Dizziness that just won’t quit can make everyday life a hassle—even the basics like walking to the bathroom start to feel like Olympic-level events. For folks told to try vestibular rehabilitation, doctors sometimes add betahistine into the mix. But does that little pill really help you steady your world? That’s what most people want to know.
First off, betahistine isn’t some miracle fix. It's actually been around since the 1970s and is best known for treating Ménière’s disease, a condition that turns your world upside down with spinning vertigo attacks. But more and more, doctors are using it for all sorts of dizzy spells—especially when paired with vestibular rehab.
The big draw is that betahistine may improve blood flow in your inner ear, which seems to help with symptoms like spinning and ear fullness. It doesn't “cure” the reason you’re dizzy, but it might take the edge off enough that you can push through those not-so-fun rehab exercises. That means you get more out of each session—sort of like taking painkillers before doing physical therapy for a sore knee.
Still, there are a lot of mixed opinions. Some research says betahistine can cut down dizzy days and make rehab exercises more tolerable, while other studies see little to no difference compared to a sugar pill. Bottom line: the combo probably works best for folks with major symptoms who keep skipping rehab because they feel too lousy to even try.
- How Betahistine Works in the Body
- Vestibular Rehabilitation Basics
- Combining Betahistine with Vestibular Rehab
- Real-World Tips and Common Questions
How Betahistine Works in the Body
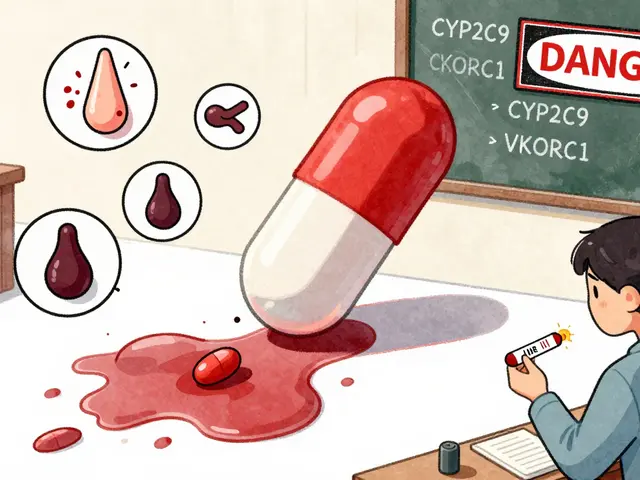
When you pop a betahistine tablet, it mainly targets the inner ear. This is the part of your body that handles balance and senses motion, so when it's not working right, you feel shaky or dizzy. Betahistine is thought to tweak certain receptors—specifically, histamine H1 and H3 receptors. In simple terms, it boosts blood flow around your inner ear and brain, which may help clear out built-up fluids and relieve that weird spinning sensation.
Most folks take betahistine for conditions like vertigo and dizziness, especially if they have problems like Ménière’s disease. Doctors often dose it at 16 to 24 mg, two or three times a day. It doesn’t knock you out or make you hyper; if anything, most people say they barely feel it, other than a slight relief from that constant off-balance feeling.
What’s also interesting is that betahistine has a pretty low rate of side effects. A few people might deal with a headache or mild tummy ache. Here’s a quick look at what happens after you take it:
- It widens blood vessels in the inner ear (better blood means less pressure).
- It speeds up how fast fluid leaves that area, helping clear up muffled hearing and fullness.
- It might help your brain relearn how to balance, so those vestibular rehabilitation exercises feel easier over time.
Still, no drug works the same for everyone. Some people notice a difference right away, while others need a few weeks to feel any change. Real talk: if your doctor suggested betahistine, they’re aiming to make symptoms less in-your-face so you can stick with your rehab plan. If you’re not sure it’s working after a month, let your doctor know.
| Effect | What Betahistine Does |
|---|---|
| Balance Improvement | Speeds fluid out of the inner ear, reducing pressure |
| Dizziness Control | Boosts inner ear blood flow, may ease vertigo |
| Side Effects | Mild headache, stomach upset (rare) |
Vestibular Rehabilitation Basics
People hear the words “vestibular rehabilitation” and picture a fancy clinic, but in reality, it’s a down-to-earth approach. It’s a set of exercises made to help your brain and body adjust so dizziness and balance issues aren’t running your life. Most often, physical therapists guide you through it. The main goal? Train your brain to make sense of weird signals from your inner ear and get you steady on your feet again.
Rehab treats all kinds of dizzy problems, like vertigo, Ménière’s disease, and plain old unexplained imbalance. It doesn’t matter if your dizziness started after an infection, a fall, or just randomly—these exercises have your back.
- Gaze stabilization: You focus on an object while moving your head. Sounds simple, but with vertigo, this can feel like a ride at the carnival. It trains your eyes and inner ear to work together better.
- Balance training: You’ll do things like stand on one leg, walk heel-to-toe, or stand on different surfaces to mess with your balance just enough to force your brain to compensate.
- Habituation: If certain movements trigger dizziness, you repeat those in a controlled way until your system learns to chill out and stop freaking over every head turn.
A lot of people want a shortcut, but honestly, vestibular rehab works best when done right—and it’s proven. For example, studies from universities in the U.S. say about 75% of patients notice real improvement after a couple of months, especially if they do the exercises at home, not just in therapy.
| Type of Dizziness | Success with Rehab (%) |
|---|---|
| Benign Paroxysmal Positional Vertigo (BPPV) | 85% |
| Mild Vestibular Migraine | 60% |
| Chronic Unilateral Vestibular Loss | 70% |
The stuff isn’t one-size-fits-all, so therapists customize plans for each person. That way, you’re not wasting time on exercises that won’t help. The secret sauce is sticking with it: a few minutes every day, and you’ll likely notice that dizzy days aren’t dominating your schedule anymore.

Combining Betahistine with Vestibular Rehab
Pairing betahistine with vestibular rehabilitation has become a go-to plan for people stuck in a loop of spinning rooms and unsteady steps. This combo really aims to help you get the most out of your exercises by making dizzy episodes less disruptive, especially early on, when everything just feels too wobbly to manage without some backup.
Here’s the simple logic: rehab exercises work best if you can actually do them. But those with severe dizziness sometimes skip or cut corners because they feel too rotten. By easing symptoms, betahistine might give you just enough relief to stick with your program consistently. A review of studies from 2023 pointed out that people using both approaches reported better quality of life and fewer drop-outs compared to those trying rehab alone.
| Approach | Drop-out Rate | Improvement in Balance |
|---|---|---|
| Rehab only | 30% | Moderate |
| Rehab + Betahistine | 18% | Good |
Here’s what most doctors recommend when combining both:
- Start betahistine a few days before your first rehab session. This gives your body time to adjust and lets you feel a difference by your first round of exercises.
- Stick with your prescribed rehab routine—don’t slack off just because you feel a bit better. The exercises rebuild confidence in your balance system.
- Watch for side effects. Most people tolerate betahistine fine, but keep an eye out for headaches, upset stomach or rashes. Call your doc if anything feels off.
- Update your rehab therapist on how you’re feeling—both good and bad. They can tweak your exercises or your medication routine so you get the most out of both.
One cool tip: some people find they’re more motivated to stick to vestibular rehabilitation when they don’t have to dread the worst spinning attacks. So the combo isn’t just about physical results—getting your confidence back helps you bounce back faster, too.
Real-World Tips and Common Questions
People using betahistine for vertigo always ask: How do I know it’s working? Will I need it forever? Let’s get into some smart tips, honest answers, and what usually happens for most folks juggling vestibular rehabilitation and medication.
If you’re just starting betahistine, most doctors recommend staying consistent with the timing each day. For best results, take it with food to cut down on stomach upset—it’s not uncommon for people to feel some heartburn or headache early on. These usually fade after a few days, but if you notice wheezing, serious rash, or feel faint, get checked out right away. Those are rare side effects, but worth knowing.
Now, don’t expect overnight changes. Most benefits (less spinning, steadier steps) show up after 2–4 weeks. That’s just being real—there’s no instant switch, and tracking your symptoms with a diary can help spot improvements you might miss while you’re in the middle of it all.
- Work with your therapist: Share when you feel worse or better. They might adjust your exercises if needed.
- Stay hydrated: Dizziness can get worse if you’re even a little dehydrated.
- Don’t skip sessions: Consistency with rehab is what rewires your balance system.
- Avoid driving until you’re steady: Nobody wants to risk a fender-bender mid-spin.
- Ask about meds that clash: Some allergy pills and antidepressants can mess with betahistine.
Worried about taking betahistine for too long? Most folks only use it for a few months—long enough to help them stick with rehab until the real improvement sets in. After that, many can stop taking it altogether without the dizziness coming back. Don’t stop suddenly though; talk with your doctor about tapering off if you’ve been on it for a while.
| Common Questions | Short Answers |
|---|---|
| Can I drink alcohol? | It’s best to keep it minimal—booze makes dizziness worse. |
| Does betahistine work for all vertigo? | No, it helps most with inner ear causes, not migraine or stroke-related dizziness. |
| Is it safe for older adults? | Yes, but doses might need tweaking, especially if you have asthma or ulcers. |
| What if I miss a dose? | Just skip it and take your next one as planned—don’t double up. |
Remember, vestibular rehabilitation is the main event; betahistine is just the backup singer. The real gains come from sticking with those exercises, even on days when you’d rather just lie down.






Jason Layne
April 28, 2025 AT 11:20 AMDo not be fooled by the glossy pamphlets that present betahistine as a benign aid for vestibular rehabilitation.
The pharmaceutical conglomerates have been quietly funding trials that downplay the drug’s vascular side effects, hoping to lock patients into a perpetual cycle of medication.
What they fail to mention is that the histamine modulation inherent in betahistine can subtly alter cerebral blood flow, a fact that is inconvenient for their market narrative.
By presenting the medication as a mere 'supportive' agent, they disguise the fact that it is a pharmacological crutch designed to keep patients dependent.
The studies you read, laced with corporate sponsorship, often cherry‑pick endpoints that show marginal improvement in dizziness scores while ignoring dropout rates.
Those dropout statistics, when examined closely, reveal that nearly a third of participants abandoned the regimen due to intolerable headaches or gastrointestinal distress.
Moreover, the so‑called ‘enhancement of blood flow’ is a euphemism for vasodilation that can precipitate hypotension in susceptible individuals.
A sudden drop in blood pressure while performing balance exercises is a recipe for falls, contradicting the safety claims made by the manufacturers.
Independent meta‑analyses have concluded that the effect size of betahistine over placebo is statistically insignificant in the majority of vestibular disorders.
If you look beyond the abstract, you will notice that many of the positive trials employed non‑blinded designs, further compromising their validity.
The truth is that vestibular rehabilitation, when executed with proper adherence, yields improvements in up to eighty percent of patients without any pharmacological assistance.
Adding a drug that carries its own risk profile merely muddies the therapeutic waters.
Patients are often led to believe that the combination therapy is a cutting‑edge protocol, when in reality it is a marketing ploy exploiting the anxiety of those with chronic vertigo.
Regulatory agencies have flagged concerns about long‑term usage, yet these warnings are buried deep within the fine print of prescribing information.
If you value true recovery, focus on the exercise regimen, dietary adjustments, and vestibular habituation techniques rather than chasing a pill that may do more harm than good.
The bottom line is that the pharma narrative around betahistine is a classic example of profit‑driven medicine masquerading as evidence‑based care.
Hannah Seo
April 28, 2025 AT 11:37 AMWhile the concerns about pharmaceutical influence are worth noting, many clinicians have observed modest symptom relief when betahistine is used alongside a structured rehab program.
In practice, the drug may help patients tolerate the early, more challenging balance exercises by reducing the intensity of vertigo spikes.
It is essential to monitor for side effects such as mild headaches or gastrointestinal upset, and to adjust the dosage if needed.
Most importantly, the core of recovery remains the patient’s commitment to daily vestibular exercises, proper hydration, and gradual progression of difficulty.
Clinicians often recommend initiating betahistine a few days before the first therapy session to allow the medication to reach steady-state levels.
Regular communication with the therapist ensures that any changes in symptom patterns can be addressed promptly.
Overall, betahistine should be viewed as an adjunct rather than a substitute for the rehabilitation regimen.
Patients who combine both approaches under medical supervision tend to report higher satisfaction and better functional outcomes.
Victoria Unikel
April 28, 2025 AT 11:55 AMi kinda feel like betahistine helps just a lil bit, but not everyone gets the same vibe.
some people say they feel less spin after a week, others dont notice nuthin.
just remember to keep doing the exercises, cuz the med alone wont fix u.
Lorena Garcia
April 28, 2025 AT 12:13 PMTotally hear you – the response to betahistine is all over the map.
I’ve seen friends who swear by it for a few days, then they go back to the same dizzy routine.
Bottom line: don’t let the pill become an excuse to skip the rehab drills.
Stick with the exercises, track your progress, and adjust the med only if your doc says so.
Rama Hoetzlein
April 28, 2025 AT 12:31 PMThe philosophical implication of pairing a synthetic vasodilator with a physical re‑education program is nothing short of a modern Faustian bargain.
We are told to trust the molecule to "ease the flow" while we laboriously retrain our neural pathways – a duality that mirrors the conflict between external control and internal autonomy.
Yet, the aggressive marketing narrative frames this synergy as a triumph of biomedical progress, disguising the underlying ethical compromises.
One must question whether the convenience of a pill merely postpones the deeper, perhaps uncomfortable, confrontation with one’s own physiological limits.
In the grander schema, this reflects a societal tendency to outsource agency to pharmacology, echoing ancient myths where heroes seek divine aid instead of honing their own skills.
The resulting dependency can erode the very resilience that vestibular rehabilitation aims to cultivate.
Moreover, the side‑effect profile – headaches, gastrointestinal unease – serves as a reminder that the body resists such shortcuts.
When patients experience even mild adverse reactions, the illusion of safety shatters, exposing the fragile trust placed in corporate‑sponsored therapeutics.
Thus, the true challenge lies not in choosing betahistine or not, but in confronting the seductive promise of a quick fix while committing to the arduous, yet authentic, process of neural adaptation.
Only through such mindful rejection of superficial solutions can we honor the integrity of both body and mind.
Lindsey Crowe
April 28, 2025 AT 12:49 PMWow, because a philosophy lecture really solves my vertigo, right?