NTI drugs aren’t just another category of medication-they’re the ones where a tiny mistake can mean the difference between healing and hospitalization. These drugs have a razor-thin line between doing their job and causing serious harm. A 10% higher dose of warfarin might send your INR soaring into dangerous territory. A slight switch in generic brands of levothyroxine could leave you fatigued, depressed, or at risk for heart problems. There’s no room for guesswork with NTI drugs. If you or someone you care about is taking one, you need to know exactly what it means-and which drugs fall into this high-risk group.
What Exactly Makes a Drug an NTI Drug?
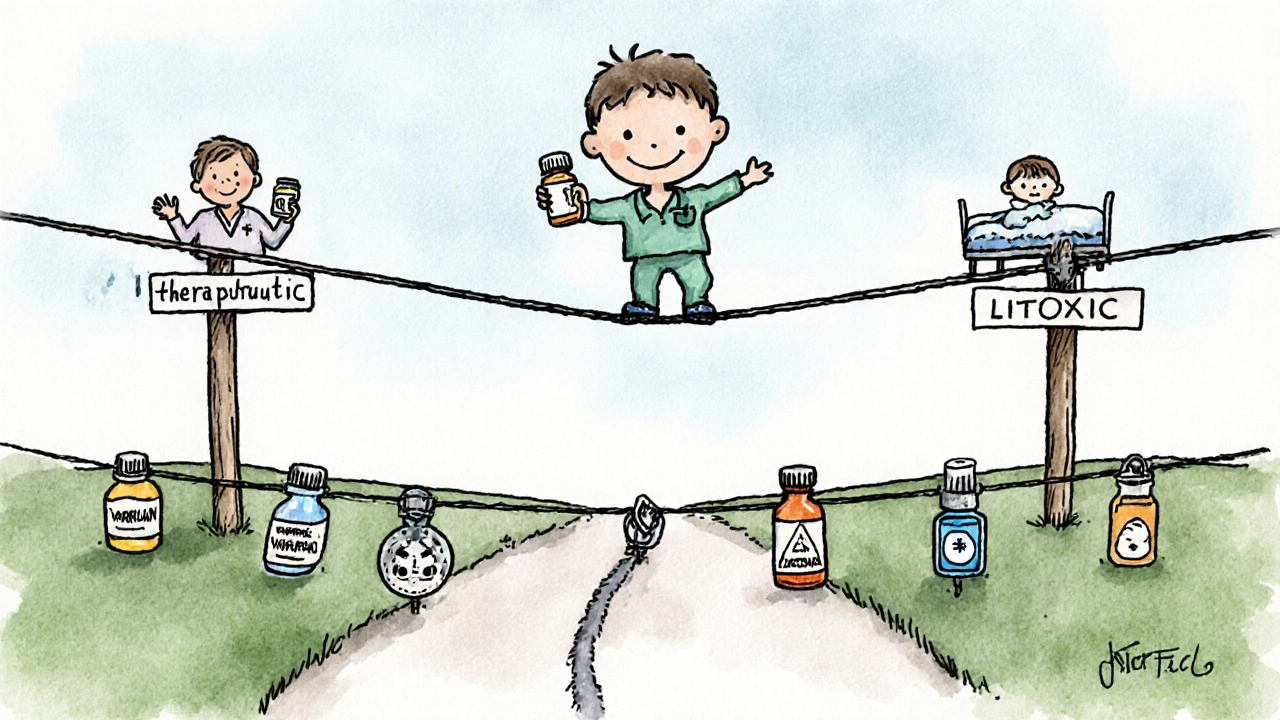
An NTI drug, or Narrow Therapeutic Index drug, has a very small window between the dose that works and the dose that’s toxic. Think of it like walking a tightrope: step a little too far one way, and you’re fine. Step just a tiny bit too far the other way, and you’re in trouble. For most medications, your body can handle some variation. Not with NTI drugs. The difference between a therapeutic blood level and a toxic one is often less than twofold. For example, digoxin’s safe range is 0.5 to 2.0 nanograms per milliliter. Go above 2.0, and you risk fatal heart rhythm problems. Go below 0.5, and the drug doesn’t work at all.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in dose or blood concentration can lead to life-threatening failures or adverse reactions. This isn’t theoretical. Studies show NTI drugs make up only about 15% of medications that require blood level monitoring-but they’re responsible for 30% of dosing-related adverse events. That’s why hospitals and pharmacists treat them differently. Generic substitutions? Not always allowed. Dosing changes? Require close follow-up. Blood tests? Non-negotiable.
The Core NTI Drug List: What’s on the Radar
While the FDA doesn’t publish one official, exhaustive list, multiple authoritative sources-including state pharmacy boards, clinical guidelines, and drug databases-agree on the most common and clinically significant NTI drugs. Here are the ones you’re most likely to encounter:
- Warfarin (Coumadin, Jantoven): This blood thinner requires regular INR tests. The target range is 2.0-3.0 for most conditions. An INR above 4.0 increases major bleeding risk by over 7 times. Even small changes in diet, antibiotics, or supplements can throw it off.
- Lithium: Used for bipolar disorder, lithium’s therapeutic range is just 0.6-1.2 mmol/L. Levels above 1.5 can cause tremors, confusion, kidney damage, or seizures. Many patients miss monitoring appointments, which is why 32% of lithium users fall out of range within six months.
- Digoxin: A heart medication for atrial fibrillation and heart failure. Its narrow window (0.5-2.0 ng/mL) means even a missed dose or a kidney issue can push it into toxicity. Symptoms? Nausea, vision changes, irregular heartbeat.
- Phenytoin (Dilantin): An older but still widely used seizure drug. The therapeutic range is 10-20 mcg/mL. Too low? Seizures return. Too high? Slurred speech, dizziness, nystagmus (jerky eye movements). It interacts with dozens of other drugs, making monitoring essential.
- Carbamazepine (Tegretol): Another anticonvulsant with a similar range (4-12 mcg/mL). It’s also used for nerve pain and bipolar disorder. Its metabolism varies wildly between people due to genetics, making blood levels critical.
- Tacrolimus and Cyclosporine: These immunosuppressants are vital after organ transplants. Tacrolimus targets 5-15 ng/mL in the first months post-transplant. A level just 2 ng/mL too high can cause kidney damage. Too low? Rejection. Transplant centers check these levels 3 times a week at first.
- Levothyroxine: Often thought of as a simple hormone replacement, but even small changes in brand or formulation can cause TSH levels to swing from normal (1.2) to severely high (8.7), leading to fatigue, weight gain, and heart strain. One Reddit user documented a case where switching generics took three months to stabilize.
- Valproic Acid (Depakote): Used for seizures and mood disorders. Therapeutic range is 50-100 mcg/mL. Toxicity can cause liver failure or pancreatitis. It’s especially risky in women of childbearing age due to birth defect risks.
- Aminoglycosides (Gentamicin, Tobramycin): Antibiotics given in hospitals for serious infections. They’re dosed by weight and require both peak and trough blood tests. Trough levels must stay below 2 mcg/mL to avoid permanent kidney or hearing damage.
Why Generic Substitutions Can Be Dangerous
For most drugs, switching from brand to generic is safe and saves money. For NTI drugs? It’s a gamble. The FDA requires stricter bioequivalence standards for NTI generics: the 90% confidence interval for absorption (AUC and Cmax) must fall between 90.00% and 111.11% of the brand drug. For non-NTI drugs, it’s 80-125%. That’s a tighter window because even a 10% difference in absorption can push a patient out of the safe range.
State laws reflect this risk. Forty-seven U.S. states have laws restricting automatic substitution of NTI drugs. Twenty-eight require the prescriber to write “dispense as written” or “no substitution” on the prescription. In North Carolina, the official NTI list includes digoxin, lithium, phenytoin, warfarin, and tacrolimus. Oklahoma’s 2025 list added nortriptyline and esketamine. Pharmacists are trained to flag these. If your pharmacy switches your levothyroxine brand without telling you, speak up.

Monitoring Isn’t Optional-It’s Lifesaving
With NTI drugs, you can’t rely on how you feel. Symptoms of toxicity often appear only after damage has started. That’s why blood tests are mandatory:
- Warfarin: INR every 3-5 days when starting, then weekly until stable.
- Lithium: Every 3-6 months, or sooner if kidney function changes or symptoms appear.
- Digoxin: At least once a year, more often if you’re elderly or have kidney issues.
- Tacrolimus: Three times a week in the first month after transplant, then weekly or biweekly.
- Phenytoin: Every 2-4 weeks when starting, then every 3-6 months.
Cost is a barrier. A single blood test can run $25-$150. Medicare covers 80% for designated NTI drugs, but copays still add up. Many patients skip tests because they feel fine. That’s the trap. You feel fine until you don’t.
Emerging NTI Drugs: The New Frontier
The list isn’t static. New cancer drugs are increasingly falling into this category because they’re designed to hit specific molecular targets-so precisely that the margin for error shrinks. Axitinib (for kidney cancer), ponatinib (for leukemia), and olaparib (for ovarian cancer) now have defined therapeutic blood ranges. For example, ponatinib’s target is 20-50 ng/mL. Outside that, it’s either ineffective or causes dangerous blood clots.
The FDA’s 2023 draft guidance proposes adding apixaban and rivaroxaban to the NTI list, even though they’re often considered safer than warfarin. The reasoning? Bleeding risk still increases sharply at higher levels, and reversal agents are limited. This shows the FDA is catching up with clinical reality.
What You Can Do: A Simple Action Plan
If you’re on an NTI drug, here’s what to do right now:
- Know your drug’s name and purpose. Don’t just say “my heart pill.” Know if it’s warfarin, digoxin, or lithium.
- Ask your doctor or pharmacist: “Is this an NTI drug? What’s the target blood level? How often do I need testing?”
- Keep a log. Write down your test results and any symptoms-dizziness, nausea, tremors, changes in mood or heart rhythm.
- Never switch brands without telling your provider. Even if the label says “generic,” ask if it’s the same formulation.
- Inform all providers. Emergency rooms and new doctors may not know your medication history. Carry a list.
There’s no magic trick to staying safe with NTI drugs. It’s about consistency, communication, and vigilance. The system isn’t perfect-monitoring costs money, EHRs don’t always alert providers, and patients get overwhelmed. But you have power. Ask questions. Track your numbers. Don’t assume it’s fine because you feel okay. With NTI drugs, feeling okay doesn’t mean you’re safe.
Frequently Asked Questions
Are all blood thinners NTI drugs?
No. Warfarin is an NTI drug because its therapeutic range is narrow and it’s affected by many foods and medications. Newer blood thinners like apixaban, rivaroxaban, and dabigatran have wider therapeutic windows and don’t require routine blood monitoring. However, the FDA is reviewing whether some of these should be reclassified as NTI due to bleeding risks at higher doses.
Can I switch from brand to generic NTI drugs safely?
It’s risky without medical supervision. Even FDA-approved generics can have slight differences in absorption. For drugs like levothyroxine or phenytoin, switching brands-even within generics-has caused TSH spikes and seizure breakthroughs. Always consult your doctor before switching. Many states require a doctor’s note to allow substitution.
What happens if I miss a blood test for my NTI drug?
You’re flying blind. For lithium or warfarin, missing a test could mean your level is dangerously high or low without you knowing. Symptoms like fatigue, confusion, or bruising might be dismissed as aging or stress. But with NTI drugs, those symptoms could signal toxicity. If you miss a test, reschedule immediately. Don’t wait for symptoms.
Are NTI drugs only for adults?
No. Children on phenytoin or carbamazepine for epilepsy need the same careful monitoring. Dosing is based on weight and metabolism, which change as they grow. Newborns on digoxin for heart conditions require daily monitoring. Age doesn’t make you immune-kids and seniors are especially vulnerable to dosing errors.
Why aren’t all NTI drugs on the FDA’s official list?
The FDA doesn’t maintain a single public list. Instead, it identifies NTI drugs case-by-case based on clinical data and bioequivalence studies. The Orange Book lists only 12 drugs as NTI-designated, but clinical experts recognize over 30. State pharmacy boards and professional societies fill the gap. The list is evolving, especially with newer cancer drugs.
Next Steps: What to Do Now
If you’re taking an NTI drug, schedule your next blood test today. Don’t wait for your doctor to remind you. If you’ve recently switched medications or pharmacies, call your provider and ask: “Is this the same formulation I was on before?” Keep a printed copy of your drug list and target levels in your wallet. If you’re caring for someone else-especially an elderly parent or transplant patient-help them track their numbers. NTI drugs demand attention, but with the right steps, they can be managed safely. The goal isn’t perfection-it’s awareness. Know your drug. Know your numbers. Speak up.



sharicka holloway
November 26, 2025 AT 12:11 PMJust had to refill my levothyroxine last week and the pharmacy switched brands without telling me. I felt like garbage for three weeks-fatigue, brain fog, the whole thing. Finally called my endocrinologist and they said, 'Oh, that’s a different generic.' Blood test confirmed my TSH had jumped from 1.8 to 7.9. Never again. Always ask if it’s the same formulation. It’s not just about cost-it’s about survival.
Lauren Zableckis
November 27, 2025 AT 16:19 PMThis is the kind of post that should be mandatory reading for every patient on chronic meds. I work in a clinic and see people skip their lithium checks because 'they feel fine.' Then they end up in the ER with tremors and confusion. We don’t talk enough about how fragile these balances are. It’s not paranoia-it’s precision medicine.
reshmi mahi
November 29, 2025 AT 07:54 AMUSA still thinks generics are just as good? Lol. In India we know better. My cousin’s dad switched from brand to generic digoxin and ended up in ICU with ventricular tachycardia. The pharmacy didn’t even know what NTI meant. You think your $5 savings is worth your life? Wake up.
laura lauraa
November 30, 2025 AT 14:47 PMAnd yet… the pharmaceutical-industrial complex thrives on this very fragility. The FDA’s 90-111% bioequivalence standard for NTI drugs is a farce-it’s still a 21% swing, and yet we call it 'safe.' Meanwhile, the same corporations that profit from these drugs lobby against mandatory monitoring programs. It’s not negligence-it’s design. The system isn’t broken; it’s working exactly as intended.
Gayle Jenkins
December 2, 2025 AT 06:52 AMYES. This is exactly why I started carrying a laminated card with my meds and target levels in my wallet. My mom’s on tacrolimus after her transplant, and I help her track her numbers. We log every test, every dose, every change in diet or antibiotics. It’s exhausting-but it’s worth it. If you’re on an NTI drug, don’t wait for a crisis. Be the person who asks the questions. You’re not being difficult-you’re being smart.
Kaleigh Scroger
December 3, 2025 AT 00:24 AMOne thing no one talks about is how hard it is to get insurance to cover frequent blood tests. My dad’s on phenytoin and his copay for each test is $45. Medicare says it’s covered but only if you’re 'actively managing'-which means they deny it if you’re stable. So you’re stuck between risking toxicity or paying out of pocket. The system punishes people who follow the rules.
Elizabeth Choi
December 3, 2025 AT 04:53 AMIt’s funny how people panic about NTI drugs but don’t blink at taking 10 different NSAIDs or sleeping pills. The real danger isn’t the drug-it’s the delusion that medicine is precise. It’s not. It’s a gamble with variables we don’t even measure. You think your INR is stable? You’re just lucky.
Allison Turner
December 4, 2025 AT 17:40 PMWhy do we even bother with this? Just take the brand name. Done. Stop playing Russian roulette with your liver and kidneys. If you can’t afford it, get help. Don’t risk your life for $10 a month.
Darrel Smith
December 5, 2025 AT 10:40 AMThey say 'don’t switch generics' but no one tells you that the brand name is just as bad. Warfarin? That’s a poison that’s been around since the 1940s. They made it to kill rats. Now we give it to grandmas. And you think the FDA cares? They’re paid by the same companies that make the pills. This whole system is rigged. You’re not safe-you’re just being used.
Aishwarya Sivaraj
December 6, 2025 AT 16:09 PMI’m from India and we have the same problem here. My aunt switched from brand to generic carbamazepine and had a seizure within a week. The pharmacist didn’t even know what NTI meant. We need better education-not just for patients but for the people handing out the pills. And yes I know this is long but it matters
Iives Perl
December 7, 2025 AT 00:36 AMNTI drugs? More like NTI-Narrow Therapeutic Illusion. They’re tracking your blood levels but who’s tracking the labs? I bet 70% of those 'accurate' readings are faked or misread. The system’s a lie. And don’t get me started on the FDA. 🤫
steve stofelano, jr.
December 8, 2025 AT 10:51 AMThank you for this comprehensive and meticulously researched exposition. The nuanced interplay between pharmacokinetic variability, regulatory oversight, and patient autonomy is both profoundly important and tragically underappreciated. I would respectfully suggest that future iterations of this discourse consider incorporating comparative international regulatory frameworks, particularly those of the European Medicines Agency, which employ a more granular classification system for therapeutic index risk stratification.