If you found a little pill that could cut the chance of breast cancer returning by almost half, you'd want to know everything about it, right? That's Tamoxifen—one of the heavy hitters in the world of cancer treatment. People call it the OG of hormone therapy drugs for breast cancer, and there's a good reason. First approved back in the 1970s, this medication is probably sitting in medicine cabinets of hundreds of thousands of women—and some men—across the world. It's one of those names that always pops up in cancer forums or when you ask an oncologist about keeping breast cancer under control. But despite its superstar rep, a ton of myths, hacks, and horror stories swirl around it. Let's get honest about what Tamoxifen actually does, how it really feels to take it, and what you can actually expect (without the sugarcoating).
How Tamoxifen Works in the Body
So here’s where the magic—and confusion—begins. Tamoxifen is what's called a Selective Estrogen Receptor Modulator, or SERM for short. But don't let the fancy label trip you up. The whole point of Tamoxifen is this: it sticks to estrogen receptors in breast cells so estrogen can’t do its job there. Why should you care? Well, with some breast cancers—what doctors call "estrogen receptor-positive" (ER+) cancers—estrogen acts like jet fuel, making those cells grow and spread faster. Tamoxifen pulls the fuel line so cancer can’t keep revving up.
Here's a simple image: imagine estrogen as a key that fits into a lock (the estrogen receptor) on breast cancer cells. When Tamoxifen jumps in, it jams the lock, making it impossible for the key to turn. That slows things down and gives your immune system—and other treatments—a fighting chance to clean up. But Tamoxifen isn’t just a blocker. In some tissues, like the bones or uterus, it acts like a weak form of estrogen. This is why some side effects feel weird and why it can actually help prevent osteoporosis after menopause. Back in the 1980s, researchers ran a game-changing study: after five years on Tamoxifen, women with ER+ breast cancer had a 49% lower risk of recurrence than those who took a placebo. Even the risk of dying from breast cancer dropped by 31%. Those are real numbers, not empty promises.
| Year | Number of Tamoxifen Prescriptions (USA) |
|---|---|
| 2000 | 6.5 million |
| 2010 | 4.8 million |
| 2023 | 5.2 million |
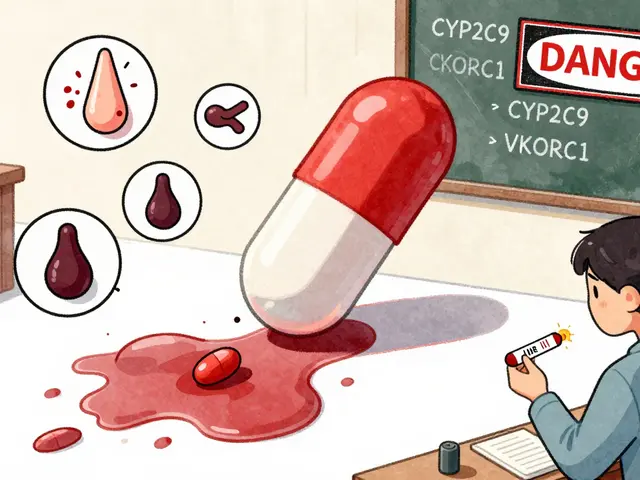
The way Tamoxifen gets handled in your body—absorbed, metabolized, and cleared—is mostly dictated by your liver. Genes play a part in whether you're a 'fast' or 'slow' metabolizer. Some folks get blood levels that are almost double what others get from the same dose. If you ever feel your side effects are wild compared to a friend, or you're not seeing results, your genes could be the culprit.
Who Benefits Most from Tamoxifen Therapy?
Tamoxifen is often labeled as a "women’s drug"—but that's just half the story. If you, or someone you care about, has been diagnosed with ER+ breast cancer (meaning their pathology report literally says these cells are estrogen-hungry), Tamoxifen is probably going to be on the table. It’s usually offered after surgery (lumpectomy or mastectomy) and sometimes after chemo or radiation. The goal: lower the odds of cancer coming back. If you haven’t reached menopause yet, Tamoxifen is usually the first choice over other hormone-blockers like aromatase inhibitors, because your ovaries are still pumping out lots of estrogen. Postmenopausal? You get more options, but Tamoxifen still works, especially for folks who can’t handle other drugs.
You might be surprised to learn that Tamoxifen isn’t just for women. Men with breast cancer (yep, it happens) or even those at high risk—like guys with BRCA2 mutations—get put on Tamoxifen, too. It’s also sometimes used to lower breast cancer risk in people who have never had it but are considered “high risk”—think strong family history, genetic mutations, or prior breast lumps that weren’t cancer but made doctors nervous. In a big UK prevention trial, Tamoxifen reduced the odds of getting breast cancer by around one-third in high-risk women. If you want the hard facts, here’s one: the standard Tamoxifen prescription is usually 20mg per day, taken for 5 to 10 years. That’s a long haul. But every year you stick with it, your protection gets better. For example, women who made it through 10 years saw their recurrence risk drop by an extra 25% compared to women who stopped at five years.
The Upsides: What Tamoxifen Can Really Do
If you want some stats to keep you motivated, Tamoxifen has helped drop breast cancer death rates by up to 40% since the late 1970s, according to cancer registries in Europe and the US. It’s the backbone of breast cancer survival for a good chunk of survivors worldwide. And this isn’t just about cutting down risk in the short term. The benefits of Tamoxifen persist even after you stop taking it. In one study, women who took it for five years had a 30% lower risk of developing a new breast cancer in the other (healthy) breast, and this benefit stuck for at least 15 years after stopping the drug. That’s some real staying power.
People sometimes freak out about the idea of taking “cancer drugs” for years, but Tamoxifen isn’t chemo. Most can take it at home, doesn’t require infusions, and you even get your hair to yourself. There are even some hidden bonuses: Tamoxifen is linked to denser bones in women after menopause, which helps fight off osteoporosis—a big problem if you’re already at risk for bone issues.
Doctors are starting to pay attention to prevention, too. If you have a monster family history or have tested positive for a BRCA mutation, Tamoxifen can actually lower your risk of ever developing breast cancer in the first place. For example:
- A 2019 study found Tamoxifen cut new breast cancer diagnoses by 44% in women with inherited BRCA1 or BRCA2 mutations.
- Some other non-cancer conditions, like severe gynecomastia (which is breast tissue growth in men), can respond to Tamoxifen as well.
But don’t run for the pharmacy yet. Like any good thing, there are catches. But the point is: if you’re looking for real, proven protection, there are few pills with a better track record for hormone-receptor-positive breast cancers.
Tamoxifen Side Effects: What You Might Actually Feel
Everybody wants to know the side effects, because let’s be real: nobody wants a new set of problems while trying to dodge cancer. Tamoxifen’s side effects range from odd to annoying to occasionally serious. The most talked about are “menopausal” symptoms. Think hot flashes, night sweats, and mood swings. Some people feel them strong, others barely notice. Want numbers? About 1 in 3 users will report significant hot flashes.
Other surprises include vaginal dryness, changes in periods (from lighter to stopping altogether), and sometimes reduced libido. Not sexy, but expected. There’s also the feeling of “brain fog” reported by some, and weirdly, leg cramps or muscle aches. Then there are emotional changes. Folks sometimes feel more anxious or a bit down. A lot of this comes from dropping estrogen levels, but if your moods feel out of control, it’s worth chatting with your doctor. Many people power through these—knowing the drug is stacking the odds in their favor.
There are rare but very real risks. Tamoxifen can slightly bump up the risk of blood clots—maybe up to 2-3% for certain people after years of use, which is still less than what many birth control pills carry. The risk for uterine cancer in postmenopausal women is about double, but the actual numbers are low (less than 1% over five years). You’ll usually get regular gynecological checks to spot anything early. If you notice sudden leg swelling or chest pain, it’s time to call your doc, not power through. For most people under 50 and without blood clot history, these serious side effects stay rare.
There’s a ton of talk online about Tamoxifen and weight gain. There’s no strong scientific proof that Tamoxifen itself makes you pack on pounds. But after treatment, bodies change, activity slumps, metabolism resets, and people can feel hungrier. You’ll want to be kind to yourself—track what’s changing, keep up activity, and connect with a dietitian if things get tough. Sometimes the routine of a daily pill can feel like a constant reminder of cancer, which takes a mental toll too. You’re not alone; support groups and counseling really help.

Tips for Thriving on Tamoxifen: Making Treatment Work for You
First things first: taking Tamoxifen is a marathon, not a sprint. Here are some tips straight from patients, nurses, and docs that can make things less rocky:
- Tamoxifen is best taken at the same time every day. Many go for evenings, especially if drowsiness is an issue. Setting a daily alarm or linking it with another habit (like brushing teeth) keeps things on-track.
- Hot flashes running wild? Cooling pillows, light layers, and avoiding caffeine or spicy foods at night can really help. Some find that yoga or paced breathing chills things out too.
- If sex or vaginal dryness is an issue, water-based lubricants make a world of difference. Don’t be embarrassed to ask for help. Doctors see this all the time.
- Keep moving. Regular exercise curbs a bunch of side effects, from mood dips to muscle pains. Even walks count. And bonus: it can stave off weight gain and boost bone strength.
- Stay up on appointments—blood work, liver tests, gynecology exams. These catch problems early before they become big headaches.
- Supplements? Ask your doctor before grabbing anything from the health food store. Some, like St. John’s Wort, can make Tamoxifen less effective by messing with your liver’s ability to process the drug.
- If you’re struggling with mood or sleep, don’t tough it out. Sleep meds, SSRIs, or therapy can make longer-term treatment much easier.
Double-check any new medication, even over-the-counter stuff, with your cancer team. Pain meds, antidepressants, or herbal supplements can sometimes block Tamoxifen from working right.
Another tip: if you simply can’t handle the side effects (and tried the hacks above), talk to your oncologist about dose changes or switching to another medication. Sticking with treatment—even at slightly lower doses—can keep your risk reduction on track and help you actually finish the course.
One last thing: Tamoxifen pills look identical year after year. If your pharmacy ever swaps to a new generic that feels or looks different, don’t panic—but definitely double-check the dose and manufacturer. For people super sensitive to even tiny changes, keep a med diary and bring it to each appointment.




Julia Phillips
July 5, 2025 AT 11:59 AMReading through this deep dive on Tamoxifen felt like watching a dramatic theatre of hope and fear. I can hear the whisper of countless women clutching that tiny pill like a lifeline. The way the drug blocks estrogen feels almost magical, yet the side‑effects can feel like a storm. It’s a reminder that survivorship is a brave, ongoing performance. Keep the facts coming, we need more honest stories.
Richa Punyani
July 9, 2025 AT 13:14 PMEsteemed colleagues, the comprehensive overview presented herein elucidates both the pharmacological mechanisms and the epidemiological impact of Tamoxifen with commendable clarity. The inclusion of statistical data enhances the credibility of the discourse. While the benefits are profound, it remains imperative to monitor the patient‑specific risk profile meticulously. I appreciate the balanced perspective offered.
Bhupendra Darji
July 13, 2025 AT 14:30 PMThanks for laying it all out; I think many folks just need the plain truth without all the jargon. It’s good to know that even men can benefit from Tamoxifen when they face this rare cancer. The tip about checking interactions with over‑the‑counter meds is spot on. Keep the practical advice coming.
Robert Keter
July 17, 2025 AT 15:46 PMTamoxifen’s role in the adjuvant setting cannot be overstated; it essentially rewires the hormonal landscape of estrogen‑receptor‑positive breast cancers, denying the tumor the proliferative signal it so desperately seeks. By occupying the estrogen receptor, it acts as a molecular roadblock, a fact that was first confirmed in clinical trials back in the 1980s and has since become a cornerstone of therapy. The durability of its effect is remarkable, with studies showing sustained risk reduction well beyond the five‑year treatment window, which is a testament to its long‑term imprint on cellular pathways. Moreover, the drug’s selective activity means that while it antagonizes estrogen in breast tissue, it can agonize receptors in bone, thereby conferring a protective effect against osteoporosis. This duality, however, comes with a trade‑off, as the partial estrogenic activity in the uterus raises a modest but real concern for endometrial hyperplasia. Patients should be counseled about the need for periodic gynecologic surveillance, especially those who are post‑menopausal. The side‑effect profile, while generally manageable, does include vasomotor symptoms such as hot flashes, which affect roughly one‑third of users and can be mitigated with lifestyle adjustments. Additionally, some individuals report mood fluctuations and a subtle cognitive fog, underscoring the importance of a holistic supportive care plan. The risk of thromboembolic events, although low, warrants a careful assessment of personal and familial clotting histories before initiating therapy. Pharmacogenomics adds another layer of complexity: CYP2D6 polymorphisms can dramatically alter plasma concentrations, leading to either sub‑therapeutic exposure or heightened toxicity. Thus, genotyping may become a valuable tool in personalizing Tamoxifen dosing in the near future. From an adherence standpoint, the daily pill regimen can become a psychological burden, serving as a constant reminder of the disease; peer support groups have demonstrated efficacy in improving compliance. Clinicians should also be vigilant about drug‑drug interactions; common agents like certain antidepressants can inhibit CYP2D6 and blunt the drug’s effectiveness. The evolving landscape of endocrine therapy now includes aromatase inhibitors, which may be preferable in post‑menopausal women, yet Tamoxifen remains an indispensable option for younger patients with intact ovarian function. In summary, the benefits of Tamoxifen are profound, but they must be weighed against individual risk factors, side‑effect tolerance, and patient preferences. Ongoing research continues to refine its use, aiming to maximize survival while minimizing adverse outcomes.
Rory Martin
July 21, 2025 AT 17:02 PMIt’s suspicious how often the pharma giants push Tamoxifen without fully disclosing the hidden long‑term vascular risks. Some say the data is selectively published, keeping the clotting danger under wraps. Stay vigilant and demand full transparency from your oncologist.
Maddie Wagner
July 25, 2025 AT 18:18 PMHey everyone, I’ve walked the Tamoxifen road with my sister and I can tell you the journey is a roller‑coaster of emotions. The hot flashes feel like spontaneous fireworks, but knowing they’re a sign the drug is doing its job gives me a weird sense of pride. I learned that setting a daily alarm and pairing the pill with a glass of water turned it into a ritual that kept me on track. If you’re struggling, reach out to a support group; sharing stories usually lightens the emotional load. Remember, you’re not alone in this battle.
Boston Farm to School
July 29, 2025 AT 19:33 PMGot the info about bone benefits they’re nice but also watch the uterus risk some doctors forget the endometrial checks it can be easy to miss
Emily Collier
August 2, 2025 AT 20:49 PMIt's encouraging to see the data presented so clearly; the reduction in recurrence rates truly highlights Tamoxifen's efficacy. Patients should be reminded that regular follow‑ups, including mammograms and gynecologic exams, are essential to catch any rare complications early. Lifestyle modifications, such as maintaining a healthy weight and staying active, can further enhance the drug's protective effects. Open communication with the healthcare team about any side effects will enable timely interventions and improve adherence.
Catherine Zeigler
August 6, 2025 AT 22:05 PMReading through the comprehensive overview reminds me of how far breast cancer treatment has come, yet also how much we still rely on patient perseverance. The fact that Tamoxifen can simultaneously protect bone density while battling cancer cells is a fascinating duality that underscores the elegance of selective estrogen receptor modulators. However, the journey isn’t without its hurdles; navigating hot flashes, mood swings, and occasional joint discomfort can feel overwhelming without proper support. I’ve found that integrating gentle yoga and mindfulness meditation into my routine helps to temper those vasomotor symptoms and improves overall well‑being. Moreover, staying connected with a community of fellow survivors offers a shared space to exchange coping strategies, making the daily pill feel less like a burden and more like a collective commitment to health. It’s also worth noting that genetic testing for CYP2D6 variants can provide insight into how effectively one’s body metabolizes the medication, potentially guiding dosage adjustments. While the drug’s impact on reducing recurrence is well documented, we must also remain vigilant about monitoring for rare but serious side effects such as thromboembolic events. Regular check‑ups with both oncologists and primary care physicians ensure that any emerging concerns are caught early. Ultimately, the decision to embark on a five‑ to ten‑year course of Tamoxifen should be a collaborative one, balancing the statistical benefits with personal quality‑of‑life considerations. By staying informed, proactive, and supported, patients can navigate this treatment journey with confidence and optimism.
henry leathem
August 10, 2025 AT 23:21 PMFrom a clinical pharmacology standpoint, the risk‑benefit calculus of tamoxifen unequivocally favors its inclusion in adjuvant protocols for ER‑positive malignancies, notwithstanding its endothelial perturbations and the marginal uptick in endometrial neoplasia incidence. Nevertheless, the oncologic community must perpetually recalibrate dosing schemas to mitigate thrombotic propensity, especially in hypercoagulable phenotypes. Evidence‑based stratification remains the linchpin of optimal therapeutic index.
jeff lamore
August 15, 2025 AT 00:37 AMThank you for the detailed synthesis; the data points are clear and actionable. It’s helpful to have both the statistical outcomes and practical management tips in one place. Looking forward to more updates on emerging endocrine therapies. Keep up the good work!
Kris cree9
August 19, 2025 AT 01:52 AMi read the whole thing its cool but man tamoxifen got me scared i dont know what to do lol
Paula Hines
August 23, 2025 AT 03:08 AMLife is a series of choices and tamoxifen is one of those paradoxes a drug that fights while it can also harm it mirrors the duality of existence we must accept the risk to gain the peace the journey is yours
John Babko
August 27, 2025 AT 04:24 AMIndeed, the therapeutic value of tamoxifen is undeniable!!! However, clinicians must remain vigilant; the possibility of endometrial hyperplasia, though low, demands regular monitoring!!! Patient education is paramount!!!
Stacy McAlpine
August 31, 2025 AT 05:40 AMTamoxifen helps a lot but you gotta stick to the schedule. Missing doses can lower the protection so set a reminder and take it every day.
Roger Perez
September 4, 2025 AT 06:55 AMGreat rundown! 👍 I’ve been on tamoxifen for three years and the hot flashes can be wild 🌡️ but staying active and drinking cold water helps. Keep sharing the science! 🚀
michael santoso
September 8, 2025 AT 08:11 AMThe presented data, while comprehensive, fails to address the nuanced interplay between CYP2D6 polymorphisms and systemic exposure, thereby overlooking a critical determinant of therapeutic efficacy.
M2lifestyle Prem nagar
September 12, 2025 AT 09:27 AMStay strong keep moving and trust your doctor
Karen Ballard
September 16, 2025 AT 10:43 AMThanks for the clear and helpful information.
Gina Lola
September 20, 2025 AT 11:59 AMYo, that tamoxifen stuff is wild – it’s like a double‑edged sword in the hormone game. Gotta keep an eye on the clot risks but the recurrence cut is solid.