Medication-Food Timing Calculator
Select your medication type and meal timing to get personalized guidance on safe medication administration
Results
When you take a pill, you might think it’s just about the medicine. But what you eat-or drink-can change how that medicine works in your body. Sometimes, food makes a drug work better. Other times, it turns a safe medication into a dangerous one. This isn’t rare. About 30% of all bad reactions to medications happen because of what people ate or drank around the time they took their pills.
Why Food Changes How Medicines Work
Food doesn’t just fill your stomach. It changes your body’s chemistry. When you eat, your stomach acid levels shift. Your gut starts moving differently. Liver enzymes wake up. All of this affects how your body absorbs, breaks down, or gets rid of a drug. There are three main ways food messes with medicine:- Absorption problems: Food can block a drug from entering your bloodstream. For example, calcium in milk or yogurt binds to antibiotics like tetracycline and reduces absorption by up to 50%.
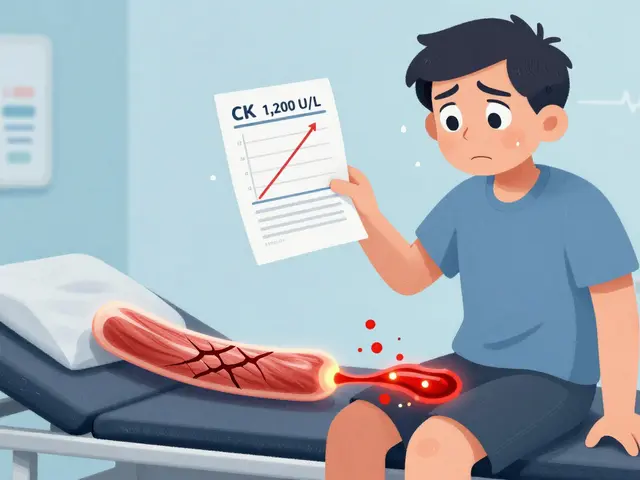
- Metabolism changes: Some foods slow down or speed up how your liver processes drugs. Grapefruit juice is the most famous example-it blocks an enzyme called CYP3A4, which normally breaks down statins. Without it, simvastatin levels can jump by 330%, raising the risk of muscle damage.
- Opposite effects: Certain foods directly fight the drug’s action. Vitamin K in spinach, kale, or broccoli counteracts warfarin, a blood thinner. If you eat a big salad one day and none the next, your blood can clot dangerously-or bleed uncontrollably.
Medications That Are Especially Sensitive to Food
Not all drugs are affected the same. Some are picky. Others don’t care what you eat. Here’s what you really need to know.Antibiotics
Many antibiotics don’t work well with dairy or calcium supplements. Ciprofloxacin and other fluoroquinolones can lose 75-90% of their power if taken with milk, cheese, or even fortified orange juice. The fix? Wait at least 2 hours before or 4 hours after eating calcium-rich foods. Amoxicillin, on the other hand, is fine with food. It won’t hurt it. So don’t skip meals just because you’re on antibiotics-unless your doctor says so.Thyroid Medicine
Levothyroxine (Synthroid) is one of the most common pills people take. But it’s also one of the most sensitive. If you take it with breakfast-even a piece of toast-your body absorbs 34% less of the drug. That means your thyroid levels stay low, you stay tired, and your cholesterol might rise. The rule is simple: Take it on an empty stomach, 60 minutes before eating anything. Water is fine. Coffee, milk, or fiber cereal? Wait.Blood Thinners
Warfarin (Coumadin) is tricky. It doesn’t care if you eat. But it cares how much vitamin K you eat every day. One cup of cooked kale has 483 micrograms of vitamin K. That’s more than most people need in a full day. If you eat kale every day, your blood stays stable. If you eat it only once a week, your INR (a blood test that measures clotting) swings wildly. The goal isn’t to avoid vitamin K. It’s to keep it steady. Eat the same amount every day. A food diary helps. Patients who track their intake have 28% fewer emergency blood tests.Heart Medications
Statins like simvastatin and atorvastatin are safe with most foods-except grapefruit. One glass of grapefruit juice can turn a normal dose into an overdose. The FDA says grapefruit interactions cause over 1,100 ER visits every year. Newer blood thinners like apixaban (Eliquis) don’t have this problem. They’re much less affected by diet. If you’re on warfarin and find it hard to manage your diet, ask your doctor about switching.Stomach Pills
Proton pump inhibitors like omeprazole (Prilosec) need to be taken 30-60 minutes before your first meal. That’s when your stomach starts making acid. If you take them after eating, they won’t work as well. H2 blockers like famotidine (Pepcid) don’t care when you eat. They work either way.Painkillers
NSAIDs like ibuprofen and naproxen can irritate your stomach. Taking them with food cuts your risk of ulcers by more than half. One study found 15% of people who took ibuprofen on an empty stomach got ulcers. Only 4% did when they ate first. That’s one of the few times food helps. So if your doctor says “take with food,” don’t ignore it.MAO Inhibitors
These older antidepressants are rare now, but they’re dangerous if you don’t know the rules. They can cause a deadly spike in blood pressure if you eat foods with tyramine: aged cheese, cured meats, soy sauce, tap beer, or fermented foods. A single slice of blue cheese can contain 100-400 mg of tyramine. That’s enough to trigger a hypertensive crisis. If you’re on an MAOI, you need a full list of forbidden foods. No guessing.When to Take Your Pills: The Timing Rules
“Take on an empty stomach” sounds simple. But what does that really mean? The standard is: 1 hour before or 2 hours after a meal. That’s what studies show works best. Many people think “empty stomach” means no food for 30 minutes. That’s not enough. In one trial, patients who waited 30 minutes before eating had 22% less drug in their blood than those who waited 60 minutes. Here’s a quick guide:- Take before meals: Levothyroxine, omeprazole, bisphosphonates (for osteoporosis), some antibiotics.
- Take with food: NSAIDs (ibuprofen, naproxen), fat-soluble drugs (diazepam, griseofulvin), some antifungals.
- Avoid with food: Tetracycline, ciprofloxacin, thyroid meds, calcium supplements (if you’re on antibiotics).
- Avoid with grapefruit: Simvastatin, atorvastatin, felodipine, cyclosporine, some anti-anxiety drugs.
What Most Patients Get Wrong
A lot of people think they’re doing fine. But research shows they’re missing key details.- 68% don’t understand what “take on empty stomach” means. They take their pill with a sip of coffee or a bite of toast.
- 54% have never heard that grapefruit can be dangerous with meds.
- 41% believe all pills should be taken with food to protect their stomach-even if that makes the drug useless.
How to Stay Safe
You don’t need to memorize every interaction. But you can protect yourself with three simple habits.- Ask your pharmacist every time you get a new prescription. Not your doctor. Your pharmacist. They’re trained to spot food-drug risks. Ask: “Is there anything I shouldn’t eat or drink with this?”
- Use a medication schedule. Write down what you take, when, and with what. Apps like MyMedSchedule (from NIH) let you log meals and get alerts if something conflicts.
- Be consistent. If you take your blood thinner with spinach, eat spinach every day-not just on Sundays. If you take levothyroxine before breakfast, do it at the same time every morning. Your body needs routine.

What’s Changing in 2025
New rules are coming. Starting January 1, 2025, Medicare Part D requires pharmacists to give food-drug interaction counseling to every senior starting a high-risk medication. That includes blood thinners, statins, and antidepressants. The FDA now requires all new drug labels to include clear food interaction warnings-down to the minute. No more vague “take on empty stomach.” Now it says: “Take 60 minutes before breakfast.” And if you’re on a statin and drink grapefruit juice regularly? Your doctor might now recommend a genetic test to see if your liver breaks down drugs slowly. That’s not science fiction. It’s happening now.Bottom Line
Food isn’t the enemy. But it’s a powerful player in how your medicine works. A banana won’t hurt your blood pressure pill. But a glass of grapefruit juice might. A slice of cheese won’t ruin your antibiotic. But a bowl of yogurt might. The key isn’t perfection. It’s awareness. Know which meds need space from food. Know which foods can cancel out your treatment. And when in doubt? Ask your pharmacist. It’s the easiest way to avoid a bad reaction.Medicines are powerful. But they’re only as good as how you take them.




Cassie Henriques
December 15, 2025 AT 15:59 PMSo grapefruit juice + statins = 330% spike? That’s wild. CYP3A4 inhibition is such a classic pharmacokinetic nightmare-why isn’t this on every prescription bottle in neon? Also, vitamin K consistency with warfarin? 28% fewer ER visits? That’s a public health win waiting to happen. My pharmacist flagged this for me after my INR went nuclear last winter. 🤯
Benjamin Glover
December 17, 2025 AT 09:34 AMTypical American medical laziness. You can’t expect people to read labels. In the UK, we have proper pharmacist consultations-no one takes tetracycline with yogurt without being told, ‘No, you idiot, it won’t work.’
Jake Sinatra
December 17, 2025 AT 22:41 PMThis is exactly why medication adherence is more about education than compliance. The data here is solid-30% of adverse events tied to food interactions? That’s preventable. I work in clinical pharmacy, and I’ve seen patients on levothyroxine take it with their morning coffee and wonder why they’re still exhausted. It’s not the drug. It’s the timing. Consistency isn’t optional-it’s physiology.
RONALD Randolph
December 19, 2025 AT 05:42 AMWRONG. You say ‘take on empty stomach’-but what does that mean? 30 minutes? 60? 90? The FDA’s new rule is long overdue. No more vague language. If the label says ‘60 minutes before breakfast,’ then it’s 60 minutes. Not 55. Not 58. Sixty. Period. And if you’re drinking grapefruit juice while on simvastatin? You’re not just being careless-you’re endangering lives. There should be a warning label with a skull and crossbones.
Raj Kumar
December 20, 2025 AT 08:07 AMBro, this is so real. I’m from India, and my auntie was on warfarin, ate lots of curry leaves and spinach every day, then switched to just rice and dal for a week-her INR went from 2.5 to 5.8. We didn’t know why. Then the pharmacist said, ‘Same amount of green, every day.’ Now she tracks it in a notebook. No more panic. Simple, right? Also, don’t take antibiotics with curd. I learned that the hard way.
John Brown
December 20, 2025 AT 12:39 PMLove this breakdown. So many people think ‘natural’ means ‘safe’-but kale can be as dangerous as a drug if you’re on warfarin. I used to think ‘take with food’ meant ‘whenever you feel like it.’ Now I set alarms. My pharmacist gave me a printed chart. Best 5 minutes of my life.
Christina Bischof
December 21, 2025 AT 00:56 AMMy dad took his blood pressure med with grapefruit juice for years. No idea it was a problem. He ended up in the hospital. I wish this was taught in high school health class.
Jocelyn Lachapelle
December 21, 2025 AT 18:24 PMJust started levothyroxine and I’m already obsessed with timing. 60 minutes before breakfast? Done. No coffee, no toast, no sneaky almond milk. I’m weirdly proud of myself. Also, I started a food log-turns out I eat kale every Tuesday. Who knew? This stuff matters.
Mike Nordby
December 23, 2025 AT 16:07 PMThank you for including the 2025 Medicare changes. Pharmacists being required to counsel seniors on food-drug interactions? This is systemic change. It’s not about blaming patients-it’s about designing systems that account for human forgetfulness. The FDA’s move toward minute-specific labeling? Long overdue. This post should be mandatory reading for every prescriber.