When your skin acts up, it’s easy to assume it’s just eczema, a chronic inflammatory condition that causes dry, itchy patches, often in folds of the skin. Also known as atopic dermatitis, it’s one of the most common skin issues—but it’s not the only one. Many people mistake psoriasis, an autoimmune disorder that triggers thick, scaly plaques, usually on elbows, knees, and scalp. Also known as plaque psoriasis, it often runs in families and doesn’t itch as much as eczema. Or they think their red, flushed face is just sunburn, when it’s actually rosacea, a persistent facial redness with bumps and visible blood vessels, often triggered by heat, alcohol, or stress. Also known as facial vascular disorder, it’s frequently misdiagnosed as acne or allergic reaction. These aren’t just different names for the same thing—they’re distinct conditions with different causes, treatments, and long-term impacts.
Then there’s contact dermatitis, a reaction to something your skin touched—like poison ivy, nickel in jewelry, or harsh soaps. Also known as allergic or irritant dermatitis, it shows up as a red, blistering rash right where the substance made contact. Unlike eczema or psoriasis, it usually clears up once you avoid the trigger. But if you keep using the same soap, lotion, or laundry detergent, it’ll come back. And then there’s fungal infections like ringworm, which looks like a circular red patch but needs antifungal cream, not steroid ointment. Mixing these up can make things worse. Using steroid creams on a fungal infection can spread it. Using antifungals on psoriasis won’t help at all. The wrong treatment doesn’t just waste time—it can cause more irritation, scarring, or even secondary infections.
What you see in the mirror isn’t always what’s going on underneath. A rash that flares after stress? Could be eczema or psoriasis. Burning and stinging instead of itching? More likely rosacea. A patch that spreads after you changed your detergent? Probably contact dermatitis. The patterns matter. The location matters. The timing matters. And so does your family history. You don’t need a medical degree to spot the clues—you just need to know what to look for. Below, you’ll find real comparisons from actual cases: how one person’s itchy elbows turned out to be psoriasis, not eczema; how a persistent red nose was rosacea all along; how a "allergy" that wouldn’t go away was actually a reaction to a new shampoo. These aren’t theory—they’re stories from people who got it wrong first, then learned how to fix it.
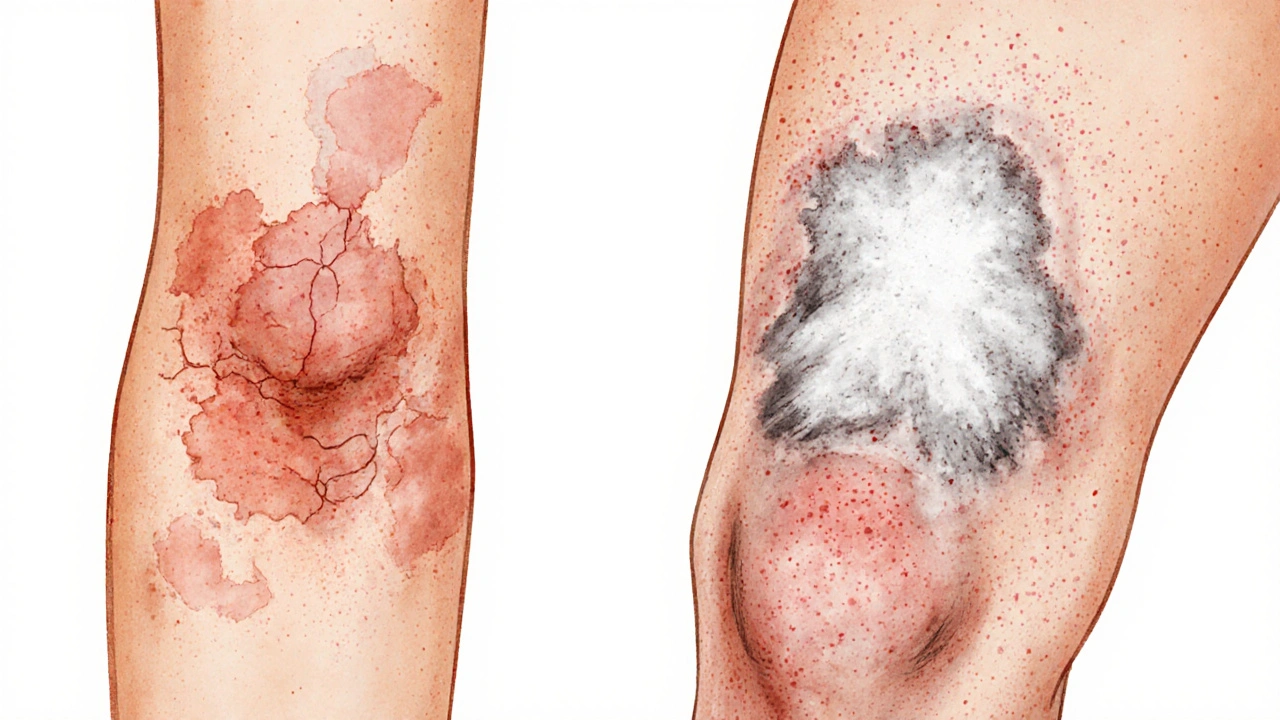
Learn how to tell eczema and psoriasis apart by their rash appearance - location, texture, scaling, and how they look on different skin tones. Key differences that help avoid misdiagnosis.
read more