Non-Opioid Pain Management Finder
Find Your Best Non-Opioid Pain Relief
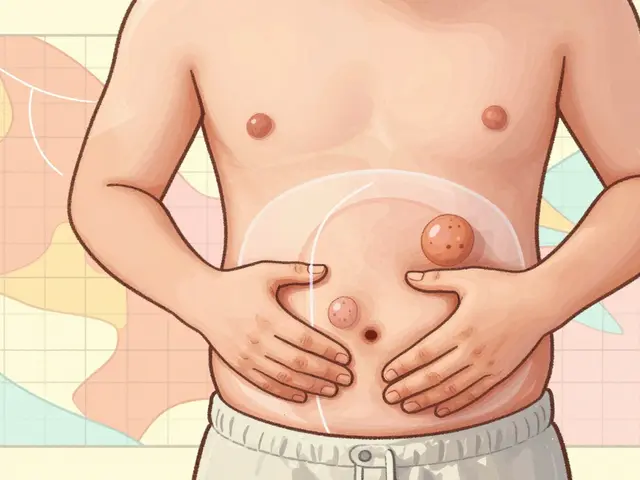
Recommended Options
Physical Therapy
Effectiveness: 85%
Side Effects: None
Insurance Coverage: Varies
Cognitive Behavioral Therapy
Effectiveness: 75%
Side Effects: None
Insurance Coverage: Often Covered
Topical Treatments
Effectiveness: 70%
Side Effects: Minimal
Insurance Coverage: Limited
NSAIDs
Effectiveness: 65%
Side Effects: Stomach, kidney, heart
Insurance Coverage: Often Covered
Acetaminophen
Effectiveness: 60%
Side Effects: Liver
Insurance Coverage: Often Covered
Suzetrigine
Effectiveness: 80%
Side Effects: Minimal
Insurance Coverage: Limited
For millions of people living with chronic pain, opioids are no longer the go-to solution. The risks - addiction, overdose, tolerance - are too high, and the science now clearly shows they don’t work well over the long term. In 2021 alone, over 16,700 deaths in the U.S. were linked to prescription opioids, according to the CDC. That’s why doctors are shifting hard toward non-opioid pain management. The good news? There are dozens of effective, safer options that actually help people move better, sleep deeper, and live fuller lives - without the danger of dependence.
What Non-Opioid Pain Management Really Means
Non-opioid pain management isn’t just about swapping one pill for another. It’s a full toolkit: physical movement, mental strategies, targeted medications, and hands-on therapies. The CDC’s 2022 guidelines say it plainly: for chronic pain, non-opioid treatments should come first. Opioids? Only if everything else has been tried and the benefits clearly outweigh the risks. This shift isn’t theoretical. A 2022 study in JAMA Network Open tracked over 200 people with chronic back or joint pain for a year. Those on non-opioid treatments reported the same level of pain relief as opioid users - but with nearly 40% fewer side effects. No foggy brain. No constipation. No risk of overdose. Just real, lasting improvement.Top Non-Pharmacological Approaches That Deliver Results
Medications aren’t the only answer. In fact, for many people, movement and mindset are the most powerful tools.- Exercise therapy: Whether it’s walking, swimming, or strength training, regular physical activity reduces inflammation and rebuilds muscle that supports painful joints. The CDC recommends at least 2-3 sessions per week for 6-8 weeks to see real change. People with knee osteoarthritis who did water-based exercises saw 40% less pain after 12 weeks.
- Cognitive Behavioral Therapy (CBT): This isn’t just "thinking positive." CBT teaches you how pain changes your brain and how to rewire those patterns. Eight to 12 weekly sessions can cut pain intensity by 30-50% in people with fibromyalgia or chronic back pain.
- Acupuncture and massage: A survey of 247 chronic pain patients on Mayo Clinic Connect found 68% got moderate to significant relief from physical therapy, and 52% found acupuncture helpful. These aren’t fringe treatments - Medicare and many private insurers now cover them.
- Mindfulness and yoga: Daily practice of 20-45 minutes for 6-8 weeks can reduce pain-related stress signals in the brain. Studies show people who stick with mindfulness report better sleep and less reliance on meds.
Effective Non-Opioid Medications You Can Actually Use
When meds are needed, there are plenty of options that don’t carry the same dangers as opioids.- NSAIDs (ibuprofen, naproxen): Great for inflammation-based pain like arthritis or tendonitis. But don’t take them long-term - they can hurt your stomach, kidneys, or heart. Stick to the lowest dose for the shortest time.
- Acetaminophen (Tylenol): Safer on the stomach than NSAIDs, but too much can damage your liver. The max daily dose is 3,000-4,000 mg, depending on your health. That’s about 6 extra-strength tablets. Don’t go over.
- Duloxetine (Cymbalta) and venlafaxine (Effexor): These SNRI antidepressants are FDA-approved for nerve pain and chronic musculoskeletal pain. About 30-40% of users get 30-50% pain reduction. Side effects? Nausea and drowsiness at first, but most people adjust.
- Pregabalin (Lyrica) and gabapentin: First-line for nerve pain from diabetes, shingles, or sciatica. About half of users see noticeable relief. But drowsiness and weight gain are common - up to 62% report feeling foggy.
- Topical treatments: Capsaicin cream (from chili peppers) and lidocaine patches deliver pain relief right where it hurts, with almost no systemic side effects. Great for localized joint or nerve pain.

The Big New Player: Suzetrigine (Journavx)
In October 2023, the FDA approved something groundbreaking: suzetrigine, the first new non-opioid painkiller in over 20 years. It’s not for everyday aches. It’s for moderate to severe acute pain - like after surgery or a broken bone - where NSAIDs and acetaminophen aren’t enough. Unlike opioids, suzetrigine doesn’t affect the brain’s reward system. It blocks sodium channels in nerves, stopping pain signals before they reach the brain. Early data shows it’s as effective as low-dose opioids - without the risk of addiction. This is a turning point. It proves that safe, powerful non-opioid pain relief is possible, even for intense pain.Why Some People Still Struggle - And How to Get Help
The problem isn’t that these options don’t work. It’s that they’re hard to access. Insurance often limits physical therapy to 15-20 visits a year. Acupuncture needs pre-approval. CBT can cost $100-$150 per session without coverage. A 2022 U.S. Pain Foundation survey found 42% of patients hit insurance walls when trying non-opioid care. Rural areas are worse off. A 2023 study found 58% of rural counties have no physical therapist, and 72% have no psychologist. If you live in one of these places, telehealth is your best bet. Many CBT programs and yoga classes are now available online through Medicare or private insurers. If you’re stuck, talk to your doctor about these resources:- The U.S. Pain Foundation offers free toolkits and connects patients with local support.
- The American Chronic Pain Association provides downloadable guides on exercise, CBT, and self-management.
- Ask if your clinic has a pain specialist on staff. Multimodal plans - combining physical therapy, meds, and mental health support - work best.
What Doesn’t Work - And What to Avoid
Not all "alternatives" are equal. Skip these:- Long-term high-dose NSAIDs: They don’t fix the problem - they just mask it, while damaging your organs.
- Unregulated supplements: CBD oil, turmeric pills, and other supplements aren’t FDA-tested for pain. Some may interact with your meds.
- Waiting too long to act: The longer you wait to try non-opioid options, the more your nervous system gets wired for pain. Early intervention = better outcomes.
Real Stories, Real Results
On Reddit’s r/ChronicPain community, one user shared how they cut their pain in half after 6 months of aquatic therapy, CBT, and low-dose naltrexone (an off-label use that reduces inflammation). Another swapped daily oxycodone for daily walking and a topical capsaicin cream - and hasn’t had a panic attack about pain since. These aren’t outliers. They’re examples of what’s possible when you stop treating pain with a single pill and start treating it as a whole-body issue.Getting Started: Your 30-Day Plan
If you’re ready to move away from opioids, here’s how to begin:- Week 1-2: Talk to your doctor. Ask: "What non-opioid options are right for my type of pain?" Request referrals for physical therapy or CBT.
- Week 3-4: Start one movement activity - even 10 minutes of walking or stretching daily. Add one non-opioid med if prescribed (like acetaminophen or a topical cream).
- Week 5-6: Try one mind-body practice. Use a free app like Insight Timer for 10 minutes of mindfulness each morning.
The Future Is Here
The non-opioid pain market is growing fast - from $35.7 billion in 2022 to an expected $58.3 billion by 2030. Why? Because people are demanding safer care. Researchers are developing new drugs, wearable pain devices, and even biomarker tests to match the right treatment to the right person. You don’t have to wait for the future. The tools are here now. They’re not perfect. They take effort. But they’re safer, more sustainable, and often more effective than opioids ever were. It’s not about giving up pain relief. It’s about getting better relief - without the risk.Are non-opioid pain treatments really as effective as opioids?
Yes - for most chronic pain conditions. A 2022 study in JAMA Network Open found that people using non-opioid treatments for back or joint pain had the same level of pain relief after 12 months as those on opioids - but with far fewer side effects. Opioids don’t work well long-term, and their risks often outweigh the benefits. Non-opioid options like physical therapy, CBT, and certain medications are now the first-line recommendation by the CDC and FDA.
What’s the safest non-opioid pain reliever for daily use?
For most people, acetaminophen (Tylenol) is the safest daily option - if you stay under 3,000-4,000 mg per day. But it doesn’t reduce inflammation. For inflammation-based pain like arthritis, short-term use of NSAIDs (ibuprofen, naproxen) is effective, but not ideal for long-term daily use due to kidney and stomach risks. Topical treatments like capsaicin or lidocaine patches are often the safest for ongoing use since they don’t enter your bloodstream much.
Can I use non-opioid treatments if I’m already on opioids?
Absolutely - and you should. Many people transition from opioids to non-opioid care with medical supervision. Your doctor can help you slowly reduce opioids while introducing physical therapy, CBT, or medications like duloxetine or pregabalin. This is called a multimodal approach, and it’s the most successful way to reduce opioid dependence without worsening pain.
Why isn’t my insurance covering physical therapy or acupuncture?
Many insurers still limit coverage due to outdated policies or cost concerns. Medicare covers 80% of physical therapy after your deductible, but private plans often cap visits at 15-20 per year. Acupuncture usually requires pre-authorization. Call your insurer and ask for a copy of their pain management policy. If denied, ask your doctor to write a letter of medical necessity - many denials are overturned with proper documentation.
Is there a new non-opioid drug I should ask my doctor about?
Yes - suzetrigine (brand name Journavx), approved by the FDA in October 2023. It’s the first new non-opioid painkiller in over 20 years and is designed for moderate to severe acute pain, like after surgery or injury. It works differently than opioids and has no addiction risk. It’s not for chronic pain yet, but it’s a major step forward. Ask your doctor if it’s appropriate for your situation.
What if I live in a rural area with no physical therapists or pain specialists?
Telehealth is your best option. Many CBT programs, yoga classes, and even physical therapy sessions are now available online. The U.S. Pain Foundation and American Chronic Pain Association offer free digital resources. Medicare and some private insurers cover virtual physical therapy. Start with daily walking, stretching, and mindfulness apps - they’re free and proven to help. You don’t need a specialist to begin making progress.





Trevor Whipple
January 14, 2026 AT 05:04 AMman i tried all that cbt and yoga crap for my lower back and it did jack. then i got prescribed gabapentin and boom, i can actually sleep. why do people act like movement is some magic cure? my pain is neurological, not lazy.
Gregory Parschauer
January 15, 2026 AT 19:06 PMLet me be clear: the opioid crisis was not caused by pharmaceutical companies-it was caused by weak-willed patients who refused to endure discomfort like real humans. You don’t need ‘mindfulness’ or ‘aquatic therapy.’ You need discipline. Pain is a signal, not a sentence. If you can’t tolerate 10 minutes of walking without reaching for a pill, you’ve already lost the battle against your own biology. The CDC’s guidelines are a surrender to weakness, not a medical breakthrough.
And don’t get me started on suzetrigine. Another pharmaceutical placebo dressed up as innovation. If it worked so well, why wasn’t it developed 20 years ago? Because the profit margins on opioids are still better. This is just rebranding.
Acupuncture? Please. It’s placebo with needles. The only reason Medicare covers it is because bureaucrats are too lazy to say no. If you want real relief, stop chasing trends and start building resilience. Pain is part of life. Learn to carry it.
Milla Masliy
January 17, 2026 AT 06:47 AMI’m a physical therapist in rural Kansas, and I can tell you-this post nails it. We’ve seen people go from wheelchair-bound to walking without meds using just water therapy and CBT. But you’re right, access is the real issue. My clinic has a waiting list of 8 weeks, and half my patients can’t afford copays. Telehealth helped during the pandemic, but now it’s back to ‘we’ll cover 5 visits.’
One woman I worked with switched from oxycodone to daily stretching and a lidocaine patch. She said, ‘I don’t feel numb anymore-I feel alive.’ That’s the goal, not just less pain, but more life.
If you’re reading this and stuck, DM me. I’ll send you free home exercise videos. You don’t need a specialist to start moving.
Damario Brown
January 17, 2026 AT 09:08 AMlol the whole ‘non-opioid’ thing is just a cover for insurance companies not wanting to pay for real painkillers. gabapentin makes you fat and drowsy, cymbalta gives you brain fog, and tylenol gives you liver failure if you breathe wrong. meanwhile, opioids? yeah, they’re risky, but they WORK. you think people take them because they like being addicted? no, they take them because nothing else touches their pain.
and suzetrigine? sounds like a drug company’s marketing department got drunk and named it. ‘Journavx’? what is this, a sci-fi movie? next they’ll patent ‘PainGone 3000’ and charge $2000 a pill.
stop pretending this is about safety. it’s about cost. and if you’re telling someone with degenerative disc disease to ‘do yoga’ instead of giving them relief, you’re not a healer-you’re a bureaucrat with a clipboard.
sam abas
January 18, 2026 AT 08:05 AMInteresting how the article cherry-picks studies. The JAMA study? Yeah, it showed equal pain relief-but only after 12 months. What about the first 3 months? Opioids were significantly better then. And the ‘40% fewer side effects’? That’s because they excluded patients who dropped out due to worsening pain. They didn’t report attrition rates. Classic bias.
Also, the ‘topical treatments’ section ignores that capsaicin burns like hell for the first two weeks. Most people quit. And CBT? It’s great if your pain is psychosomatic. But if your spine is collapsing? No amount of mindfulness will fix a herniated disc.
And why is suzetrigine only for acute pain? Because it doesn’t work for chronic. The FDA knows it. They’re just selling hope to people who’ve been failed by the system. Meanwhile, the real solution-better pain research funding-isn’t even mentioned.
Also, ‘talk to your doctor’? My doctor doesn’t know what CBT is. He just prescribes pills and hopes for the best. The system is broken, and this post is just pretty words for people too scared to admit it.
John Pope
January 20, 2026 AT 03:53 AMThere’s a deeper metaphysical layer here that no one’s addressing: pain isn’t just a biological event-it’s a narrative. We’ve been conditioned to see pain as an enemy to be eradicated, when in truth, it’s a teacher. The opioid crisis wasn’t about drugs-it was about our collective refusal to sit with discomfort, to let pain reveal what we’ve been avoiding.
CBT doesn’t just ‘rewire the brain’-it dissolves the ego’s illusion of control. When you practice mindfulness, you’re not reducing pain-you’re dissolving the resistance to it. That’s why people report feeling ‘more alive’-they’re not numbing themselves anymore.
And suzetrigine? It’s a technological band-aid on a spiritual wound. We’re building better painkillers while ignoring the cultural sickness that made us need them in the first place. We’ve outsourced our suffering to pills because we’ve lost the rituals, the community, the sacred space to feel without fixing.
Maybe the real non-opioid solution isn’t a drug or a therapy-it’s relearning how to be human in a world that treats pain like a bug to be patched.
Clay .Haeber
January 21, 2026 AT 17:45 PMOh wow, another feel-good, Pinterest-approved pain manifesto. Let me guess-next you’ll tell me that crying into a journal while drinking turmeric lattes will fix my herniated disc? Congrats, you’ve turned chronic pain into a wellness influencer’s dream.
Acupuncture? It’s just placebo with a side of incense. And ‘water-based exercises’? Yeah, because nothing says ‘cure’ like floating like a jellyfish while your spine crumbles.
And suzetrigine? The FDA approved a drug named after a rejected character from Star Trek? Journavx? That’s not a medication-that’s a rejected brand name for a new energy drink. You think this is progress? It’s just corporate rebranding with a side of virtue signaling.
Meanwhile, people with real pain are still getting denied care because their insurance thinks ‘stretching’ is a valid substitute for morphine. This isn’t science. It’s a sales pitch dressed in TED Talk pajamas.
Avneet Singh
January 22, 2026 AT 00:51 AMLet’s be honest-this entire article is a marketing brochure for Big Pharma’s new non-opioid revenue stream. Suzetrigine? It’s just another molecule waiting to be patented. The real winners here aren’t patients-they’re the shareholders of the companies that now control the ‘safe pain’ market.
And don’t get me started on ‘CBT for chronic pain.’ That’s code for ‘we don’t have a real solution, so we’ll make you feel guilty for wanting one.’
Meanwhile, in India, people with severe arthritis use traditional Ayurvedic oils and daily movement. No insurance. No apps. No CBT. Just community, consistency, and centuries of empirical knowledge. Maybe the answer isn’t more drugs or more therapy-it’s less Western medical arrogance.