Anti-Xa Test Indication Checker
Is Anti-Xa Testing Needed?
This tool helps determine if Anti-Xa testing is clinically indicated based on patient factors. According to guidelines, routine monitoring isn't recommended. Testing should only be performed when specific clinical triggers are present.
Select clinical factors and click "Check Indication" to see if testing is indicated.
Most people on low molecular weight heparin (LMWH) like enoxaparin or dalteparin never need an Anti-Xa test. It’s not a routine check like a blood pressure reading. But when something goes wrong-unexpected bleeding, a new blood clot, or strange lab results-that’s when Anti-Xa monitoring becomes critical. This isn’t about checking numbers for fun. It’s about catching dangerous imbalances before they cause harm.
Why Anti-Xa Monitoring Exists
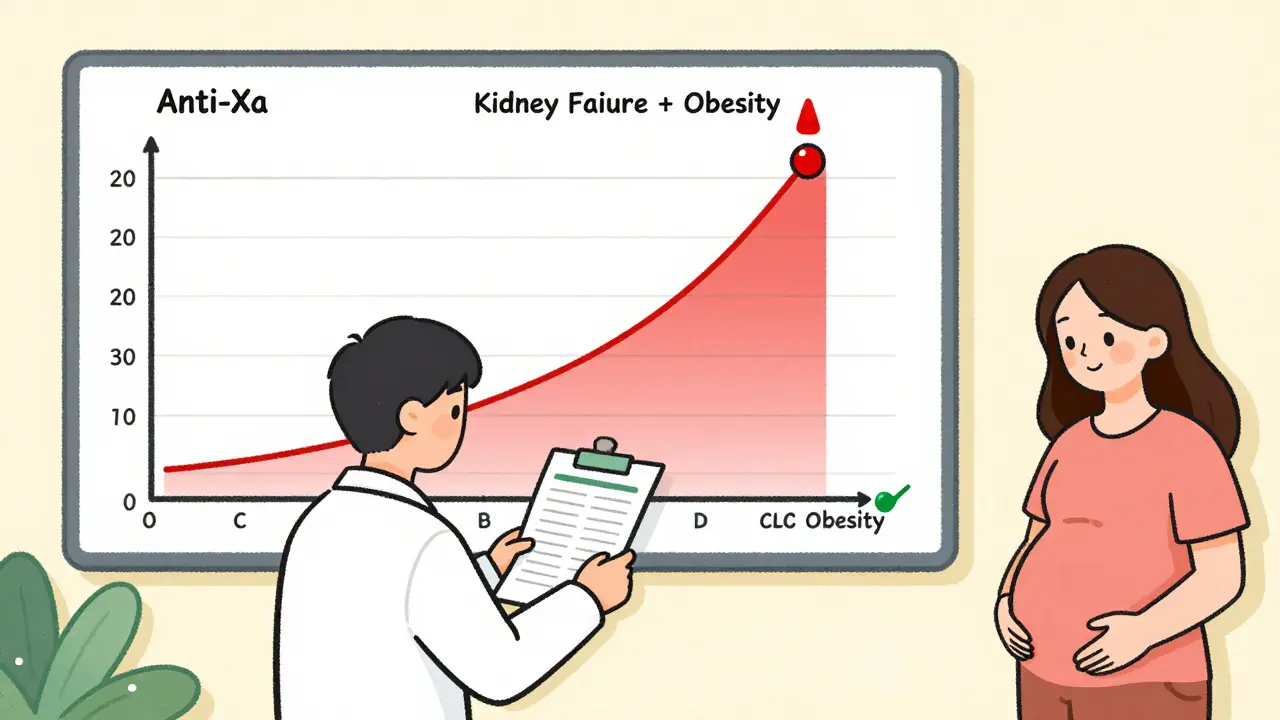
LMWH works by blocking factor Xa, a key player in blood clotting. Unlike unfractionated heparin, which needs frequent aPTT checks, LMWH was designed to be predictable. Dose based on weight, given once or twice daily, and usually safe without testing. That’s the theory. The reality? Some people’s bodies don’t follow the script. When kidneys aren’t working well, or someone weighs over 150 kg or under 40 kg, or they’re pregnant, LMWH sticks around longer or gets distributed differently. That means the drug builds up-or doesn’t build up enough. Anti-Xa testing measures exactly how much the drug is affecting clotting. It tells you if the level is too low (risk of clot) or too high (risk of bleeding).When You Actually Need the Test
Don’t order it because it’s day 3 post-op. Don’t check it just because the chart says "anticoagulation." Wait for a red flag. Here’s what triggers real testing:- Major bleeding with no clear cause-like a nosebleed that won’t stop, blood in urine, or unexplained bruising after starting LMWH.
- Thrombosis on therapy-a new DVT or PE despite being on a full therapeutic dose.
- Severe kidney impairment-creatinine clearance below 30 mL/min. Below 15 mL/min? Testing is strongly considered.
- Extreme body weight-over 150 kg or under 40 kg. Standard dosing may not work here.
- Pregnancy-especially third trimester. Target levels shift, and clearance changes.
- Suspected heparin-induced thrombocytopenia (HIT)-if switching from heparin to LMWH as a bridge, you need to confirm the dose is right.
A 2018 audit from Ventura County Medical Center found that only 28% of Anti-Xa tests ordered were actually justified. The rest? Routine checks after surgery, fear of liability, or misunderstanding guidelines. That’s not just wasteful-it’s dangerous. One in 12 inappropriate adjustments led to bleeding.
How the Test Works
The Anti-Xa test isn’t a simple blood draw. Timing matters. You need to draw the sample 4 to 6 hours after the injection-that’s the peak level. Drawing it right before the next dose (trough) doesn’t help much for LMWH. And you can’t test too early. The drug needs at least three doses to reach steady state.Target ranges depend on why you’re giving the drug:
- Prophylaxis (preventing clots): 0.2-0.5 IU/mL
- Therapeutic (treating clots): 0.6-1.0 IU/mL
- Pregnancy: 0.2-0.6 IU/mL (lower upper limit than non-pregnant)
Results come back in 2-4 hours in most hospitals. But here’s the catch: results vary between labs. One lab’s 0.8 IU/mL might be another’s 0.9. That’s why you don’t compare numbers across institutions. Always use your own lab’s reference range.
What the Test Can’t Do
Anti-Xa testing has limits. It won’t tell you if someone is going to bleed tomorrow. It doesn’t measure overall clotting risk. It can’t detect direct oral anticoagulants like apixaban or rivaroxaban. And it can’t tell you if the patient took the shot.Studies show that 41% of patients with a single supratherapeutic Anti-Xa level had no bleeding at all. That’s why you never adjust dose based on one number. You look at the whole picture: symptoms, kidney function, weight, recent surgery, other meds. A high level with no bruising? Maybe just a lab quirk. A high level with new gum bleeding? That’s a red flag.
Who Says What
The American College of Chest Physicians (ACCP) in their 2021 guidelines says clearly: don’t monitor routinely. Strong recommendation, Grade 1B. But they also say: consider it in those high-risk groups. Dr. Sam Schulman, who led a major 2015 meta-analysis, says monitoring obese patients isn’t usually needed-dosing by total body weight works fine. But Dr. Evan Lin from UC Davis says: “If a patient on LMWH has unexplained bleeding or clotting, you check the level. That’s not optional.” At Vanderbilt, they cut inappropriate testing by 63% by having pharmacists review every order before it’s done. At UW Medicine, they have a written algorithm: “Check Anti-Xa if CrCl <30, weight >150 kg, or unexpected clinical event.”The Cost and the Risk
Each test costs $45-$75. In the U.S., Medicare spends $28.7 million a year on unnecessary Anti-Xa tests. That’s money that could go to real care. But the bigger risk? Misinterpreting the test. A 2018 study showed that 72% of inappropriate dose changes made after Anti-Xa results led to harm-either bleeding or new clots. That’s not because the test is bad. It’s because people treat it like a dial instead of a clue.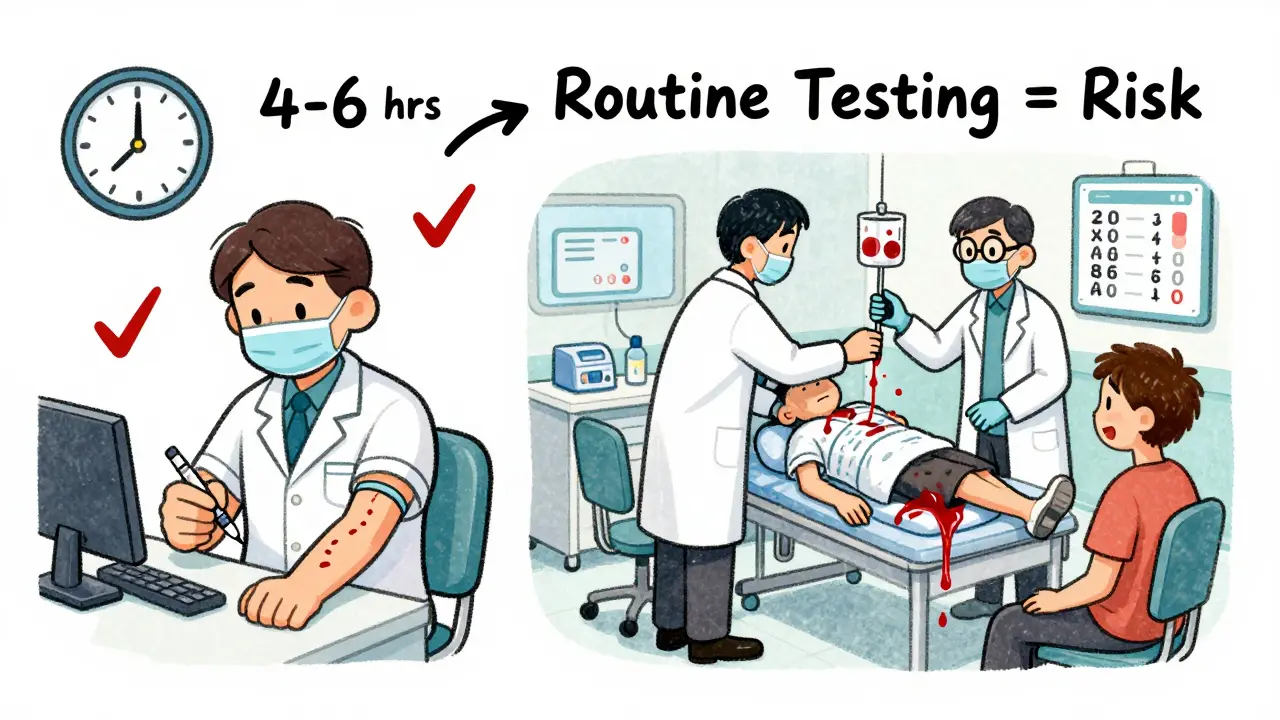
What to Do Next
If you’re on LMWH and you start bleeding for no reason, tell your doctor. If you develop a new leg swelling or chest pain, don’t wait. If you have kidney disease and are on LMWH, ask if your dose makes sense. Don’t ask for the test yourself unless there’s a clear reason. But if your provider orders it without a trigger, ask why. Is it because of your weight? Your kidneys? A recent bleed? Or just because they’ve always done it? The goal isn’t to hit a number. It’s to keep you safe. Anti-Xa monitoring is a tool for emergencies, not checklists. Use it right, and it saves lives. Use it wrong, and it hurts them.What Happens After the Test
If the level is too low and you’ve had a clot? The dose goes up. If it’s too high and you’re bleeding? The next dose is held. Sometimes, they switch to a different anticoagulant like argatroban or fondaparinux. But here’s the key: one test doesn’t dictate everything. You need to recheck after a dose change. You need to monitor for clinical signs. You need to know if your kidneys changed. You need to ask if you’re taking other drugs that affect kidney function-like NSAIDs or certain antibiotics. At academic hospitals, pharmacists work with doctors to make these calls. In smaller clinics? It’s often left to whoever is on call. That’s why guidelines matter. That’s why knowing the triggers matters.Looking Ahead
New point-of-care devices are being tested-machines that can give Anti-Xa results in under 30 minutes. That could change things in emergency rooms or ICUs. But even then, the rule stays the same: test only when the clinical picture demands it. The future isn’t more testing. It’s smarter testing. Targeted. Evidence-based. Patient-centered. The data is clear: routine monitoring adds no benefit. But in the right hands, at the right time, it’s life-saving.Do all patients on LMWH need Anti-Xa monitoring?
No. Most patients on LMWH don’t need it. Routine monitoring isn’t recommended by major guidelines. Anti-Xa testing is only needed when there’s a clinical reason-like unexpected bleeding, a new blood clot, severe kidney disease, extreme body weight, or pregnancy.
When should the blood be drawn for an Anti-Xa test?
The blood sample should be drawn 4 to 6 hours after the LMWH injection. This captures the peak level, which is what clinicians use to assess if the dose is correct. Drawing blood right before the next dose (trough) is not useful for therapeutic monitoring with LMWH.
What are the target Anti-Xa levels for LMWH?
For prophylactic dosing (preventing clots), the target is 0.2-0.5 IU/mL. For therapeutic dosing (treating clots), the target is 0.6-1.0 IU/mL. During pregnancy, the target range is narrower: 0.2-0.6 IU/mL. Always confirm the reference range with your specific lab.
Can Anti-Xa testing predict bleeding risk?
Not reliably on its own. A high Anti-Xa level doesn’t always mean bleeding will happen. Studies show that 41% of patients with supratherapeutic levels had no bleeding symptoms. Clinical signs-like new bruising, blood in urine, or low hemoglobin-are more important than the number alone.
Is Anti-Xa testing accurate across all labs?
No. There’s up to 15% variation between labs due to differences in equipment, reagents, and calibration. That’s why you should always use your own lab’s reference range and avoid comparing results from different institutions. Standardization efforts are underway, but it’s still a limitation.
What happens if the Anti-Xa level is too high?
If the level is high and the patient has signs of bleeding, the next dose is typically held. In severe cases, protamine sulfate can partially reverse LMWH, though it’s less effective than with unfractionated heparin. Sometimes, switching to a different anticoagulant is needed. Never adjust the dose based on one lab result-always correlate with clinical symptoms.
Can Anti-Xa testing be used for other blood thinners?
No. Anti-Xa testing is specific to heparins-both unfractionated and low molecular weight. It does not measure direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, or dabigatran. These require different tests, and often, no routine monitoring is needed.






Jane Lucas
December 28, 2025 AT 05:29 AMjust had my mom on lovenox after knee surgery and they tested her levels for no reason. she was fine. they lowered her dose and she got a clot. now she’s on warfarin and i hate it. why do they do this?
Olivia Goolsby
December 29, 2025 AT 20:59 PMLet me tell you something, because I’ve seen it with my own eyes-this whole Anti-Xa testing regime is a pharmaceutical-industrial complex scam. Labs make money off these tests, hospitals get reimbursed, and doctors cover their butts. The ACCP says don’t do it? That’s because they’re paid off by the DOAC manufacturers. Did you know that the same companies that make rivaroxaban also own half the lab equipment used for Anti-Xa? It’s not about safety-it’s about profit. And don’t even get me started on how they manipulate reference ranges to justify more testing. They’re not monitoring you-they’re monetizing your fear. Wake up.
Kishor Raibole
December 31, 2025 AT 12:55 PMIt is with profound respect for the clinical acumen displayed in this exposition that I feel compelled to offer a formal observation. The assertion that routine monitoring is unnecessary is, in my view, both scientifically sound and ethically prudent. However, the systemic failure to implement such guidelines with uniformity across institutions suggests a deeper pathology within the healthcare delivery paradigm-one characterized by defensive medicine, institutional inertia, and a lamentable absence of standardized protocols. I submit that the solution lies not in further testing, but in the institutionalization of pharmacist-led anticoagulation stewardship, as exemplified by Vanderbilt.
Elizabeth Alvarez
January 1, 2026 AT 22:05 PMThey’re lying to you. Anti-Xa tests don’t measure the drug-they measure what the government wants you to believe the drug is doing. The real danger? The heparin is laced with microchips. Not to track you-no, that’s the cover story. They’re using the blood samples to build a biometric database for the next phase of the vaccine program. That’s why they push testing so hard in hospitals. They need your blood to calibrate the nanobots. And don’t think pregnancy is safe-they’re targeting fetal development too. That’s why the target range is lower during pregnancy. It’s not for your safety. It’s for control. I’ve seen the leaked documents. They’re not testing for clots. They’re testing for compliance.
Miriam Piro
January 3, 2026 AT 13:53 PMLook. I get it. We’ve been conditioned to trust numbers. But here’s the truth: blood doesn’t lie, but labs do. And doctors? They’re just the middlemen in a system that turned healing into a spreadsheet. Anti-Xa levels? They’re a placebo for anxiety. You think a number between 0.6 and 1.0 makes you safe? Nah. Safety is in the breath you take when you wake up. It’s in the way your leg doesn’t swell. It’s in the silence between heartbeats. The test is a distraction. A shiny object to keep you from asking: Why am I on this drug in the first place? Who decided I needed it? Who profits when I bleed? We’re not patients-we’re data points in a machine that doesn’t care if you live or die. It just needs you to keep coming back.
dean du plessis
January 4, 2026 AT 18:00 PMBeen on LMWH for a year after a PE. Never had a test. No bleeding. No clots. Just take the shot, stay hydrated, move around. If something feels wrong, talk to your doc. Simple. No need to overthink it. The system makes it complicated so people feel like they need to do something. Sometimes the best thing is nothing.
Todd Scott
January 5, 2026 AT 03:51 AMAs someone who’s worked in anticoagulation clinics across three continents, I’ve seen this play out in rural India, urban South Africa, and suburban Ohio. The pattern is universal: when you have trained pharmacists reviewing orders, inappropriate testing drops by over 60%. The problem isn’t the test-it’s the lack of expertise. In the U.S., nurses and residents are expected to interpret Anti-Xa levels without training. In Nairobi, we have one pharmacist for every 200 patients, and they’re brilliant at triaging. The solution isn’t to abandon testing-it’s to invest in people who understand it. Knowledge beats algorithms every time.
Nikki Thames
January 5, 2026 AT 11:22 AMIt is deeply concerning that such a clinically nuanced topic is being reduced to a series of bullet points and colloquialisms. The notion that patients should 'ask why' if tested is not only patronizing-it is dangerously irresponsible. Anticoagulation is not a consumer choice. It is a high-risk therapeutic intervention that demands clinical authority. To suggest that laypersons should question physician judgment based on a blog post is to invite catastrophe. The guidelines exist for a reason: because people die when they do not follow them. And yes, sometimes that means testing-even if it feels unnecessary. Because in medicine, we do not wait for bleeding to occur before acting.
Chris Garcia
January 5, 2026 AT 11:22 AMLet me speak plainly: this is not about numbers on a screen. This is about dignity. In my village in Nigeria, we say: 'The hand that holds the needle must know the heart it serves.' LMWH is not a magic bullet-it is a sacred trust. When a woman carries life inside her, and her body shifts the drug’s path, who are we to say 'it’s fine'? When a man weighs 180kg and the machine says 'standard dose,' do we let him die because the algorithm doesn’t see him? The test is not the enemy. The arrogance of one-size-fits-all medicine is. We must honor the human variable. Not because it’s convenient. But because it’s holy.
James Bowers
January 6, 2026 AT 10:45 AMIt is the opinion of this reviewer that the assertion that Anti-Xa monitoring is unnecessary in the majority of cases is both statistically accurate and clinically prudent. However, the dissemination of this information through informal, colloquial media channels risks undermining the professional integrity of clinical decision-making. The absence of formal citations, the use of emotive language, and the lack of structured guidance may lead to inappropriate patient self-advocacy, resulting in deleterious outcomes. It is recommended that such content be restricted to peer-reviewed journals and institutional training modules.
Janice Holmes
January 8, 2026 AT 09:40 AMTHEY’RE LYING TO YOU. EVERY SINGLE ONE OF THEM. Anti-Xa tests? They’re just the tip of the iceberg. The real reason they want you tested? So they can track your blood chemistry for the next phase of the bio-surveillance program. You think they don’t know how you metabolize drugs? They’ve been building a database since 2012. Every test. Every dose. Every bruise. They’re mapping your body to predict your future. And if your level’s off? They don’t adjust your dose-they flag you. For insurance. For employment. For the next pandemic. You think this is medicine? No. This is control. And they’re using your fear to make it stick.