Insulin Injection Site Rotation Planner
Injection Site Rotation Guide
Proper site rotation is crucial for preventing lipohypertrophy and bruising. This tool helps you track your injection sites and plan your rotation schedule effectively.
Log New Injection
Rotation Status
When you’ve been giving yourself insulin for months or years, you might not think twice about where you inject. But those little bumps, lumps, or bruises on your stomach, thighs, or arms? They’re not harmless. They’re signs of lipodystrophy and bruising-common, avoidable problems that can wreck your blood sugar control without you even realizing it.
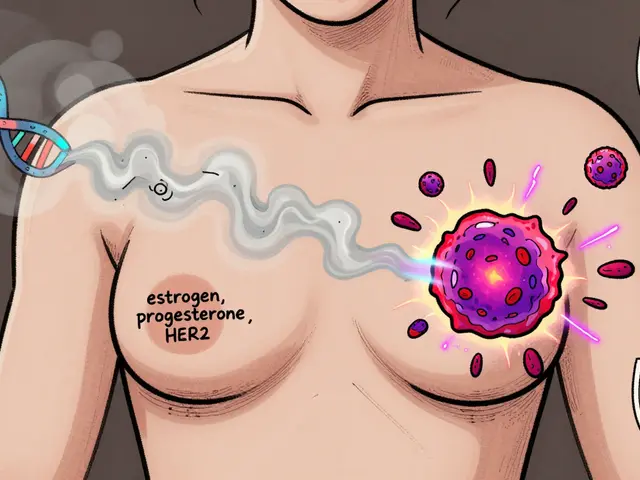
What Exactly Is Lipodystrophy?
Lipodystrophy isn’t one thing. It’s two opposite problems that both come from repeated insulin injections in the same spots. One is lipohypertrophy: fat builds up under the skin, creating soft, rubbery lumps. The other is lipoatrophy: fat disappears, leaving shallow dents or pits. Both mess with how insulin gets absorbed-and that means your blood sugar goes haywire.Lipohypertrophy is far more common. Studies show up to half of people using insulin develop it at some point. It usually shows up on the abdomen-78% of cases-because that’s where most people inject. These lumps aren’t red or hot. They don’t hurt. That’s why people miss them. In fact, many patients actually prefer injecting into these lumps because they feel less pain. Big mistake. Insulin absorbed from these areas is slow, uneven, and unpredictable. You might think you’re giving the same dose, but your body gets less-or too much-without warning.
Lipoatrophy is rarer now, mostly because modern insulin formulations don’t trigger it as much as older ones did. Still, it happens. It looks like a small, sunken spot. It’s not a bump. It’s a hole. And yes, it also messes with insulin absorption. Both types of lipodystrophy are linked to poor injection habits-not to the insulin itself.
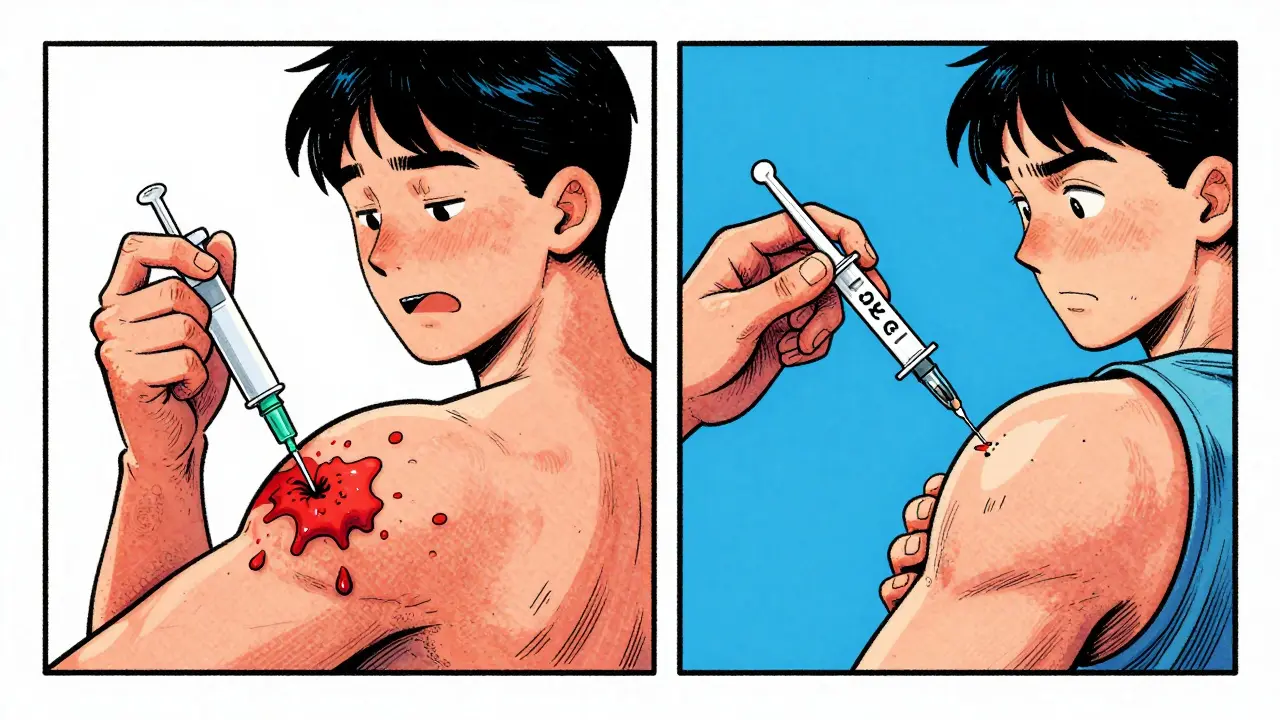
Why Bruising Happens (And Why It’s More Than Just a Blotch)
Bruising after an insulin shot isn’t rare. One study found nearly 66% of insulin users had visible bruising at some point. It’s not always from hitting a vein. Often, it’s from pressing too hard on the pen, using a dull needle, or reusing needles. A 31-gauge needle is fine. Reusing it five times? Not fine. Each reuse blunts the tip. That means more tissue damage. More bleeding. More bruising.Some people think bruising is just a one-off. It’s not. Repeated bruising in the same spot is a warning sign. It’s your body saying, “This area is getting damaged.” And over time, that damage can turn into lipohypertrophy. Think of bruising as the first stage of tissue breakdown. Ignore it, and you’re setting yourself up for bigger problems down the road.
How Lipodystrophy and Bruising Ruin Your Blood Sugar
This is the part most people don’t get. You’re doing everything right-counting carbs, checking glucose, taking your insulin on time-but your A1c keeps creeping up. Or worse, you’re getting unexplained low blood sugars. That’s not bad luck. That’s lipodystrophy.Insulin absorbed from a lipohypertrophic lump doesn’t enter your bloodstream the way it should. It’s delayed. Sometimes it takes hours. Other times, it comes out all at once. That leads to wild swings: high glucose after meals, then sudden drops hours later. One study found people with undiagnosed lipohypertrophy had 3.2 times more unexplained hypoglycemia and 2.7 times more episodes of diabetic ketoacidosis.
And here’s the kicker: you might need 20-30% more insulin to get the same effect if you’re injecting into lumps. That means higher doses, higher costs, and more risk of weight gain. It’s a vicious cycle. You inject in the same spot because it’s less painful. You get a lump. You need more insulin. The lump grows. You keep injecting there. Rinse and repeat.
How to Spot Lipodystrophy-Even If You Can’t See It
You can’t always see lipohypertrophy. Especially if you’re pale or have darker skin. That’s why feeling matters more than looking.Here’s how to check your injection sites every time you prep:
- Use your fingertips. Gently press around your usual spots-abdomen, thighs, arms, buttocks.
- Look for areas that feel firmer, thicker, or rubbery compared to the skin around them.
- Don’t ignore areas that feel different even if they look normal.
- Compare both sides. If one side feels lumpier, mark it and avoid it.
- If you find a lump bigger than an inch across, stop injecting there. Ever.
For lipoatrophy, you’re looking for indentations. A small depression that doesn’t bounce back. If you see or feel one, rotate away immediately.
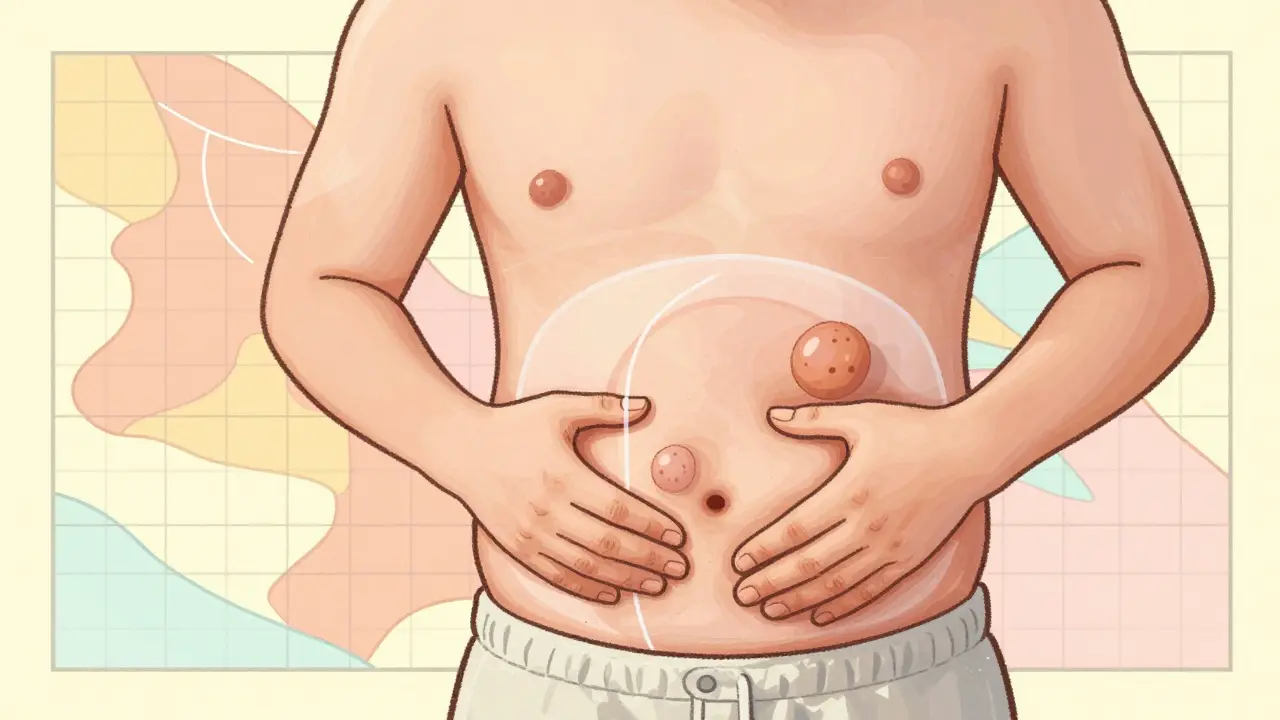
How to Rotate Sites Right-No Guesswork
Site rotation isn’t just “switch sides.” It’s a system. Here’s how to do it properly:- Divide your body into four zones: abdomen (avoid 2 inches around the navel), thighs, upper arms, and buttocks.
- Within each zone, divide into 1-inch squares. Think of it like a grid.
- Inject in one square, then move to the next. Don’t go back to a square until at least 4-8 weeks have passed.
- Use a different zone each day. For example: Monday-abdomen, Tuesday-thigh, Wednesday-arm, Thursday-abdomen again, but a different quadrant.
- Keep a simple log. A notebook, phone app, or even a sticky note on your fridge works.
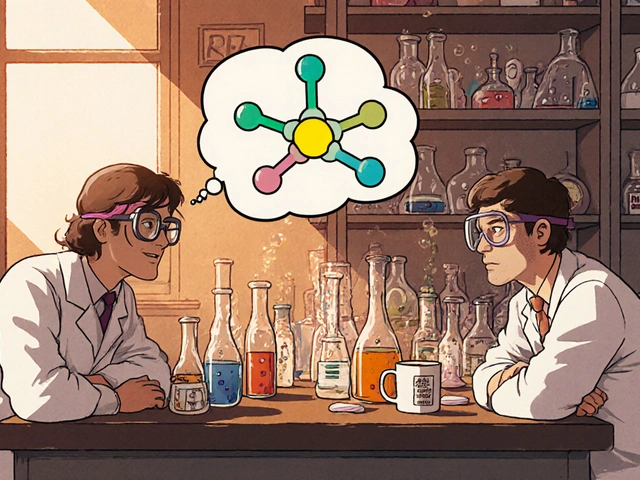
Apps like InPen or Glooko can map your injection sites automatically. They show you where you’ve injected and remind you when it’s safe to return. Users who used these tools saw a 31% drop in lipohypertrophy over six months.
Needle Tips That Actually Help
You don’t need fancy gear. But small changes make a difference:- Use a new needle every time. Seriously. Reusing needles increases bruising by 40% and raises lipohypertrophy risk.
- Go with 32G or 31G needles. Thinner means less tissue damage.
- Don’t rub the area after injecting. Just press gently for 5-10 seconds. Rubbing causes micro-tears and bleeding.
- Inject at a 90-degree angle if you have enough fat. If you’re thin, pinch the skin and inject at 45 degrees.
- Don’t inject into bruised, scarred, or swollen areas-even if they’re not lumpy. Give them time to heal.
What Your Doctor Should Be Checking (But Probably Isn’t)
Most people go years without their injection sites being checked. A survey found 61% of insulin users said their doctor never looked at their injection areas in five years. That’s unacceptable.Ask your doctor or diabetes educator to examine your sites at least once a year. If you’ve had high A1c, unexplained lows, or frequent bruising, ask for it every visit. They should be palpating your skin-not just asking if you’re rotating.
There’s no test for lipodystrophy. It’s diagnosed by touch. If your provider doesn’t know how to feel for lumps, ask for a referral to a certified diabetes educator. They’re trained to spot this.

Real Stories: What Works
One user on Reddit had a golf ball-sized lump on their abdomen after two years of injecting in the same spot. Their A1c jumped from 7.2% to 8.9%. They switched to a rotation system and started using a new needle every time. Three months later, their A1c dropped to 6.8%. They didn’t change their diet or meds. Just their injection technique.Another person, who bruised every time they injected, started pressing gently instead of jamming the pen into their skin. The bruising stopped in two weeks. No more black-and-blue marks. No more fear of injecting.
These aren’t miracles. They’re simple fixes. But they only work if you act.
What’s Changing in 2025
New tech is making this easier. Abbott announced at the ADA meeting in 2023 that they’re developing biosensors that can detect early tissue changes at injection sites-before lumps form. The goal? A patch or pump that tells you, “This area is stressed. Move.”Meanwhile, AI tools like Glooko’s site-mapping feature are already helping thousands. They track where you inject, warn you if you’re repeating too soon, and even suggest better spots based on your body type.
But tech won’t fix this alone. Education will. The International Injection Technique Group has grown from 12 to 37 countries since 2018. More clinics are training staff to check injection sites. More patients are learning to feel for lumps. That’s progress.
Bottom Line: This Is Your Responsibility
You’re the one injecting. You’re the one feeling the lumps. You’re the one seeing the bruises. No one else will notice unless you tell them. And if you don’t act, your blood sugar will keep swinging. Your risk of complications will climb. Your insulin will cost more. Your life will get harder.Fixing this doesn’t require a new drug. It doesn’t need a surgery. It just needs you to look. To feel. To rotate. To use a new needle. To say no to the easy spot.
Do that, and you’re not just avoiding lumps and bruises. You’re taking back control of your diabetes.
Can lipodystrophy go away on its own?
Yes-but only if you stop injecting into the affected area. Lipohypertrophy can shrink over months if you avoid it completely. Lipoatrophy may improve too, though it often leaves a permanent indentation. The key is patience and strict avoidance. Injecting into the same spot again will make it worse.
Is bruising from insulin dangerous?
Bruising itself isn’t dangerous, but it’s a red flag. It means you’re damaging tissue. Repeated bruising in the same spot increases your risk of developing lipohypertrophy. It’s not the bruise you need to worry about-it’s what it’s telling you about your technique.
Do I need to rotate sites if I use an insulin pump?
Absolutely. Pump users are actually at higher risk for lipodystrophy because the cannula stays in the same spot for days. Change your infusion site every 2-3 days, and rotate locations. Don’t use the same area within 4-8 weeks. Many pumps now have built-in rotation reminders-use them.
Can I inject into scar tissue?
No. Scar tissue doesn’t absorb insulin properly. It can cause erratic blood sugar swings and increase the risk of infection. Always avoid scars, even if they’re old or flat. Find a new spot.
Why do some people get lipodystrophy and others don’t?
It’s not about genetics. It’s about habits. People who reuse needles, skip rotation, or inject in the same small area every day are far more likely to develop it. Even people with type 1 diabetes who’ve been on insulin for 20 years can avoid it entirely with proper technique. The difference is consistency, not biology.
Should I use a different needle for each injection?
Yes. Reusing needles dulls the tip, increases pain, raises bruising risk, and damages tissue. It also increases the chance of infection. A new needle costs pennies. The cost of poor blood sugar control? Thousands of dollars a year.
How long does it take to see improvement after I start rotating?
You might notice fewer bruises in a week. Lipohypertrophy lumps take longer-often 3 to 6 months to shrink noticeably. But your blood sugar should stabilize faster. Many users report fewer unexplained lows within 2-4 weeks of proper rotation. Consistency is everything.




Paige Shipe
December 29, 2025 AT 15:40 PMLipodystrophy isn't even on most doctors' radar. I've been on insulin for 12 years and never once had someone check my injection sites. I found my own golf-ball lump by accident while stretching. No one warned me. No one cared. Now I rotate religiously. My A1c dropped from 8.4 to 6.9. It's not magic. It's just not being lazy.
Tamar Dunlop
December 30, 2025 AT 15:42 PMAs a Canadian living with type 1 diabetes since childhood, I am compelled to express my profound gratitude for this meticulously researched and deeply compassionate exposition. The clinical precision with which you delineate the pathophysiology of lipohypertrophy, coupled with the empathetic recognition of the psychological burden borne by those who inject daily, elevates this piece to the level of medical literature worthy of global dissemination. Thank you for speaking truth to the invisible suffering.
David Chase
December 31, 2025 AT 04:25 AMTHIS IS WHY AMERICA’S HEALTHCARE IS BROKEN 😤 You’re supposed to get educated on this stuff BEFORE you start injecting, not after you’ve got a damn golf ball under your skin! 🤬 Reusing needles? That’s not frugal-that’s reckless. 🚫💉 My cousin went blind because her doc never checked her sites. This isn’t ‘self-care’-it’s negligence wrapped in a Band-Aid. Stop normalizing bad habits. #DiabetesEmergency
Emma Duquemin
January 1, 2026 AT 20:25 PMOH MY GOODNESS. I just read this and I’m crying. Not because it’s sad-because it’s so DAMN CLEAR. I used to inject into the same spot on my thigh because it ‘felt right.’ I thought bruising was normal. Turns out, I was basically giving my body a slow-motion beating. I started rotating last month. No more purple patches. My fasting sugars dropped 30 points. I feel like I’ve been handed back my life. If you’re reading this and you’re still injecting in the same three inches? STOP. Just stop. Go feel your skin right now. You might be surprised. You’re worth more than convenience.
Kevin Lopez
January 2, 2026 AT 07:17 AMLipohypertrophy = altered pharmacokinetics. Subcutaneous adipose tissue remodeling → delayed insulin absorption → glycemic variability. Evidence: meta-analysis by Hirsch et al., 2021. Needle reuse = increased tissue trauma. 31G > 32G for penetration efficiency. Rotation protocol: 1-inch grid, 4–8 week recurrence interval. Pump users: cannula site change every 72h max. Compliance correlates inversely with HbA1c variance. QED.
Samar Khan
January 2, 2026 AT 16:30 PMWhy do people still reuse needles?? 😒 I saw someone do it at the pharmacy and I wanted to scream. It’s not saving money-it’s costing you your kidneys. Bruising = tissue damage = future lumps. You think you’re being smart? You’re just being stupid. 🤦♀️
Russell Thomas
January 4, 2026 AT 04:16 AMWow. So the solution to decades of poor diabetes management is… to touch your skin? And use a new needle? Groundbreaking. I bet the pharmaceutical companies are shaking in their boots. Next you’ll tell us we should brush our teeth. 🙄
Joe Kwon
January 5, 2026 AT 02:09 AMI’ve been using the Glooko app for rotation tracking since last year. It’s not perfect, but it’s saved me from reusing spots. I used to ignore the warnings-now I listen. My A1c went from 7.8 to 6.5. I’m not a genius. I just followed the system. If you’re skeptical, try it for 30 days. You’ll see the difference before your next doctor visit. No hype. Just data.
Nicole K.
January 6, 2026 AT 14:21 PMIf you’re reusing needles, you’re selfish. You’re not just hurting yourself-you’re risking your family’s future. Think about your kids. Think about your parents. This isn’t a personal choice. It’s a moral failure.
Amy Cannon
January 8, 2026 AT 11:45 AMIt is with profound solemnity that I reflect upon the gravity of this subject matter, as it pertains to the corporeal integrity of those who navigate the daily exigencies of insulin therapy. The subtle, insidious nature of lipodystrophy-often imperceptible to the untrained eye, yet devastating in its metabolic consequences-demands not merely awareness, but institutionalized vigilance. One cannot help but lament the systemic failure of medical practitioners to prioritize tactile examination of injection sites as a fundamental component of routine diabetes care. It is, frankly, an abdication of professional duty. The onus, however, must also rest upon the individual: to become the vigilant steward of one’s own physiology, to cultivate the discipline of rotation, to eschew the seductive ease of the familiar site. This is not merely medical advice-it is an act of self-respect.
Himanshu Singh
January 10, 2026 AT 03:44 AMReally helpful! I didn’t know lipoatrophy was still a thing. I thought it was only from old insulin. I’ve been injecting in same spot for 3 years 😅 Now I’m using app to track. Thanks for sharing!
Alex Ronald
January 11, 2026 AT 11:30 AMTwo years ago I had a lump the size of a lemon. My endo said, ‘Just rotate more.’ I didn’t believe it would help. I did it anyway. Six months later, it was gone. Not flat. Not gone. Just… gone. My insulin needs dropped 25%. I didn’t change a thing else. This isn’t theory. It’s biology. And it’s fixable.
Teresa Rodriguez leon
January 11, 2026 AT 15:42 PMI used to inject into my bruises because I was scared of the pain. Now I know it was making it worse. I stopped. The bruises faded. My blood sugar finally stabilized. I wish I’d known this sooner.