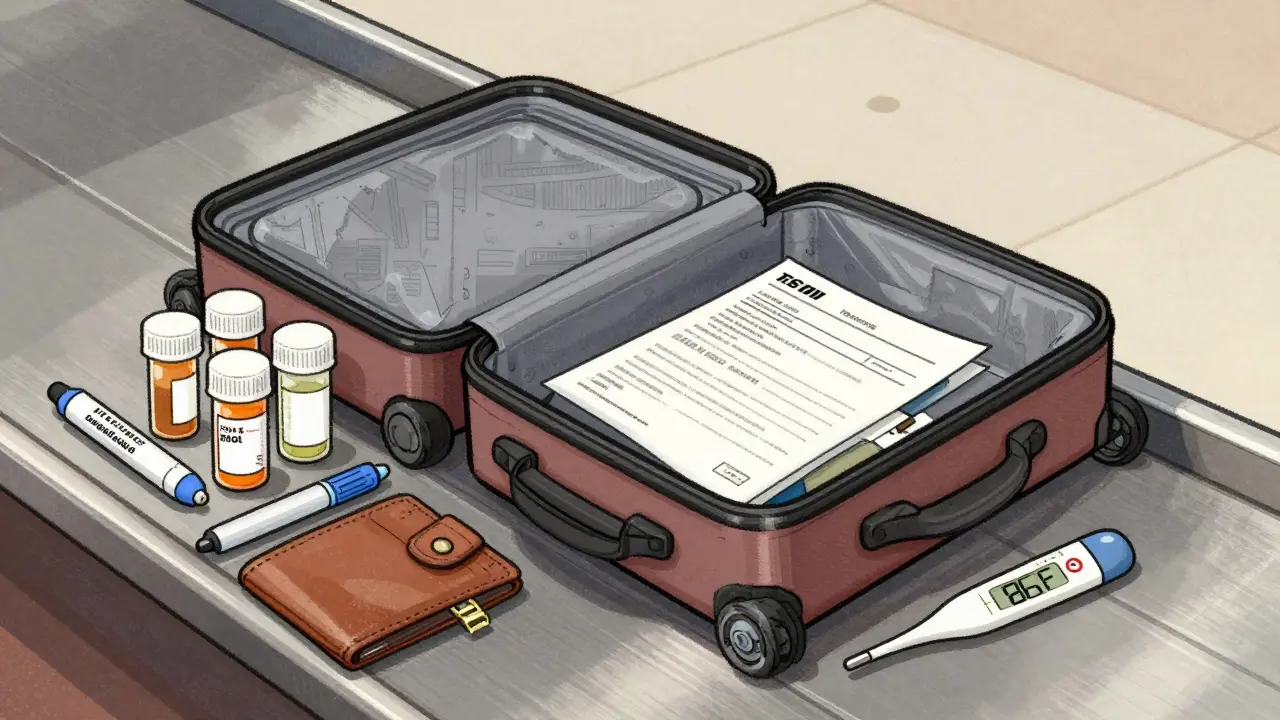
What to Pack in Your Carry-On
- Original bottles with labels (all meds)
- Extra 3-5 days of supply
- Doctor’s letter on official letterhead
- TSA Medical Notification Form (TSA-1400)
- Temperature-controlled cooler for refrigerated meds
- Insulin pens, syringes, or auto-injectors (with sharps container)
- Extra batteries for devices
- Portable power bank
- Printed copies of prescriptions
- Emergency contact info and medical ID
Leave the pill organizers at home. They’re convenient, but not safe. If you must use one, keep the original bottles in your carry-on as backup. Never rely on unlabeled pills alone.

What Happens When Things Go Wrong
Even with perfect planning, things can fail. A cooler breaks. Your bag gets lost. Your insulin freezes. Here’s what to do:
- Lost meds? Call your pharmacy. Many have international networks. Some can fax a prescription to a local pharmacy in your destination.
- Insulin failed? If you’re diabetic and your insulin is clumpy or cloudy, don’t use it. Go to the nearest hospital or clinic. They can provide emergency insulin.
- Epinephrine didn’t work? Call 911 or local emergency services immediately. A failed auto-injector is a medical emergency.
- Medication exposed to extreme heat? If you suspect degradation, stop using it. Get a replacement as soon as possible.
Report failures to the FDA’s MedWatch program. Your report helps improve safety for others. Use www.fda.gov/medwatch or call 1-800-FDA-1088.
What’s Changing in 2026
Technology is catching up. In 2023, the FDA approved temperature-indicating labels like 3M’s MonitorMark. These change color if your meds hit 86°F (30°C). By 2026, smart containers with Bluetooth sensors will hit the market. They’ll send alerts to your phone if temps go out of range.
Airlines are also upgrading. The FAA now requires temperature-controlled storage in aircraft galleys for medical items. Some international carriers already have dedicated cold bins for insulin and vaccines.
But until then, the rules haven’t changed: keep it cool, keep it labeled, keep it with you.
Final Checklist: Before You Leave
- ☑️ All meds in original bottles with labels
- ☑️ Extra 5-day supply packed
- ☑️ Doctor’s letter on letterhead
- ☑️ TSA Medical Notification Form ready
- ☑️ Refrigerated meds in validated cooler (pre-frozen for 12 hours)
- ☑️ Electronics in carry-on with extra batteries
- ☑️ No pill organizers used as primary storage
- ☑️ Prescription copies printed
- ☑️ Emergency contacts and medical ID accessible
Traveling with meds isn’t complicated. It just needs attention. One mistake can cost you your health. Follow these steps, and you won’t just survive your trip-you’ll stay in control.
Can I put my medications in checked luggage?
No, never. Checked luggage can be exposed to extreme temperatures, rough handling, and delays. Medications like insulin, epinephrine, and thyroid pills can become ineffective or dangerous. Always keep all medications in your carry-on. TSA and international health agencies require this for safety.
Do I need a doctor’s note to fly with medication?
You don’t always need one for U.S. flights, but it’s required in 92 countries. A doctor’s letter on official letterhead listing your medications, dosages, and medical necessity prevents delays at customs and helps if you need emergency care abroad. It’s also the best way to explain large quantities of liquid meds to TSA agents.
Can I use a pill organizer for travel?
Only as a secondary option. Never rely on a pill organizer alone. Pharmacists say transferring meds increases medication errors by 27.8% during travel because labels are lost. If you use one, always carry the original bottles in your carry-on as backup. Never pack unlabeled pills.
How do I keep insulin cool on a long flight?
Use an FDA-cleared travel cooler like a Frio Wallet or TempAid MedCooler. Freeze the gel packs for 12 hours at 0°F (-18°C) before your trip. Keep the cooler in your carry-on. Avoid putting it in overhead bins near vents. Some airlines allow you to store it in the galley fridge-ask the flight attendant before takeoff.
What if my medication is denied at customs?
Stay calm. Ask for the reason. Show your doctor’s letter and original prescriptions. If they still refuse, contact your country’s embassy or consulate. Many have lists of approved medications for travelers. Never force your way through. Some countries have strict drug laws-even common U.S. meds like Adderall or certain painkillers are illegal abroad.
Are there special rules for international flights?
Yes. The International Air Transport Association (IATA) and individual countries have their own rules. Some require translations of prescriptions. Others ban certain medications entirely. Check the International Association for Medical Assistance to Travellers (IAMAT) website for country-specific lists before you go. Always carry a doctor’s letter and keep meds in original containers.


Skye Kooyman
January 25, 2026 AT 14:25 PMI once left my insulin in the car for 2 hours at 90°F. Didn’t know any better. Ended up in the ER. Never again.
rasna saha
January 25, 2026 AT 21:52 PMThis is so important for travelers like me who rely on meds daily. I always carry my insulin in a Frio wallet and never let it out of my sight. Your post saved me from a bad mistake.
James Nicoll
January 27, 2026 AT 00:46 AMSo let me get this straight - we’re now treating our pills like fragile wine that needs a climate-controlled cellar? Next they’ll tell us to whisper sweet nothings to our antidepressants before boarding. 😏
Uche Okoro
January 27, 2026 AT 23:54 PMThe thermodynamic instability of biologics under non-isoergic thermal gradients is a well-documented pharmacokinetic vulnerability. The FDA’s 86°F threshold is not arbitrary-it’s derived from Arrhenius kinetics modeling of protein denaturation rates. You’re not just risking efficacy-you’re compromising molecular integrity.
Ashley Porter
January 29, 2026 AT 06:07 AMThe 3-1-1 exception for meds is a lifesaver. I always print the TSA-1400 and keep it with my prescriptions. No one’s ever questioned me since I started doing that.
Peter Sharplin
January 29, 2026 AT 16:42 PMI’m a nurse and I’ve seen too many people lose their meds to checked bags. One guy had his thyroid pills in his suitcase and got stuck in Dubai for 3 days. He went into myxedema coma. Don’t be that guy. Carry it. Always.
shivam utkresth
January 30, 2026 AT 14:40 PMIn India, we call this ‘desi wisdom’ - keep your medicine close like your chai. But honestly, this guide is next level. I’ve been using a TempAid for my dad’s insulin since last monsoon. No more panic at airport security. Also, never trust a pill organizer unless you’ve got the original bottle like your life depends on it - because it does.
John Wippler
January 31, 2026 AT 13:09 PMTraveling with meds isn’t about being paranoid. It’s about being prepared. Think of your pills as your personal bodyguards - they don’t work if they’re melted, frozen, or unlabeled. Treat them like your favorite pair of shoes: always carry them, never risk them, and always check the condition before you step out.
Kipper Pickens
February 1, 2026 AT 19:56 PMThe 2026 smart containers with Bluetooth temp sensors are going to be a game-changer. Imagine your phone pinging you if your insulin hits 87°F. That’s not sci-fi anymore - it’s logistics meeting pharmacology. The FAA’s galley cold bins are a step in the right direction, but the real win is consumer-grade tech catching up.
Aurelie L.
February 2, 2026 AT 09:28 AMI don’t trust any of this. My cousin took her pills in a Ziploc and flew to Spain. No problems. Stop scaring people.
Joanna Domżalska
February 3, 2026 AT 16:16 PMSo you’re telling me I can’t just dump all my pills into a pillbox because TSA says so? What next? Are we gonna need a notarized letter to carry Advil? This is overkill.
Faisal Mohamed
February 4, 2026 AT 02:47 AMBro. 🤝 I just got back from Bali. Used a Frio, kept my pump in my jacket, and had my doctor’s letter printed on nice paper. No issues. ✈️💊❄️ #TravelSmart #InsulinLife
Alexandra Enns
February 4, 2026 AT 20:10 PMThis is why Americans are so neurotic. In Canada, we just throw our meds in our suitcase and trust the universe. You think the world revolves around your insulin? Get over it.