Every year, millions of people in the U.S. avoid medications they think they’re allergic to-only to find out later they never had an allergy at all. It’s not just a personal inconvenience. Mislabeling a side effect as an allergy can lead to worse treatments, longer hospital stays, and even life-threatening infections. The truth is, drug allergies and side effects are completely different-and knowing the difference could save your life.
What Exactly Is a Drug Allergy?
A drug allergy isn’t just feeling sick after taking a pill. It’s your immune system going into overdrive, treating a medication like a dangerous invader. When this happens, your body produces antibodies-usually IgE-that trigger a flood of chemicals like histamine. That’s what causes symptoms like hives, swelling, trouble breathing, or even anaphylaxis, which can be fatal if not treated fast. The most common culprit? Penicillin. About 80% of all documented drug allergies involve penicillin or related antibiotics like amoxicillin. But here’s the twist: studies show that up to 95% of people who say they’re allergic to penicillin can actually take it safely. Why? Because most of them never had an allergy to begin with. True drug allergies follow a pattern. They usually show up quickly-within minutes to an hour after taking the drug. That’s the hallmark of IgE-mediated reactions. But some allergic reactions are slower. A rash that appears 10 days after starting a new antibiotic? That’s often T-cell mediated, like DRESS syndrome. It’s rare, but dangerous: about 1 in 10 people with DRESS don’t survive.What Are Side Effects, Really?
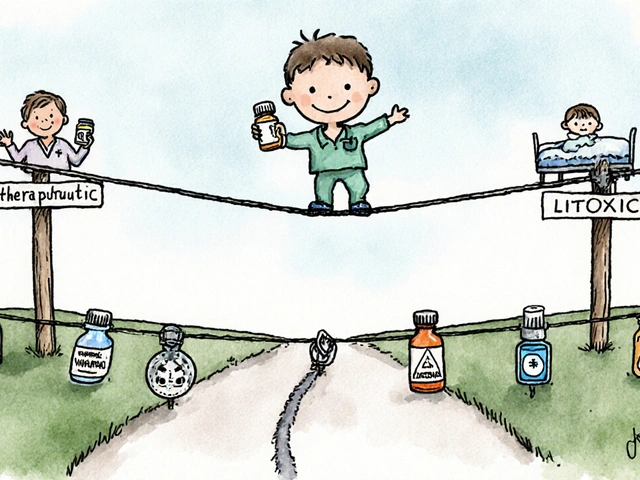
Side effects are the body’s predictable response to how a drug works-not an immune reaction. Think of them as the unintended side of a drug’s main job. For example, ACE inhibitors lower blood pressure by blocking a chemical called angiotensin. But that same blockage causes a dry cough in 5-20% of users. That’s not an allergy. It’s a direct result of the drug’s mechanism. Statins? They can cause muscle aches in 5-10% of people because they interfere with muscle cell energy production. Metformin? It often causes diarrhea because it changes how your gut absorbs sugar. These aren’t rare surprises. They’re well-known, documented, and often manageable. Timing matters. Side effects usually show up within the first few days of starting a drug. And here’s the key difference: they often get better with time. If you take an antibiotic and feel nauseous for the first two days but then feel fine, that’s likely a side effect-not an allergy. Allergies don’t fade with continued use. They get worse.How to Tell the Difference: A Simple Guide
Here’s how to spot the difference in real life:- Itchy rash? If it’s raised, red, and spreading fast-especially with swelling of the lips or tongue-it’s likely an allergy.
- Stomach upset? Nausea, vomiting, or diarrhea within 24-72 hours? Probably a side effect.
- Shortness of breath? If it happens right after taking the drug and you feel like you can’t breathe, treat it like an emergency. That’s anaphylaxis.
- Low-grade fever and rash after a week? Could be DRESS or another delayed reaction. Needs medical evaluation.
- Headache or dizziness? Common with blood pressure meds. Almost never an allergy.
Why This Mistake Costs Lives (and Money)
When doctors think you’re allergic to penicillin, they often reach for stronger, broader antibiotics like vancomycin or clindamycin. But these drugs aren’t better-they’re riskier. Patients labeled with penicillin allergy are 2.5 times more likely to get a C. diff infection, a severe and sometimes deadly gut infection caused by antibiotic overuse. The financial hit is real, too. A single hospitalization for someone with a mislabeled penicillin allergy costs about $1,000 more than for someone who can take the right drug. Multiply that across millions of patients, and it adds up to over $1 billion a year in the U.S. alone. And here’s the worst part: many of these labels stick for decades. People are told they’re allergic as kids after a rash during a viral infection-then they live with that label for life. But research shows that 90% of those labels are wrong. A simple test can clear it up.Testing and Diagnosis: What Actually Works
If you think you have a drug allergy, don’t assume. Get it checked. For penicillin, the gold standard is skin testing. A specialist puts tiny amounts of penicillin under your skin and watches for a reaction. If it’s negative, you’re almost certainly not allergic-97-99% accurate. If skin testing isn’t available or inconclusive, a supervised oral challenge might be done. You take a small, gradually increasing dose of the drug under medical supervision. Over 95% of low-risk patients pass without issue. But here’s the catch: most primary care doctors can’t tell the difference. One study found they correctly identify allergies only 42% of the time. That’s why hospitals with pharmacist-led allergy clinics are seeing an 80% drop in unnecessary penicillin avoidance. The fix? Better documentation. Instead of writing “penicillin allergy” in your chart, write: “Rash 10 days after amoxicillin, no swelling or breathing trouble.” That tells the doctor it’s likely not an allergy.
What You Can Do Right Now
You don’t need to wait for a doctor’s appointment to start making smarter choices.- Write down exactly what happened: when the reaction occurred, what symptoms you had, and how long they lasted.
- Ask yourself: Did I have a fever or another infection at the time? Many rashes during illness are mistaken for drug allergies.
- Check your records. If your chart just says “allergic to penicillin,” ask your doctor for a referral to an allergist.
- If you’ve never been tested, you’re probably not allergic. Don’t let a childhood label limit your treatment options.
The Bigger Picture: Why This Matters
This isn’t just about avoiding rashes or stomach upset. It’s about antibiotic resistance. Every time we use a broad-spectrum drug because someone was mislabeled, we push bacteria to evolve. That makes infections harder to treat for everyone. It’s also about access. If you’re told you’re allergic to sulfa drugs, you might be denied the best treatment for a UTI. If you’re labeled allergic to NSAIDs, you might miss out on pain relief that works better than opioids. New guidelines from the FDA now require drug labels to clearly separate allergy warnings from side effect lists. By 2027, most U.S. hospitals will have automated alerts in their systems that flag when a patient’s allergy label might be outdated. The message is clear: if you’ve ever been told you’re allergic to a drug, you owe it to yourself to find out if it’s true. You might be carrying around a label that’s holding you back-without even knowing it.Real Stories, Real Impact
One woman in Colorado avoided penicillin for 25 years after a mild rash as a child. When she needed antibiotics for a severe infection, her doctor had to use a more expensive, less effective drug. She finally got tested-turns out she was never allergic. She got the right treatment, recovered faster, and saved over $4,000 in extra costs. Another patient thought she was allergic to ibuprofen because she got a headache after taking it. Turns out, she was dehydrated. The headache had nothing to do with the drug. She spent years in pain, avoiding even low-dose pain relief, until a pharmacist asked the right question. These aren’t rare cases. They’re the norm.Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy as children lose it within 10 years, even without testing. But you shouldn’t assume it’s gone. The only way to know for sure is through proper evaluation by an allergist.
Is a rash always a sign of drug allergy?
No. Many rashes happen during viral infections-especially in kids-and are wrongly blamed on antibiotics like amoxicillin. In fact, up to 90% of rashes labeled as penicillin allergy in children are actually caused by the virus, not the drug. Always check with a specialist before assuming it’s an allergy.
Can side effects be dangerous?
Absolutely. Side effects like kidney injury from NSAIDs, liver damage from acetaminophen, or muscle breakdown from statins can be serious. But they’re not allergies. They’re toxic effects from the drug’s chemistry. If you experience severe symptoms-dark urine, yellow skin, extreme muscle pain-stop the drug and get help immediately. But don’t label it an allergy unless an immune response is confirmed.
What should I do if I think I have a drug allergy?
Don’t just stop the drug and assume the worst. Write down the details: what you took, when, and exactly what happened. Then talk to your doctor or pharmacist. Ask if you should be referred to an allergist for testing. Many insurance plans cover allergy evaluations, especially for penicillin.
Are there tests for all drug allergies?
No. Skin tests and blood tests exist only for a few drugs, mostly penicillin and some other antibiotics. For most other medications, diagnosis relies on your history and, if needed, a supervised challenge. That’s why accurate reporting of symptoms is so important-it’s the best tool doctors have.
If you’ve been avoiding a medication because you think you’re allergic, it’s time to ask: was it really an allergy-or just a side effect? The answer could open up better treatments, lower costs, and safer care. Don’t let an old label decide your health future.





John Hay
December 22, 2025 AT 11:46 AMPeople keep calling rashes allergies like it's a diagnosis you get from a Google search. I had a rash after amoxicillin at 7, got labeled allergic, and spent 20 years avoiding penicillin. Got tested last year-negative. Turned out it was a virus. Same thing happens to half the kids on antibiotics. Stop assuming. Get tested.
Stacey Smith
December 23, 2025 AT 06:22 AMThis is why American healthcare is broken. You get misdiagnosed as a kid and it follows you forever. No one checks. No one cares. Just slap on 'allergy' and move on. We need mandatory retesting at 25. It's not optional.
Ben Warren
December 24, 2025 AT 00:28 AMIt is, without question, a profound failure of primary care infrastructure that immunological literacy remains so rudimentary among general practitioners. The conflation of pharmacodynamic adverse effects with IgE-mediated hypersensitivity represents a systemic epistemological error, one that perpetuates therapeutic suboptimization and contributes to the broader antimicrobial resistance crisis. The data is unequivocal: 95% of penicillin allergy labels are erroneous. Yet, the medical record persists as a dogma, unchallenged, unverified, and tragically uncorrected. This is not merely a clinical oversight-it is a public health catastrophe.
Teya Derksen Friesen
December 25, 2025 AT 08:31 AMIt's fascinating how we've normalized medical mislabeling as a cultural norm. In Canada, we've started pilot programs where pharmacists conduct structured allergy reviews during routine script fills. It's not about blame-it's about precision. One simple question: 'Did you have a fever?' can change everything. We're moving toward evidence, not assumption.
Sandy Crux
December 25, 2025 AT 18:40 PM...and yet, nobody mentions that the FDA’s new labeling requirements are being quietly watered down by pharmaceutical lobbying... the 'automated alerts' by 2027? Please. The same companies that profit from broad-spectrum antibiotics are the ones funding the guidelines. You think they want you to use penicillin? They want you on vancomycin. Always.
Hannah Taylor
December 27, 2025 AT 09:49 AMthey say penicillin allergies are fake but what if its a trick? what if big pharma is putting something in the pills to make you sick so you gotta buy their other drugs?? i got a rash once and now i dont trust anything. they control the tests too.
Jason Silva
December 29, 2025 AT 03:47 AMBro this is wild 😳 I thought I was allergic to ibuprofen because I got a headache once... turned out I was dehydrated. Now I take it like candy 🤯 If you think you're allergic, get tested. Don't let fear hold you back. #DrugAllergyMythBusted
Theo Newbold
December 29, 2025 AT 08:03 AMLet's not romanticize the 'simple test' narrative. Skin testing for penicillin has a 3% false negative rate. And what about non-penicillin allergies? No tests exist for 90% of drugs. You're not 'cured' by a negative test-you're just temporarily cleared. The system is designed to keep you guessing.
Cara C
December 30, 2025 AT 03:56 AMMy mom was told she was allergic to sulfa drugs after a rash in her 20s. She avoided them for 40 years. Last year, she got a UTI and the only effective antibiotic was sulfa-based. She did the challenge under supervision-zero reaction. She cried. Not because she was scared-but because she realized she’d been in pain unnecessarily for decades. You’re not being dramatic. You’re being brave if you ask for a test.
Michael Ochieng
December 30, 2025 AT 11:17 AMI'm from Kenya-we don't have allergists in most towns. But we have community health workers who ask: 'Did you have a fever?' and 'Was it itchy or flat?' That’s it. That’s all you need to start questioning the label. You don't need a fancy test to be smart about your health. Just ask the right questions. And if you’re the parent? Don’t let your kid’s rash become their lifelong restriction.