Gene therapy isn’t just another treatment option-it’s a rewrite of your body’s code. Instead of managing symptoms with pills, it tries to fix the root cause by delivering working genes into your cells. But here’s the catch: once you introduce a new genetic instruction into your body, everything else-medications, immune responses, even your liver’s ability to process drugs-can change in ways we’re still learning to predict.
Why Gene Therapy Isn’t Like Taking a Pill
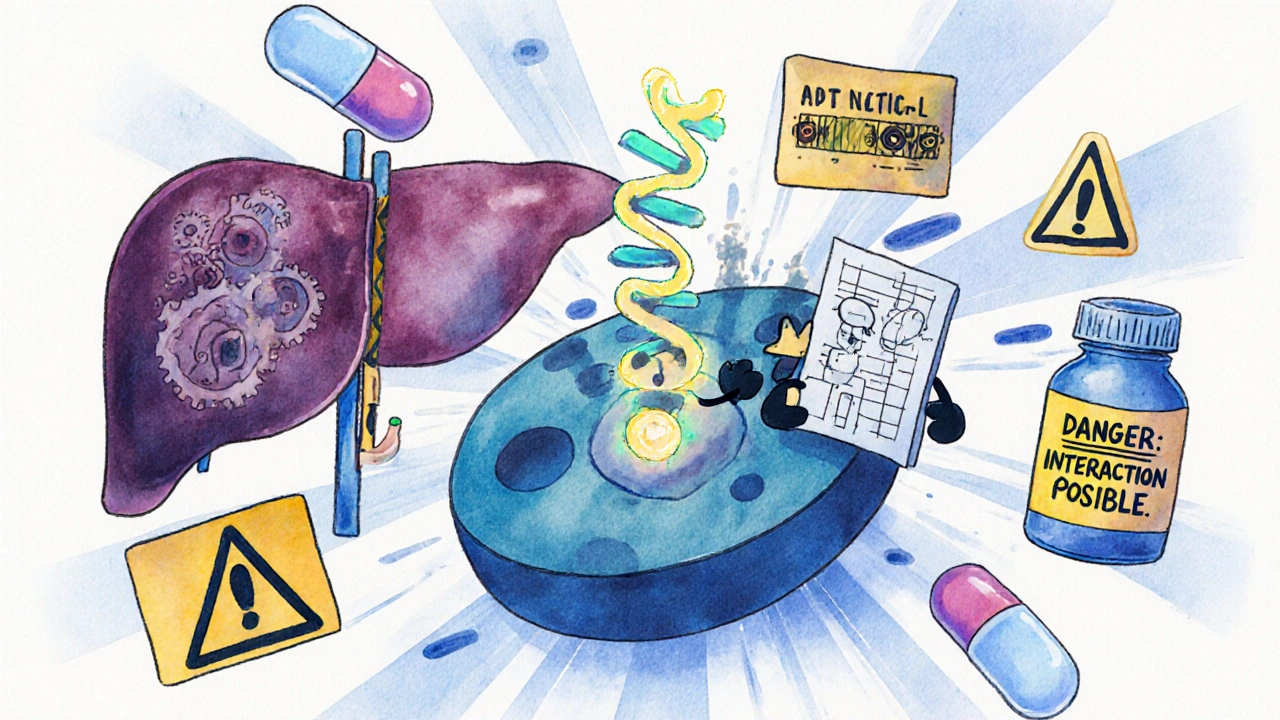
Most drugs work temporarily. You take a statin, it lowers cholesterol for a day or two. You stop, it fades. Gene therapy is different. It’s meant to last. Some therapies insert new DNA directly into your cells, turning them into tiny drug factories that keep producing proteins for years, maybe even decades. That permanence is powerful-but it’s also risky.Imagine you’re on blood thinners. You’ve been stable for years. Then you get a gene therapy treatment using an adeno-associated virus (AAV) to fix a rare liver disorder. A few weeks later, your INR levels spike. Why? The viral vector triggered an immune response that temporarily shut down your liver’s CYP3A4 enzyme-the same enzyme that breaks down warfarin. Your blood thinner is now building up to dangerous levels, and your doctor didn’t see it coming because no one’s tracked this exact interaction before.
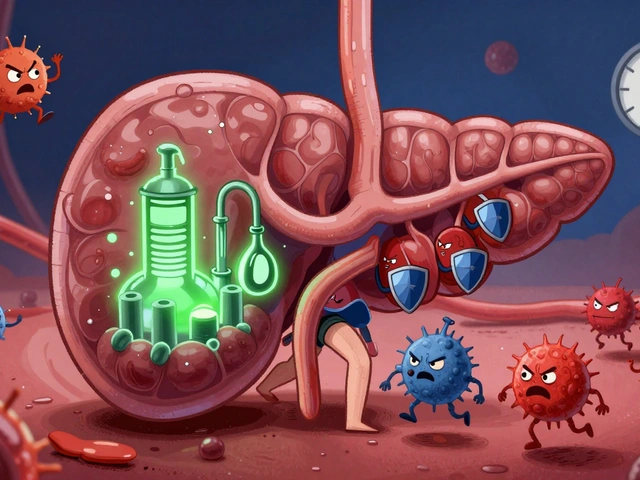
This isn’t hypothetical. In clinical trials, patients receiving AAV-based therapies have shown unexpected changes in how their bodies handle common drugs like antidepressants, anticonvulsants, and even over-the-counter painkillers. The immune system, startled by the viral vector, starts pumping out cytokines. Those inflammatory signals can dial up or dial down liver enzymes that metabolize 80% of all prescription drugs. And because every person’s immune system reacts differently, there’s no one-size-fits-all warning.
The Ghosts of Past Failures
The first big warning sign came in 1999. Jesse Gelsinger, an 18-year-old with a rare metabolic disorder, died after receiving a gene therapy using an adenovirus vector. His immune system overreacted. Within days, his organs failed. Autopsies showed massive inflammation in his liver. What made it worse? Earlier tests on monkeys had already shown the same deadly reaction-but it was dismissed as an outlier.Then, between 1999 and 2002, five children in gene therapy trials for SCID-X1-a condition that leaves babies without an immune system-developed leukemia. Why? The therapy used gamma-retroviral vectors that slipped the new gene right into the LMO2 gene, a known cancer trigger. The treatment fixed their immune deficiency… but accidentally turned on a tumor switch.
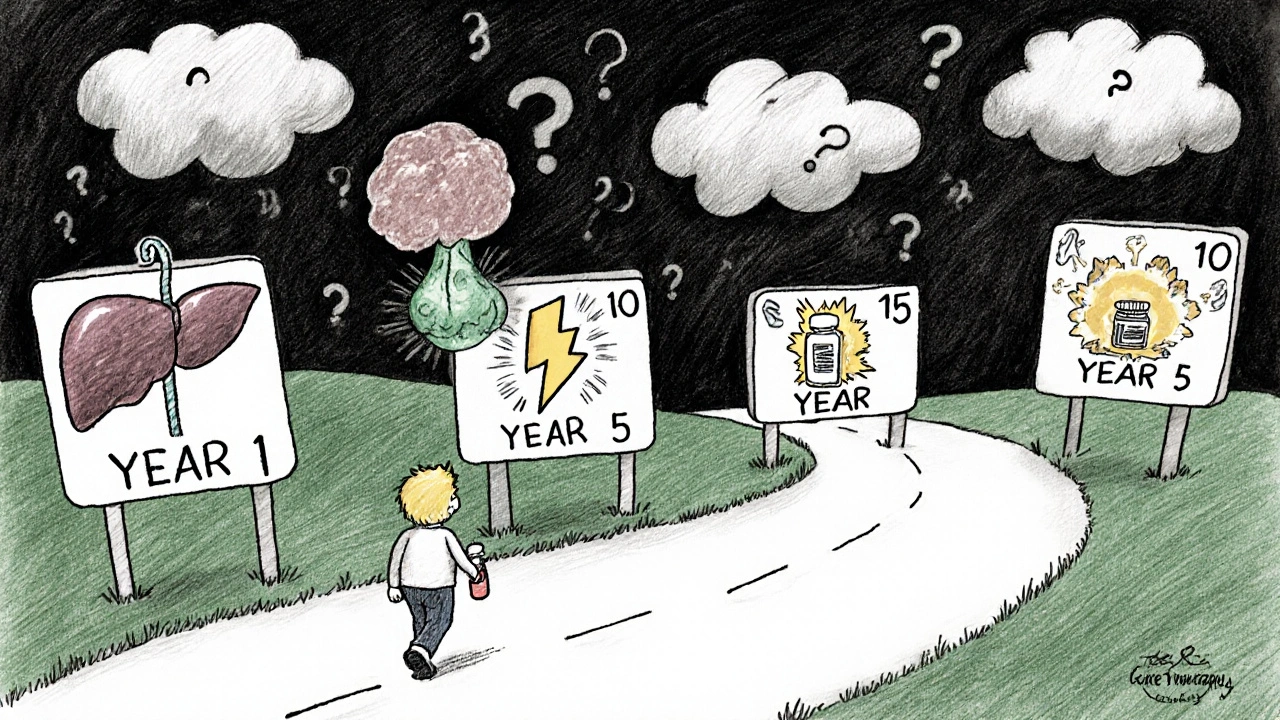
These weren’t just accidents. They were lessons written in blood. Today, regulators require 15 years of follow-up for any gene therapy that integrates into the genome. Why 15 years? Because cancer or organ damage might not show up for a decade. And if you’re on other medications during that time? Those interactions could speed things up-or hide the warning signs.
How Viral Vectors Mess With Your Drugs
There are three main types of viral vectors used today: adenoviruses, lentiviruses, and AAVs. Each behaves differently-and each interacts with drugs in its own way.- Adenoviruses trigger strong immune responses. They’re great for short-term expression but dangerous if you’re already on immunosuppressants or steroids. The combo can lead to cytokine storms or mask signs of infection.
- Lentiviruses integrate into your DNA. They’re used in CAR-T therapies and blood disorders. But if you’re taking chemotherapy or antivirals, the timing matters. Some drugs can kill the modified cells before they even start working.
- AAVs are the most common today. They don’t integrate, so they’re seen as safer. But they still cause immune reactions. And here’s the kicker: if you’ve been exposed to AAVs naturally (which many people have), your body might already have antibodies that neutralize the therapy before it even starts.
Even more complicated: AAVs can accumulate in the liver, spleen, and even the brain. If your liver is now packed with viral particles, it can’t process drugs the way it used to. That means drugs like acetaminophen, which are normally safe, can become toxic. Or worse-drugs that rely on liver enzymes to activate (like codeine) might not work at all.
Off-Target Effects and Hidden Drug Interactions
Gene therapy isn’t always precise. Even the best tools can accidentally edit the wrong gene. That’s called an off-target effect. And if that wrong gene happens to be one involved in drug metabolism? You’ve created a new kind of patient.For example, if a therapy accidentally edits the CYP2D6 gene-which affects how 25% of all drugs are broken down-you might suddenly become a poor metabolizer. A standard dose of antidepressant could make you dizzy. Or if you’re on beta-blockers for heart disease, you could get dangerously low blood pressure.
And what about cell therapies? Some gene therapies involve removing your cells, editing them in a lab, and putting them back. Those cells might migrate. A modified immune cell could end up in your gut and start producing a protein that changes how your body absorbs oral meds. No one’s studied this yet. But it’s already happening in trials.
The 15-Year Shadow
The FDA now requires 15 years of follow-up for integrating therapies. That’s not a suggestion-it’s a legal requirement. Why? Because the real danger isn’t in the first month. It’s in the fifth year, when a child who got gene therapy for spinal muscular atrophy starts having unexplained seizures. Or when a man who received a liver-targeted therapy for hemophilia develops liver cancer at age 45.Here’s the problem: during those 15 years, patients will likely take dozens of medications. Antibiotics for infections. Painkillers after surgery. Hormone replacements. Antidepressants. Each one could interact with the lingering effects of the gene therapy. And because we don’t have a database of these interactions, doctors are flying blind.
One study tracked 87 patients who received AAV gene therapy for inherited blindness. Five years later, 12% showed altered liver enzyme levels. None of them were on liver-affecting drugs. But when researchers checked their medication logs, they found that 7 of those 12 had recently taken statins. The statins weren’t the cause-but the gene therapy had made their livers more sensitive to them.
What Doctors Don’t Know Yet
There’s no checklist for gene therapy drug interactions. No database. No algorithm. No warning label on your prescription that says, “May interact with gene therapy.”Pharmacists don’t know how to flag it. Electronic health records don’t have a field for “received AAV gene therapy in 2023.” And most patients don’t realize they need to tell every new doctor they see-even a dermatologist for a rash-that they had gene therapy two years ago.
The tools to predict these interactions don’t exist yet. We don’t know how age, genetics, or prior infections affect the risk. We don’t know if taking ibuprofen before therapy changes the immune response. We don’t know if antibiotics wipe out the vector before it delivers its payload.
Right now, the best advice is simple: if you’ve had gene therapy, tell every doctor you see. Keep a written record of what therapy you got, when, and what vector was used. Bring that list to every appointment. And if you’re starting a new medication, ask: “Could this interact with gene therapy?”
The Path Forward
The field is moving fast. Companies are now building registries to track long-term outcomes. Researchers are developing blood tests to measure immune response to vectors before giving a drug. Some labs are creating AI models that predict drug-gene therapy interactions based on a patient’s genome and immune profile.But until those tools are ready, the burden falls on patients and doctors. Gene therapy is no longer science fiction. It’s in clinics. It’s saving lives. But it’s also opening a new frontier of risk-one where the rules haven’t been written yet.
The safest thing you can do? Stay informed. Ask questions. And never assume a drug is safe just because it’s been on the market for years. In the world of gene therapy, yesterday’s safe drug might be tomorrow’s hidden danger.
Can gene therapy cause long-term drug interactions?
Yes. Because gene therapy can permanently alter how your cells function-including liver enzymes that break down drugs-interactions can appear years after treatment. The FDA requires 15 years of follow-up for integrating therapies because risks like cancer or metabolic changes may not show up until long after the treatment.
Do I need to tell my doctor if I’ve had gene therapy?
Absolutely. Every doctor, dentist, and pharmacist you see should know. Gene therapy can change how your body processes common medications like painkillers, antidepressants, and blood thinners. Many providers aren’t trained to recognize these interactions, so it’s up to you to bring up your treatment history.
Are all gene therapies the same in terms of drug interactions?
No. Different viral vectors (like AAV, adenovirus, or lentivirus) trigger different immune responses and affect organs differently. AAV therapies often impact the liver, while lentiviral therapies used in blood disorders can alter bone marrow function. Each type has its own interaction profile, and mixing them with drugs requires case-by-case evaluation.
Can gene therapy make me more sensitive to side effects from medications?
Yes. The immune response triggered by the viral vector can make your liver more sensitive to drugs, change how your kidneys filter medications, or alter the way your body absorbs pills. Even something as simple as ibuprofen can become more likely to cause stomach bleeding or kidney stress after gene therapy.
Is there a database of known gene therapy-drug interactions?
Not yet. There’s no centralized database tracking these interactions because the therapies are too new and too varied. Clinical trials rarely collect detailed drug interaction data. Patients are encouraged to report side effects to regulators like the FDA, but systematic tracking is still in early stages.




Nicole M
November 12, 2025 AT 19:16 PMSo let me get this straight - if I get gene therapy tomorrow, I can’t take Advil for a headache five years from now without risking liver damage? And no doctor will know unless I remember to mention it? That’s insane. We’re basically creating a new class of medical orphans.
Arpita Shukla
November 14, 2025 AT 17:51 PMActually, it’s worse than that. The CYP450 system is already wildly variable between individuals - add a viral vector that alters enzyme expression unpredictably, and you’ve got a pharmacogenomic nightmare. I’ve seen patients on stable warfarin regimens crash after AAV therapy because their INR spiked without warning. No one had a baseline. No one thought to test.
And don’t even get me started on how AAV seroprevalence varies by geography. Someone in India might have pre-existing immunity that blocks therapy entirely, while someone in the US gets full transduction. But both end up with the same ‘gene therapy’ label in their chart. That’s not precision medicine. That’s lottery medicine.
Benjamin Stöffler
November 16, 2025 AT 13:04 PMAnd yet… we’re still treating gene therapy like a magic bullet - a one-time fix that absolves us of responsibility for long-term care. But what is a human being, if not a dynamic system of biochemical feedback loops? To insert a permanent genetic instruction into that system - without understanding how it will interact with every pill, every infection, every stressor - is not science. It’s metaphysical hubris. We’re playing God with enzymes, and then acting shocked when the altar catches fire.
And the 15-year follow-up? That’s not a safeguard - it’s a confession. We know we don’t know. We just hope nobody dies before the paperwork is filed.
Mark Rutkowski
November 17, 2025 AT 18:42 PMThere’s something beautiful here, even in the chaos. Gene therapy isn’t just changing how we treat disease - it’s forcing us to rethink what it means to be a patient. You’re not just taking a drug anymore. You’re becoming a living, breathing pharmacology experiment. And that’s terrifying - but also kind of sacred.
Imagine being the person who, five years from now, takes a simple painkiller and realizes - this isn’t the same body I had before. My liver remembers the virus. My cells remember the edit. I’m not just managing symptoms anymore. I’m living with a permanent rewrite. That’s not medicine. That’s evolution - and we’re the first generation to choose it.
Ryan Everhart
November 17, 2025 AT 19:46 PMSo… we’ve got a therapy that can permanently alter your drug metabolism, but no one’s putting a checkbox in EHRs? No alerts? No pharmacist flags? Cool. So if I get a liver transplant and then gene therapy, and then need antibiotics, who’s gonna tell the ER doc I’m basically a walking drug interaction?
Meanwhile, the FDA’s like, ‘15 years of follow-up!’ Yeah, sure. But what if I move countries? Change doctors? Die of a car crash in year 7? Guess we’ll never know if that statin killed me - or the gene therapy made my liver hate it.
David Barry
November 19, 2025 AT 10:00 AMLet’s be real: this whole ‘gene therapy safety’ thing is a PR stunt. The companies know the risks. They just don’t want to admit it until after they’ve sold 10,000 treatments at $2M a pop. The ‘15-year follow-up’? That’s not for patient safety - it’s for liability shielding. By the time the cancer shows up, the patent’s expired and the company’s moved on to the next miracle cure.
And don’t even get me started on the ‘tell every doctor’ advice. You think a dermatologist cares that you got AAV therapy? They’re prescribing hydrocortisone for a rash. They don’t care if your liver’s a ticking time bomb.
Alyssa Lopez
November 21, 2025 AT 01:52 AMGene therapy is the future and if you cant handle the side effects then dont get it. We dont need to coddle patients with ‘oh no your liver might be sensitive to tylenol’ nonsense. This is cutting edge science - if you want to be a guinea pig then you sign the waiver. End of story. Stop whining about drug interactions like its a coffee allergy.
Alex Ramos
November 22, 2025 AT 13:14 PMJust wanted to add - if you’ve had gene therapy, keep a physical copy of your treatment info. I work in a clinic and we had a guy come in after a car accident. He was on blood thinners, had a liver injury, and we almost gave him a full dose of morphine. Turned out he had AAV therapy 3 years prior - his CYP3A4 was down 70%. We almost killed him because no one knew to ask. Bring a card. Write it on your phone. Tell your mom. Do whatever it takes.
Also, if you’re on meds, get a baseline liver panel before therapy. And recheck it 6 months after. It’s not rocket science - just common sense.
edgar popa
November 24, 2025 AT 04:30 AMYea i got the therapy last year and i still take ibuprofen for my back. nothin happened. maybe its just me tho.
manish kumar
November 25, 2025 AT 00:56 AMWhat nobody’s talking about is the global inequity here. The therapies are priced at $2M because they’re designed for wealthy, well-monitored patients in the U.S. and EU. But what about someone in India or Nigeria who gets a cheaper version - or worse, an unregulated one? Their liver enzymes aren’t tracked. Their meds aren’t logged. Their doctors don’t even know what AAV stands for. We’re creating a two-tiered system where the rich get monitored for decades, and the poor get a genetic gamble with no safety net.
And let’s be honest - the real danger isn’t the science. It’s the system. We’re rushing this into clinics because it’s profitable, not because we’re ready. We’ve got AI models being built to predict interactions, but they’re trained on data from 500 white, middle-class Americans. What happens when your genome is different? Your immune history is different? Your access to care is different? The algorithm doesn’t care. It just spits out a risk score based on data that doesn’t include you.
And yet, we’re still asking patients to be their own advocates. ‘Tell every doctor!’ Yeah, right. Try telling that to a single mom working two jobs, who just got her kid’s gene therapy approved and now has to navigate insurance, travel, and a new set of medical risks - all while her primary care doc has never heard of CYP2D6.
This isn’t just a medical problem. It’s a social justice crisis wrapped in a lab coat. We celebrate the breakthroughs, but we ignore the infrastructure that’s supposed to protect the people who make those breakthroughs possible. We’re building a future where your body is a living database - but we’re not even giving you the password to read it.
Until we fix that, gene therapy won’t be a cure. It’ll be a privilege.
Eve Miller
November 25, 2025 AT 06:18 AMYou all are missing the point. The real issue isn’t drug interactions - it’s consent. How many patients truly understand that gene therapy alters their biology permanently? How many read the 87-page informed consent form? How many realize that their children, decades from now, could inherit epigenetic changes from this treatment? This isn’t medicine. It’s genetic experimentation - and we’re doing it without ethical guardrails, without transparency, and without public accountability. If you’re not outraged, you’re not paying attention.