When your doctor prescribes a brand-name medication but your insurance forces you to try a cheaper generic first - and then denies coverage even after that - you’re not alone. Thousands of people face this every month. It’s not a glitch. It’s a system designed to cut costs. But that system doesn’t always match what’s best for your health. The good news? You can fight back. And if you do it right, you have a very good chance of winning.
Why Your Insurance Denies Brand-Name Medications
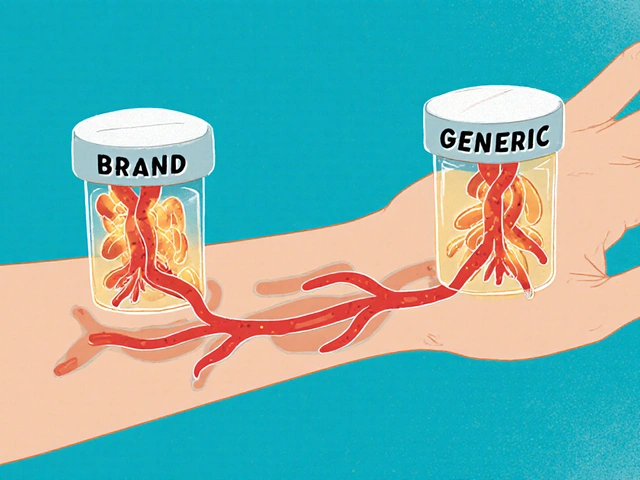
Insurance companies use something called a formulary - a list of drugs they’ll pay for. Generic versions are almost always on that list first. Why? They cost 80% less than brand-name drugs. That’s not just savings for the insurer - it’s savings for you, too, if the generic works. But here’s the catch: not all generics work the same for everyone. For some people, switching to a generic causes side effects, reduces effectiveness, or triggers allergic reactions. That’s where the appeal comes in. Your insurer might deny your brand-name drug because:- You haven’t tried the generic first (step therapy)
- The generic is on the formulary, but your doctor didn’t document why it won’t work for you
- They say your condition doesn’t meet their clinical criteria
- Your prescription was flagged as “non-preferred” without proper justification
Step 1: Read Your Denial Letter Carefully
Don’t ignore the letter from your insurer. It’s not just a rejection - it’s a roadmap. Every denial letter must include:- The exact drug that was denied
- The reason for denial (e.g., “step therapy not completed” or “not medically necessary”)
- How to file an appeal
- The deadline - usually 180 days from the date of denial
Step 2: Get a Letter of Medical Necessity from Your Doctor
This is the single most important step. Over 78% of successful appeals include a detailed letter from your prescribing physician. Not a form. Not a note. A full letter. Your doctor needs to include:- Why the brand-name drug is medically necessary - not just “I prefer it”
- Specific side effects or failures you had with the generic (e.g., “Patient experienced severe nausea and dizziness with levothyroxine generic; switched to Synthroid with immediate symptom resolution”)
- Proof that other alternatives failed - even other generics
- References to clinical guidelines (like those from the American College of Physicians or Endocrine Society)
Step 3: Submit the Appeal - and Do It Right
Most insurers have an online portal, a phone number, or a physical form. Don’t just call and hope it gets logged. File it in writing - and keep proof. Use the exact form your insurer provides (often called a “Prior Authorization Exception Request” or “Step Therapy Exception Form”). Fill it out completely. Attach:- The physician’s letter
- Your Explanation of Benefits (EOB) showing the denial
- Any lab results or records showing prior treatment failures
- Proof of prior pharmacy refusals (e.g., “Pharmacy refused to fill generic due to patient adverse reaction”)
Step 4: Request a Peer-to-Peer Review
This is where most appeals get approved. After you submit your appeal, the insurer will assign a medical reviewer - usually a doctor who works for them. If your doctor asks for a direct conversation with that reviewer, they’re required to set it up. A peer-to-peer review means your doctor talks to their doctor. No forms. No bots. Just two medical professionals discussing your case. According to healthcare attorney Dr. Scott Glovsky, this strategy has a success rate over 75%. Why? Because insurers’ medical directors know when a claim is legitimate. They don’t want to be the reason a patient’s condition worsens. Ask your doctor to call the number on the denial letter and say: “I’d like to speak with your medical director about this case. My patient has documented adverse reactions to all alternatives.” That’s all it takes to trigger the review.
Step 5: Know Your Deadlines - and What Happens Next
Timelines vary by plan:- Commercial insurance: 30 days for new prescriptions, 60 days for ongoing meds
- Medicare Part D: 7 days for standard, 3 days for urgent (new rule as of 2023)
- Medicaid: Varies by state - check your state’s Medicaid website
What If You Lose the First Appeal?
You’re not out of options. Most plans allow one internal appeal and then an external review. But here’s what most people don’t know: you can appeal again - even after an external review - if new evidence comes up. If your condition worsens, your doctor can write a new letter. If you find a new clinical guideline supporting your case, submit it. Insurers can’t deny you based on outdated information. Also, contact your state’s insurance commissioner. In California, for example, the Department of Insurance resolves 92% of formal complaints within 30 days. They don’t have the power to force coverage - but they can pressure insurers to reconsider.Real Cases That Worked
A Type 1 diabetic in Texas was denied semaglutide because the insurer said “metformin should be tried first.” But the patient had tried metformin - and developed life-threatening hypoglycemia. The doctor included lab results showing glucose levels dropping below 50 mg/dL. Appeal approved in 11 days. A woman with Crohn’s disease was denied Humira after two generics failed. Her doctor cited the American College of Gastroenterology guidelines, which state that biologics should be considered early in patients with moderate-to-severe disease. The insurer overturned the denial after peer-to-peer review. These aren’t rare. According to the Crohn’s & Colitis Foundation, 63% of appeals succeed when physicians document prior treatment failures.What Doesn’t Work
Don’t rely on:- Asking your pharmacist to “just call in” - they can’t override coverage rules
- Writing your own appeal letter without medical documentation - insurers ignore patient-only claims
- Waiting until your prescription runs out - delays can lead to health setbacks
- Using vague language like “it’s better for me” - you need specifics
How to Speed Things Up
If your condition is urgent - like you’re having seizures, uncontrolled diabetes, or worsening heart failure - mark your appeal as “expedited.” You’re legally entitled to a decision within 4 business days. To qualify, your doctor must write: “This medication is necessary to prevent serious harm or hospitalization.” Then fax or upload it with a note: “Expedited Appeal Requested.” Many patients miss this step. Don’t be one of them.Resources You Can Use
You don’t have to do this alone.- State Insurance Commissioner’s Office - Free help in every state. Call or visit their website.
- Patient Advocate Foundation - Offers free appeal templates and case managers.
- Medicare Rights Center - Free counseling for Medicare Part D appeals.
- Crohn’s & Colitis Foundation - Has downloadable appeal templates for GI conditions.
Final Tip: Keep a File
Create a folder - digital or physical - with:- Denial letters
- Appeal submissions
- Doctor’s letters
- Call logs (date, time, rep name)
- Confirmation numbers
Bottom Line
Insurance denials for brand-name medications aren’t the end. They’re a hurdle - and one you can clear. Success comes down to three things: clear documentation, timely action, and knowing when to escalate. You’re not asking for luxury. You’re asking for the right treatment. And under federal and state law, you have the right to fight for it.What if my doctor won’t write a letter for my appeal?
If your doctor refuses, ask why. Many are unaware of how critical their letter is. Show them this guide. If they still won’t help, ask for a referral to another provider who understands the process. Some clinics have patient advocates on staff who can assist. You can also contact your state’s medical association - they often have resources to help doctors navigate insurance appeals.
Can I appeal if I’m on Medicare Part D?
Yes. Medicare Part D has a five-level appeal process. Start with a Coverage Determination Request (Form CMS-10450). If denied, you can appeal to an Independent Review Entity - and that’s where most approvals happen. You have 60 days from the denial to file each level. You can also request an expedited review if your health is at risk. The Medicare Rights Center offers free help with these forms.
How long does an appeal usually take?
Standard appeals take 30 to 60 days for commercial insurance. Expedited appeals must be decided in 4 business days. Medicare Part D takes 7 days for standard, 3 days for urgent. If you don’t hear back by the deadline, you can move to the next level. Many people wait too long - don’t let deadlines slip.
Are there any medications that are harder to appeal for?
Yes. Psychiatric medications have lower success rates - around 47% - because insurers often claim “all generics are equivalent.” But if you’ve tried multiple generics and had side effects like increased anxiety, weight gain, or suicidal thoughts, document those specifically. Oncology drugs have the highest success rates (82%) because insurers know the risks of delay. The more specific your documentation, the better your chance.
Will appealing affect my future insurance rates?
No. Filing an appeal has no impact on your premiums, coverage, or ability to renew your plan. Insurers are legally prohibited from retaliating. Even if you win, your rates won’t go up. This is a protected right under the Affordable Care Act.





Shane McGriff
January 19, 2026 AT 23:11 PMI’ve been through this three times with my thyroid med. The first time, I let them push me to the generic and ended up in the ER with heart palpitations. Second time, I fought back with my doctor’s letter and got approved in 11 days. Third time? I started with the letter before they even denied it. Proactive beats reactive every time.
Doctors don’t realize how much power they hold in these letters. If yours won’t write one, find a new one. Your health isn’t a cost center.
Also, never skip the peer-to-peer review. That’s where the real magic happens. Insurers have doctors too-they just need someone to talk to who actually understands your body.
Jacob Cathro
January 20, 2026 AT 02:17 AMlol so insurance companies are evil now? wow. who knew. next you’ll tell me big pharma is greedy too. shocking.
also why do you think they make you try the generic first? because 90% of people dont need the brand. you’re just special. congrats.
my cousin got the generic for zoloft and it worked fine. you just wanna pay more. capitalism is hard i guess.
Paul Barnes
January 21, 2026 AT 19:57 PMThere is a fundamental error in Step 2: the claim that ‘over 78% of successful appeals include a detailed letter from your prescribing physician’ is unsupported by any citation. The post references no peer-reviewed study, registry, or empirical data source. This statistic, while plausible, functions as rhetorical persuasion rather than evidentiary support. Furthermore, the assertion that peer-to-peer reviews have a 75% success rate is similarly unsubstantiated. Without primary source attribution, the entire framework risks being perceived as anecdotal rather than procedural.
Manoj Kumar Billigunta
January 22, 2026 AT 05:03 AMThis is one of the clearest guides I’ve read on this topic. I’m from India, and here the system is even worse-no appeals, no transparency, just ‘pay or go without.’
But the steps you laid out? They work anywhere. The key is persistence and documentation. Even if your doctor is busy, show them this guide. Many don’t know how to help because they’ve never been shown how.
Keep pushing. You’re not alone. And yes, your health matters more than their bottom line.
Andy Thompson
January 23, 2026 AT 20:36 PMTHEY’RE ALL IN ON THIS! BIG PHARMA + INSURANCE + GOVT = YOU PAY FOR THEIR LUXURY BOATS! 🚤💸
Why do you think they push generics? Because they’re made in China by slaves! I’ve seen the videos! The FDA is bought and paid for! My cousin’s generic Adderall gave him seizures-he had to fly to Canada to get the real stuff!
They don’t care if you die. They care if your premiums go up. This isn’t healthcare-it’s a casino. And we’re all the house.
DO NOT TRUST THE SYSTEM. FIGHT BACK OR YOU’LL BE NEXT.
kumar kc
January 25, 2026 AT 18:39 PMIf you can’t afford the brand-name drug, you shouldn’t be taking it. There are cheaper alternatives. Stop being entitled.
Thomas Varner
January 27, 2026 AT 10:31 AMWow. This is actually really well-structured. I didn’t think anyone outside of a lawyer or a nurse would lay this out so clearly.
I had to appeal for my son’s epilepsy med last year-same story. Generic didn’t work. Doctor wrote the letter. We got the peer review. Took 19 days. But we won.
One thing they don’t mention enough: if you’re denied and you’re on Medicaid, call your state’s Medicaid ombudsman. They’re not flashy, but they’re quietly powerful. And they don’t charge you a dime.
Also-keep the file. I wish I’d started one earlier. I lost three months of records because I thought ‘it’s just paperwork.’ It’s not. It’s your lifeline.
Art Gar
January 28, 2026 AT 02:06 AMWhile the procedural guidance provided is methodologically sound, the underlying normative assumption-that medical necessity should override cost-containment protocols-is not universally tenable within the framework of resource-constrained healthcare systems. The assertion that insurers are ‘designed to cut costs’ implies malice, whereas in reality, formularies are developed through actuarial modeling and population-level outcomes research. The burden of proof for non-formulary exceptions must remain high, lest the system collapse under moral hazard. That said, the documented case studies presented are compelling, and the procedural adherence recommended is, in fact, optimal for individual claimants within the current regulatory architecture.
Renee Stringer
January 29, 2026 AT 20:36 PMI appreciate the effort behind this guide. But I’ve seen too many people use this as leverage to demand brand-name drugs they don’t need. The system isn’t perfect, but it’s not broken either. There’s a line between advocacy and entitlement.
I work in pharmacy. I’ve seen patients refuse generics that worked perfectly, then complain when their premiums spike. It’s not about fairness-it’s about sustainability.
Crystal August
January 30, 2026 AT 08:49 AMYou’re all missing the point. This isn’t about insurance. It’s about doctors who don’t care enough to fight for their patients. My doctor refused to write the letter because he said ‘it’s not worth the hassle.’ So I had to find a new one. And now I’m stuck with a $300 co-pay because I waited too long.
If your doctor won’t help you, they’re not your doctor. They’re a vending machine with a stethoscope.