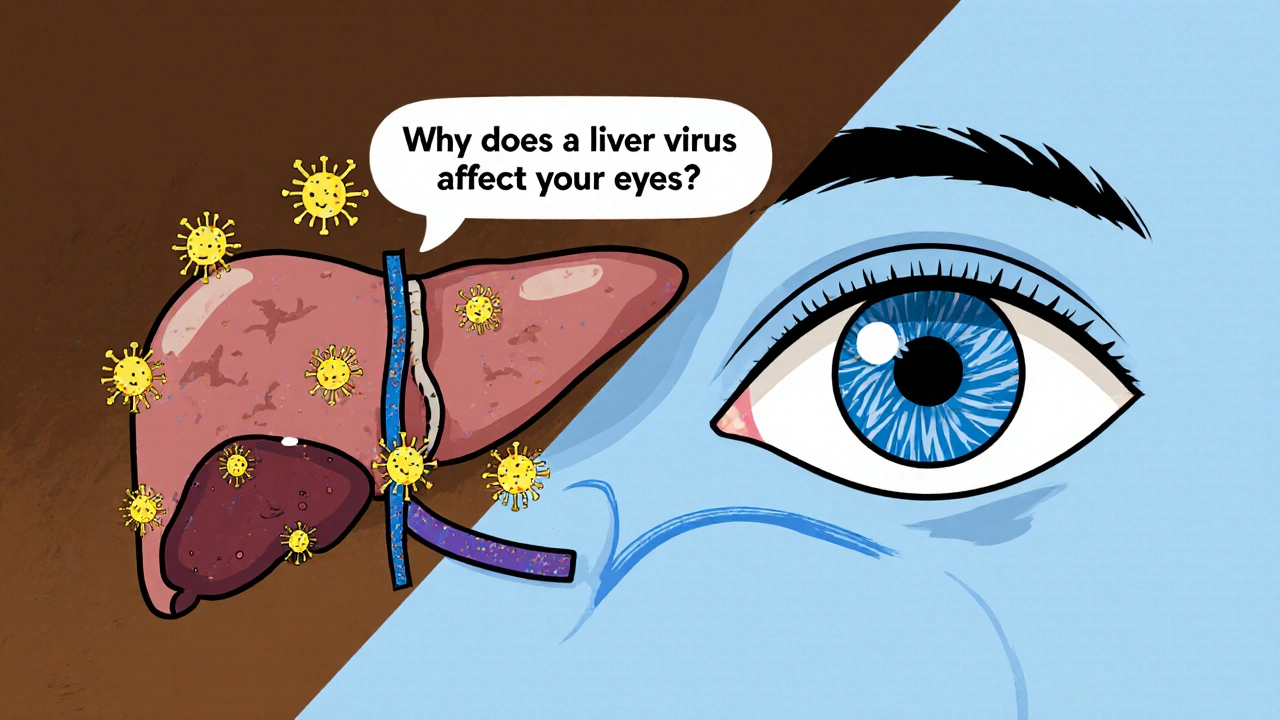
When dealing with chronic hepatitis C eye, the eye‑related problems that arise from long‑standing hepatitis C infection. Also called HCV ocular disease, it covers a range of conditions from mild dryness to serious retinal vasculitis.
Understanding the link starts with Hepatitis C virus, a blood‑borne virus that primarily attacks the liver but can also trigger immune‑mediated damage elsewhere. When the virus persists, immune complexes often form, leading to cryoglobulinemia, a condition where abnormal proteins clump in cooler parts of the body, including the eyes. These clumps can block tiny retinal vessels, causing retinal vasculitis or optic neuropathy. Another related entity is ocular manifestations, the range of eye symptoms like sicca syndrome, uveitis, and corneal lesions linked to chronic HCV. Together, they illustrate how chronic hepatitis C elevates risk for vision‑threatening issues.
First, the most common eye sign is **dry eye syndrome**, caused by reduced tear production and inflammation. Second, patients may notice retinal microvascular changes, often spotted during routine eye exams as cotton‑wool spots or hemorrhages. Third, less frequent but serious complications include *optic neuritis* and *macular edema*, both of which can impair central vision. The presence of cryoglobulinemia amplifies these risks by depositing immune complexes in the retinal circulation, a relationship captured by the semantic triple: "cryoglobulinemia influences chronic hepatitis C eye complications."
Management hinges on two fronts. Antiviral therapy—especially direct‑acting antivirals (DAAs)—targets the root cause by eradicating HCV, which in turn reduces immune complex formation. Clinical trials have shown that successful viral clearance lowers the incidence of new eye lesions and can even improve existing retinal findings, fulfilling the triple: "chronic hepatitis C eye requires antiviral therapy for improvement." For symptomatic relief, ophthalmologists often prescribe lubricating eye drops for dryness and corticosteroid eye drops for inflammatory uveitis, while systemic immunosuppressants may be considered for severe cryoglobulinemic vasculitis.
Screening is essential. Anyone with chronic hepatitis C should have a baseline ophthalmic exam, even if they feel fine. Regular follow‑up every 6–12 months helps catch early changes before they threaten sight. Patients with known cryoglobulinemia need even closer monitoring because the immune complexes can flare unpredictably.
All these points set the stage for the articles you’ll find below. We’ve gathered guides on specific treatments, case studies of retinal vasculitis, tips for managing dry eye in HCV patients, and the latest updates on DAAs and their eye‑related outcomes. Dive in to see practical advice, detailed drug comparisons, and real‑world experiences that will help you navigate chronic hepatitis C eye issues with confidence.
Explore how genotype 3 chronic hepatitis C can affect eye health, the symptoms to watch for, screening steps, and treatment options to safeguard vision.
read more