When your body tries to reject a new organ, tacrolimus, a potent immunosuppressant drug used to prevent organ rejection after transplants. Also known as FK506, it works by quieting down the immune system so your body doesn’t attack the new kidney, liver, or heart. Without it, transplant patients face a high risk of failure within weeks. It’s not a cure, but it’s one of the most critical tools doctors have to keep transplanted organs alive.
Tacrolimus doesn’t work alone. It’s often paired with other drugs like mycophenolate or corticosteroids to lower the dose and reduce side effects. But even then, it’s tricky to get right. Too little, and your body rejects the organ. Too much, and you risk kidney damage, high blood pressure, or even nerve problems like tremors or headaches. That’s why regular blood tests are non-negotiable—doctors check your tacrolimus levels to make sure you’re in the sweet spot. It’s not like taking a daily vitamin; this drug demands precision.
What makes tacrolimus even more complex is how it interacts with other things you take. Grapefruit juice can spike your levels dangerously. Some antibiotics, antifungals, and even St. John’s wort can mess with how your body processes it. That’s why talking to your pharmacist about every supplement, OTC med, or herbal tea matters more than ever. You can’t just assume something is safe because it’s natural. The immunosuppressant, a class of drugs that suppress the immune system to prevent rejection or autoimmune damage you’re on needs space to work, and other substances can steal that space.
Most people on tacrolimus are transplant recipients, but it’s also used for severe eczema and some autoimmune diseases when other treatments fail. For those patients, the goal is the same: balance control with safety. You want enough suppression to stop the disease, but not so much that you become vulnerable to infections or cancers. That’s why dose titration—slowly adjusting the amount—is so common. It’s not about finding a magic number once and forgetting it. It’s about watching your body’s signals and adjusting over time.
There’s no sugarcoating it: living on tacrolimus means constant vigilance. But it also means a second chance at life. The posts below cover exactly what you need to manage it safely—from avoiding dangerous food and drug interactions to understanding how kidney function affects dosing, and why some patients need different strategies than others. You’ll find real advice on what to ask your doctor, how to track side effects, and how to handle missed doses without panicking. This isn’t theory. It’s what works for people actually taking this drug every day.
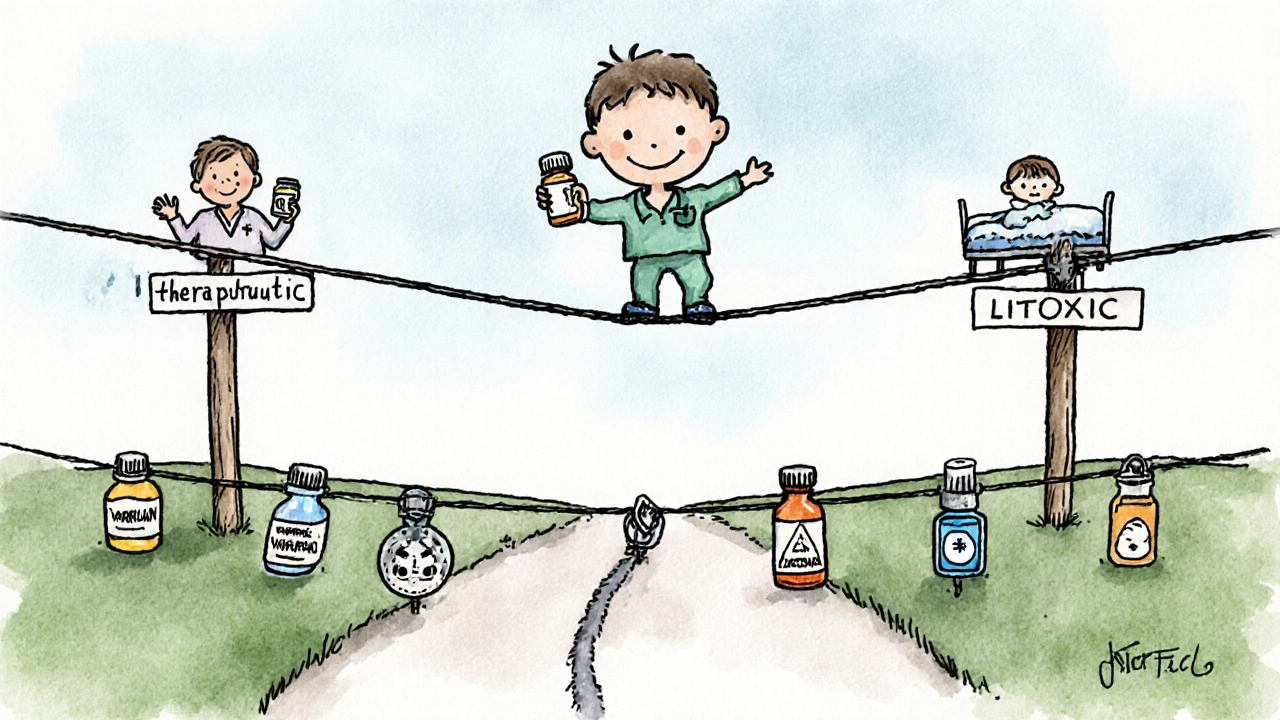
NTI drugs have a tiny margin between safe and toxic doses. Common examples include warfarin, lithium, digoxin, phenytoin, and tacrolimus. These require strict monitoring, careful dosing, and no brand switching without medical approval.
read more