Drug Absorption Calculator
How pH Affects Drug Absorption
Enter the pKa of the drug and your current/pH-raised stomach pH to see how absorption changes. The Henderson-Hasselbalch equation determines how drugs dissolve based on pH relative to their pKa.
Understanding the result:
Weak Base Drugs (pKa > 7): Higher pH reduces absorption (more ionized). A 2-unit pH increase can reduce absorption by 90%.
Weak Acid Drugs (pKa < 7): Higher pH increases absorption (less ionized). A 2-unit pH increase can increase absorption by 90%.
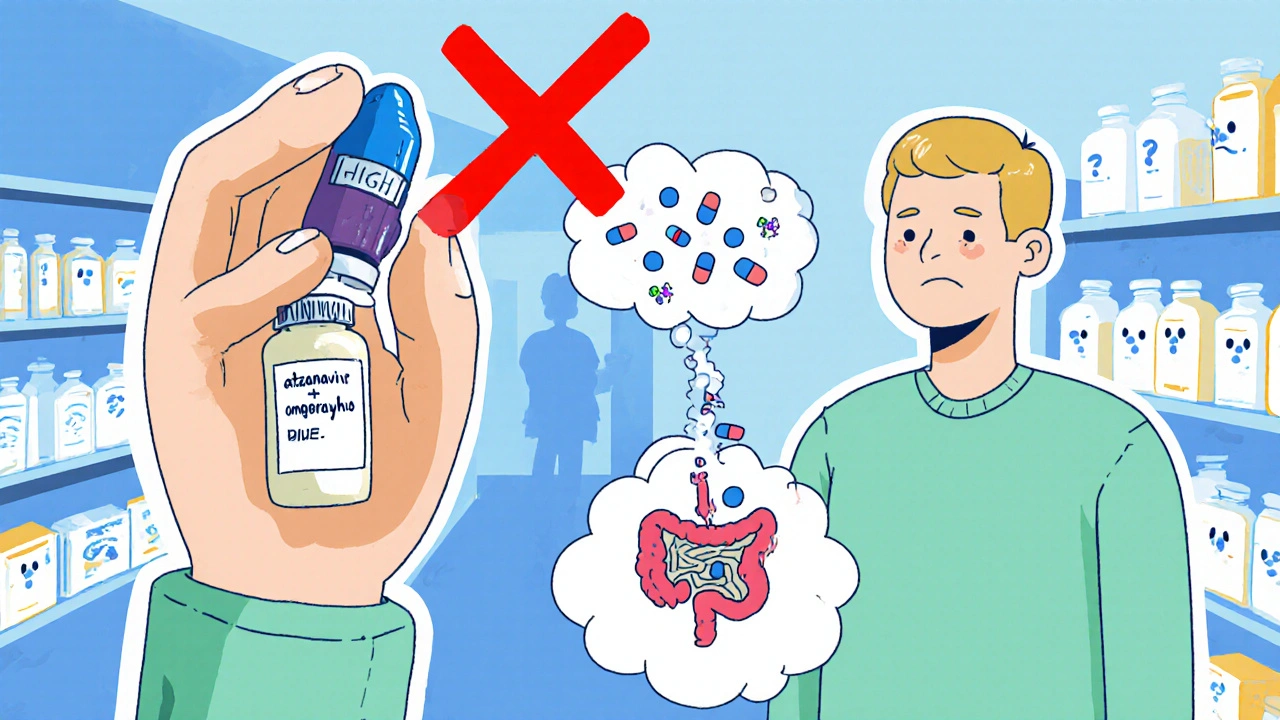
Ever taken a heartburn pill and then wondered why your HIV meds stopped working? That isn’t a coincidence - acid-reducing medications can dramatically change how other drugs dissolve and get into your bloodstream.
What Are Acid-Reducing Medications?
Acid-reducing medications, often called ARAs, are drugs that raise the stomach’s pH. The two main families are:
- Proton Pump Inhibitors (PPIs) - they irreversibly block the H+/K+ ATPase pump in parietal cells, keeping the stomach less acidic for up to 24 hours.
- H2-Receptor Antagonists (H2RAs) - they competitively block histamine H2 receptors, producing a shorter‑lasting pH rise.
Both classes lift the fasting gastric pH from the normal 1.0‑3.5 range to roughly 4.0‑6.0, which sounds harmless but reshapes the chemistry of every oral drug that passes through the stomach.
How Stomach pH Controls Drug Solubility
The key equation is the Henderson‑Hasselbalch relationship:
pH = pKa + log([non‑ionized]/[ionized])
When the environment is acidic (low pH), weak bases (pKa > 7) become ionized, which boosts their water solubility. Raise the pH and they stay mostly non‑ionized, so they dissolve more slowly. The opposite happens for weak acids (pKa < 7).
Because most oral absorption (about 90 %) actually occurs in the small intestine, the stomach’s role is to dissolve the tablet into a fine slurry. If dissolution is slowed, less drug reaches the intestine, and the overall exposure (AUC) can drop dramatically.
Which Drugs Get Caught in the pH Trap?
Pharmacokinetic studies show that about 25‑50 % of the top 200 prescribed medicines are weak bases and therefore vulnerable. The most clinically‑significant examples include:
- Atazanavir - an HIV protease inhibitor (pKa 5.2). Co‑administration with a PPI like omeprazole cuts its AUC by up to 95 % (Celerion White Paper, 2022). The drug label advises complete avoidance of PPIs.
- Dasatinib - a leukemia medication. PPIs lower its exposure by roughly 60 %, often requiring dose escalation or a 12‑hour dosing gap.
- Ketoconazole - an antifungal with notoriously poor solubility at pH > 5. Interaction with PPIs can drop levels by 75 %, rendering the treatment ineffective.
- Aspirin (weak acid, pKa 3.5) shows a modest 15‑25 % increase in absorption when the stomach is less acidic, but this change rarely demands a dose tweak.
Enteric‑coated pills add another layer of complexity. Raising gastric pH can cause premature dissolution of the coating, exposing acid‑labile drugs to the stomach’s harsh environment or creating gastric irritation.
PPIs vs H2RAs: How Their Interaction Risk Stacks Up
| Feature | Proton Pump Inhibitors (PPIs) | H2‑Receptor Antagonists (H2RAs) |
|---|---|---|
| Duration of pH elevation (>4) | 14‑18 hours | 8‑12 hours |
| Typical reduction in weak‑base AUC | 40‑80 % | 20‑40 % |
| High‑risk drugs (e.g., atazanavir, dasatinib, ketoconazole) | Often contraindicated | Dose adjustment usually sufficient |
| Effect on weak acids | 15‑25 % increase (generally not clinically critical) | Similar modest rise |
| Typical OTC availability | Yes (e.g., omeprazole, lansoprazole) | Yes (e.g., ranitidine, famotidine) |
The longer, deeper pH shift from PPIs explains why they are the primary culprit in serious drug‑absorption failures.
Real‑World Clinical Impact
Data from a 2023 retrospective cohort (12,543 patients) linked concurrent PPI use with a 37 % increase in dasatinib treatment failure. Reddit threads from early 2024 feature patients whose HIV viral load surged after starting omeprazole alongside atazanavir - an anecdote that mirrors the Celerion findings.
FAERS records from 2020‑2023 list 1,247 reports of “therapeutic failure” tied to ARAs, with atazanavir, dasatinib, and ketoconazole accounting for over 75 % of those cases.
On the positive side, a 2022 Journal of Clinical Oncology study showed that staggering dasatinib dosing 12 hours apart from a PPI salvaged efficacy in 85 % of patients, underscoring that timing strategies can work when avoidance isn’t possible.

Managing the Interaction Risk
Guidelines released by the FDA in 2023 outline three practical levers:
- Staggered dosing: Give the pH‑dependent drug at least 2 hours before the ARA for weak bases. This only cuts the interaction by ~30‑40 %, so it’s a partial fix.
- Switch the acid reducer: Use an H2RA instead of a PPI when the therapeutic goal allows it, or resort to short‑acting antacids with a 2‑4 hour gap.
- Choose pH‑independent formulations: Extended‑release or enteric‑coated versions designed to dissolve beyond the stomach can bypass the problem.
Pharmacist‑led medication reviews have proven hugely effective; a 2023 JAHPA study reported a 62 % drop in inappropriate ARA co‑prescribing after pharmacist intervention.
Electronic health record (EHR) alerts also help - Epic’s 2023 data showed 78 % clinician compliance when a high‑risk ARA‑drug combination triggered a warning.
Future Directions - From pH‑Independent Drugs to AI Prediction
Pharma companies are already redesigning molecules to dissolve at neutral pH. Roughly 37 % of new molecular entities in 2023 featured pH‑independent delivery platforms, according to Nature Reviews Drug Discovery.
AI‑driven interaction engines are emerging, too. Google Health’s 2024 prototype predicts ARA‑drug clashes with 89 % accuracy, offering clinicians real‑time risk scores.
Personalized gastric‑pH monitoring is another frontier. A 2024 Clinical Pharmacology study found that patient‑specific pH curves explain 40‑60 % of the variability in interaction magnitude, hinting that future dosing regimens could be tailored to each individual’s acid profile.
Lastly, deprescribing initiatives aim to cut chronic, unnecessary PPI use by up to 30‑50 % in the next few years, potentially preventing thousands of therapeutic failures annually.
Quick Takeaways
- Acid‑reducing meds raise stomach pH, which can halve or worse the absorption of weak‑base drugs.
- PPIs pose a higher risk than H2RAs because they sustain a higher pH for longer.
- Key culprits include atazanavir, dasatinib, and ketoconazole - avoid co‑use whenever possible.
- Staggered dosing, alternative reducers, and pH‑independent formulations are the main mitigation tools.
- Pharmacist review and EHR alerts dramatically reduce unsafe combinations.
- Future tech (AI, personalized pH monitoring) promises smarter, patient‑specific solutions.
Do all acid‑reducing drugs affect drug absorption?
No. The impact depends on how much the drug raises gastric pH and how long that effect lasts. PPIs, which keep the stomach at pH > 4 for 14‑18 hours, cause the biggest problems. H2RAs have a shorter, milder effect, and antacids act only for a few hours.
Can I take my PPI and atazanavir together if I space them out?
Atazanavir is listed as a contraindication with PPIs. Even a 12‑hour gap does not restore exposure enough to be safe. Switching to an H2RA or an antacid, or using an atazanavir‑compatible formulation, is the recommended approach.
What’s the easiest way for a clinician to spot a dangerous ARA interaction?
Most modern EHRs include decision‑support alerts. When a high‑risk drug like dasatinib is prescribed, the system flags any active PPI order and suggests alternatives or dosing adjustments.
Are over‑the‑counter antacids a safe fallback?
Antacids work for only 1‑2 hours, so they can be used if you need quick relief, but they don’t solve chronic acid‑reduction needs. Timing them 2‑4 hours apart from the pH‑dependent drug is usually enough.
Will future pH‑independent drugs eliminate this problem?
They’ll reduce it dramatically, but until those formulations dominate the market, clinicians still need to manage existing drugs with the strategies outlined above.







Tamara Schäfer
October 25, 2025 AT 14:06 PMJust think about how a tiny shift in stomach pH can ripple through the entire pharmacokinetic cascade, reshaping the fate of drugs we rely on. It's almost poetic that a simple antacid can undermine life‑saving therapy, yet also a reminder that biology is beautifully intricate. If we view these interactions through a lens of curiosity rather than fear, we can empower patients to make smarter choices. Remember, the gut is more than a bag of acid; it's an active participant in drug destiny. So, when you pop a PPI, imagine the downstream domino effect on weak‑base medications, and maybe consider an H2 blocker as a gentler alternative. Optimism lies in knowing that clinicians now have tools-like staggered dosing-to mitigate these risks. Let's keep asking questions, stay vigilant, and trust that the system will adapt as we learn more. And hey, even typos happen, but the science stays solid.
kevin burton
November 5, 2025 AT 18:32 PMThe key takeaway is that PPIs raise gastric pH for many hours, which can cut the absorption of weak‑base drugs such as atazanavir and dasatinib. H2‑RAs have a shorter effect, so the impact is usually less severe. Staggering doses, switching to an H2‑RA, or using pH‑independent formulations are practical ways to handle the problem. Simple pharmacist review can catch most unsafe combos.
Max Lilleyman
November 16, 2025 AT 23:59 PMHonestly, the data speaks for itself – PPIs are the main culprits, and the numbers are huge 😱. If you’re not careful, you’ll end up with sub‑therapeutic levels and treatment failure. 💊🚫 Check those drug‑interaction alerts before you reach for that OTC heartburn relief! 👍
Buddy Bryan
November 28, 2025 AT 05:26 AMYou're right to point out the cascade effect, but we need to be brutal about the numbers: up to an 80 % drop in AUC for some agents is not a trivial matter. Clinicians should enforce strict guidelines – no PPI for atazanavir, at the very least. Also, the literature shows that a 2‑hour gap only recovers about 30 % of exposure, so relying on timing alone is risky. I’d push for electronic alerts and pharmacist oversight as mandatory steps, not optional. The stakes are too high to stay complacent.
Jonah O
December 9, 2025 AT 10:52 AMEver notice how the pharma giants love to hide the fact that they design drugs to be vulnerable to acid‑reducers? It's like a secret recipe to keep us dependent on their next‑generation pH‑independent pills. They claim it's about safety, but really it's a control mechanism. The AI prediction tools they tout are probably just a façade to sell more software. Stay skeptical – the system is engineered to profit from our confusion.
Benjamin Sequeira benavente
December 20, 2025 AT 16:19 PMLet's turn this knowledge into action! 🚀 If you're on a PPI and a weak‑base medication, schedule a medication review ASAP. Talk to your pharmacist – they can suggest switching to an H2RA or adjusting the dose. Remember, empowerment comes from taking charge of your regimen, not letting the pills dictate your health. Keep pushing for those EHR alerts to be active, and don't settle for vague advice. Your health deserves aggressive advocacy!
Shannon Stoneburgh
December 31, 2025 AT 21:46 PMThis conspiracy angle is overblown. The data on interaction is solid and reproducible, not hidden. Pharmacists already flag risky combos. Let's focus on practical steps rather than speculation.
Nathan Comstock
January 12, 2026 AT 03:12 AMFrankly, this whole discussion about acid reducers is just a distraction from the real issue: patients need to take responsibility for their meds! The guidelines are clear, the studies are out there, and yet people keep ignoring them. If you want optimal therapy, ditch the PPIs unless absolutely necessary. It's simple common sense – no more excuses!
Terell Moore
January 23, 2026 AT 08:39 AMHow quaint it is that we still debate the mechanisms of gastric pH while the literature has already distilled the phenomenon into a handful of tables. One would think that the modern clinician, armed with decision‑support systems, would have transcended these elementary concerns. Yet here we are, rehashing the same points ad nauseam. Perhaps a deeper philosophical inquiry into the nature of pharmaceutical hegemony is required, though I suspect most will remain content with surface‑level compliance. In any case, the data remains immutable.
Amber Lintner
February 3, 2026 AT 14:06 PMOh, please! As if your lofty musings make the interaction any less real. The patients suffer because you hide behind jargon and “philosophical inquiry.” It's not about being profound; it's about saving lives. Your sarcasm does nothing but mask the urgency.
Lennox Anoff
February 14, 2026 AT 19:32 PMIt is incumbent upon us, as custodians of medical wisdom, to interrogate the very foundations upon which these pharmacological interactions rest. The first point to consider is the biochemical rationale: gastric pH modulation unequivocally alters the ionization state of weak bases, thereby affecting their solubility and, consequently, their bioavailability. Yet, many prescribers treat this as an ancillary concern rather than a central tenet of therapeutic strategy. Second, the epidemiological evidence is stark; a substantial proportion of treatment failures can be directly traced to concurrent acid‑reducing therapy. Third, the regulatory landscape offers guidance, but adherence is inconsistent. Fourth, the advent of electronic health records promises automated alerts, but the fidelity of these alerts is variable, leading to alert fatigue. Fifth, patient education remains woefully inadequate, with many individuals unaware that over‑the‑counter PPIs can sabotage their prescription regimens. Sixth, the economic implications are non‑trivial, as sub‑optimal drug exposure precipitates additional healthcare utilization. Seventh, the pharmaceutical industry is already innovating pH‑independent formulations, suggesting an awareness of the problem at the development stage. Eighth, clinicians must balance the necessity of acid suppression against the risk of drug interaction on a case‑by‑case basis. Ninth, the clinical community should champion stewardship programs that routinely review acid‑reducing drug use. Tenth, interdisciplinary collaboration between pharmacists, physicians, and patients is essential to mitigate these risks. Eleventh, future research should prioritize individualized gastric pH profiling to tailor therapy. Twelfth, educational curricula should embed these pharmacokinetic concepts early in training. Thirteenth, policy makers ought to incentivize the discontinuation of unnecessary PPIs. Fourteenth, we must not overlook the role of lifestyle modifications in reducing acid‑related complaints. Fifteenth, the moral imperative remains clear: we must safeguard therapeutic efficacy by rigorously managing acid‑reducing medication use.