Acromegaly Symptom Checker
Symptom Assessment Tool
This tool is for educational purposes only and does not provide a diagnosis. If you're experiencing multiple symptoms, consult a healthcare professional.
When doctors talk about Acromegaly is a rare hormonal disorder caused by excess growth hormone, usually due to a pituitary adenoma, they’re describing a condition that slowly reshapes the face, hands, and internal organs.
What Triggers the Hormone Overload?
The root cause is almost always a benign tumor in the pituitary gland called a Pituitary adenoma a noncancerous growth that secretes too much growth hormone (GH). This hormone pushes the liver to produce Insulin-like growth factor 1 (IGF-1) the main mediator of growth hormone’s effects on tissues. When GH and IGF‑1 stay high for years, cartilage, bone, and soft tissue keep expanding.
Key Signs That Something's Wrong
Because the changes happen gradually, patients often dismiss early clues. Here are the most common acromegaly symptoms to watch for:
- Enlarged hands and feet - ring sizes increase, shoe sizes jump.
- Coarse facial features - prominent jaw (prognathism), thicker lips, and a wider nose.
- Skin changes - oily, sweaty, and thickened skin that may develop deep folds.
- Joint pain and stiffness - especially in the knees and hips.
- Headaches or visual field loss - pressure from the adenoma on the optic chiasm.
- Excessive sweating and fatigue.
If any of these pop up, especially together, it’s worth asking a doctor for a hormonal work‑up.
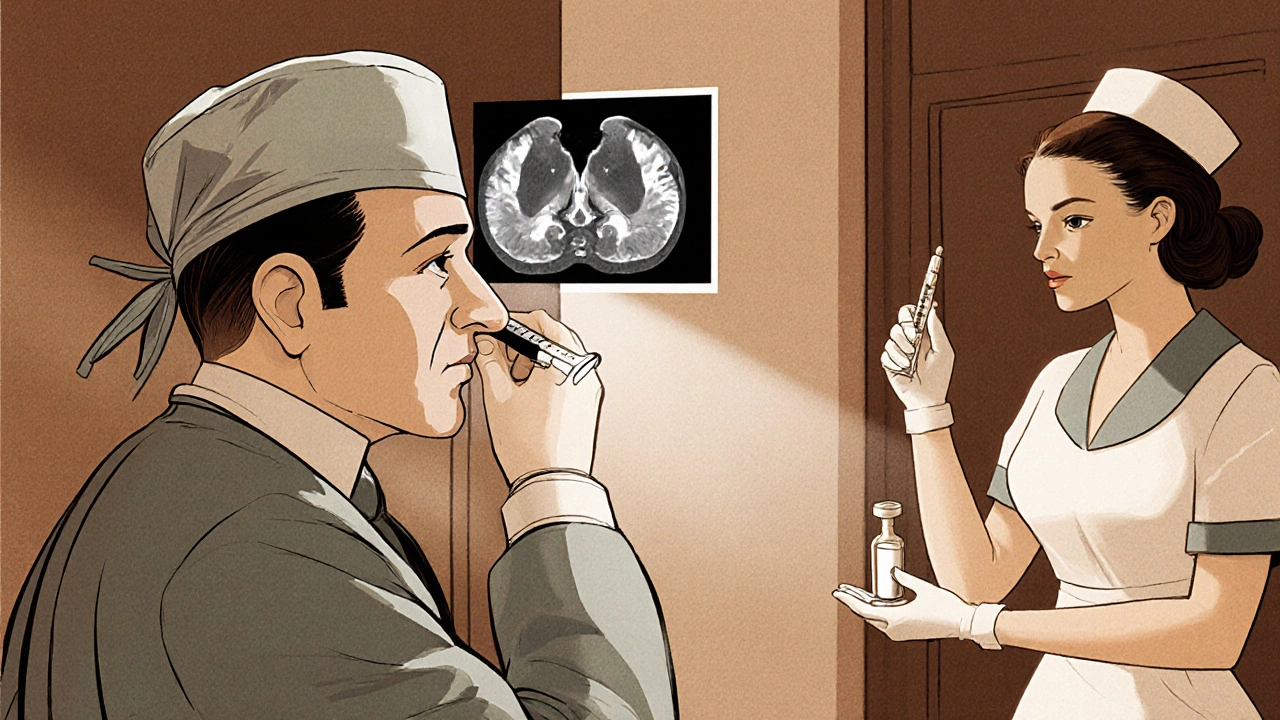
How Doctors Confirm the Diagnosis
Diagnosing acromegaly is a two‑step process: biochemical testing followed by imaging.
- Blood test for Growth hormone measured in nanograms per milliliter (ng/mL). A random GH level >1ng/mL is suspicious.
- Oral glucose tolerance test (OGTT). In healthy people, a glucose load suppresses GH below 0.4ng/mL. Failure to suppress confirms hypersecretion.
- Serum IGF-1 age‑ and sex‑adjusted levels is measured; elevated IGF‑1 supports the diagnosis.
- Magnetic resonance imaging (MRI) of the brain. A high‑resolution MRI scan that visualises the pituitary region pinpoints the size and invasiveness of the adenoma.
Endocrinologists often coordinate these tests. When you see a specialist, you’ll likely meet Endocrinologist a physician focused on hormone disorders, who will interpret the results and design a treatment plan.
Treatment Options: What Works Best?
Management aims to normalize GH/IGF‑1, shrink the tumor, and relieve symptoms. The three main pillars are surgery, medication, and radiotherapy.
| Treatment | How It Works | Typical Success Rate | Key Considerations |
|---|---|---|---|
| Transsphenoidal surgery | Direct removal of pituitary adenoma via nasal passage | 70‑80% achieve remission (GH<1ng/mL) | Best for small, well‑circumscribed tumors; requires experienced neurosurgeon |
| Somatostatin analogs (e.g., octreotide, lanreotide) | Mimic somatostatin, suppress GH release | 40‑60% normalize IGF‑1 when used alone | Injectable; may cause GI upset, gallstones |
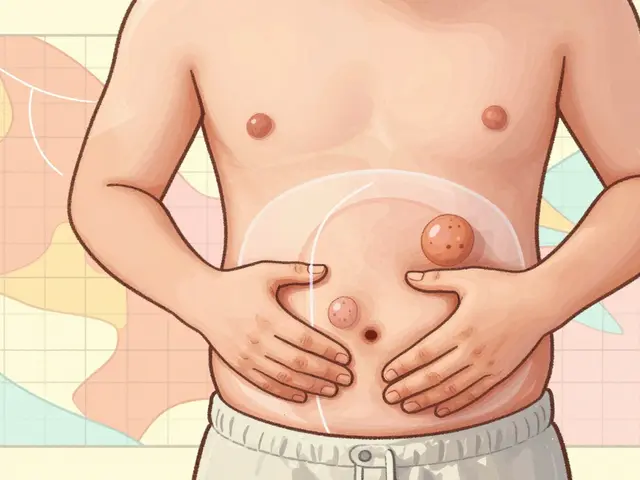
| Pegvisomant | GH receptor blocker, blocks peripheral effects of GH | 80‑90% normalize IGF‑1 | Daily oral injection; liver‑function monitoring needed |
| Radiotherapy (fractionated or stereotactic) | Targets residual tumor cells with focused radiation | 30‑50% achieve hormonal control over 5‑10years | Delayed effect; risk of hypopituitarism |
When the adenoma is small and accessible, Transsphenoidal surgery the preferred first‑line approach for most patients often offers the quickest remission. However, many patients need adjunct medication to keep GH/IGF‑1 in check.
Two medication families dominate:
- Somatostatin analogs drugs that inhibit growth hormone secretion-given as long‑acting injections every 4‑8 weeks.
- Pegvisomant a GH receptor antagonist that blocks the hormone’s action-administered daily subcutaneously.
In some cases, doctors combine a somatostatin analog with pegvisomant to achieve faster control.
Living With Acromegaly: Practical Tips
Even after treatment, patients benefit from lifestyle tweaks:
- Regular endocrinology follow‑ups to keep IGF‑1 in range.
- Dental check‑ups-enlarged jaw can affect bite and oral health.
- Joint‑friendly exercise (swimming, cycling) to ease arthritis.
- Weight management-excess GH can cause insulin resistance.
- Sleep‑study if you notice breathing pauses; enlarged tissues can narrow the airway.
Support groups, both online and in‑person, provide emotional backup and practical advice on coping with cosmetic changes.
Common Pitfalls & How to Avoid Them
Missteps often stem from delayed diagnosis. Here are three red flags you should never ignore:
- Assuming “just aging” when hands feel bigger. Measure ring size annually.
- Skipping the OGTT after a single high GH reading. The suppression test is decisive.
- Choosing medication without a baseline MRI. Tumor size guides whether surgery first could spare you lifelong drugs.
Open communication with your Endocrinologist who coordinates testing and treatment ensures you stay on the right track.
Future Directions: What’s on the Horizon?
Research is exploring newer agents that target the GH receptor more precisely, as well as gene‑editing approaches that could shrink adenomas without surgery. Clinical trials of long‑acting pegvisomant formulations promise fewer injections per year.
For now, early detection and a personalized treatment mix remain the best defense against the long‑term complications of acromegaly, such as cardiovascular disease, sleep apnea, and colon polyps.
Frequently Asked Questions
What age does acromegaly usually appear?
Most cases are diagnosed in adults between 30 and 50 years old, because the tumor grows slowly and symptoms take years to become noticeable.
Can acromegaly be cured?
Complete cure-defined as normal GH/IGF‑1 without medication-is achievable in up to 80% of patients who undergo successful transsphenoidal surgery, especially when the tumor is small.
Is there a genetic link?
Rare familial cases are tied to MEN1 (multiple endocrine neoplasia type1) syndrome, where pituitary adenomas are part of a broader tumor predisposition.
How often should IGF‑1 be checked after treatment?
Initially every 3-6 months, then annually once levels are stable and the tumor shows no growth on MRI.
Do lifestyle changes affect disease progression?
While lifestyle can’t reverse excess GH, maintaining a healthy weight, exercising, and managing blood sugar can reduce secondary complications like heart disease and diabetes.




Nickolas Mark Ewald
October 16, 2025 AT 19:31 PMIf your rings start feeling tight or your shoes no longer fit, that's a classic early red flag for acromegaly that many patients miss until the changes are obvious.
Tom Green
October 17, 2025 AT 07:46 AMWhen you see those hand and facial changes, the next step is to get an endocrinology consult; they’ll run the GH suppression test and order an MRI so you can pinpoint the adenoma before it presses on the optic chiasm.
Emily Rankin
October 17, 2025 AT 23:03 PMThe journey of a patient discovering that their jaw has subtly grown over years feels like a slow revelation of an unseen force shaping their very identity. Each morning they glance at the mirror, noticing a deeper line around the mouth, a broader nose that seems to have arrived without invitation. The gradual swelling of the soft tissue whispers that hormones are at work beyond the normal limits. In the world of endocrinology, this is the silent chorus of excess growth hormone and its messenger, IGF‑1, orchestrating a relentless expansion of bone and cartilage. The body, ever adaptable, begins to compensate: shoes become larger, rings no longer slide on, and the hands may feel like they belong to someone else. Pain joins the narrative as joints protest the added size, especially the knees and hips that bear the extra load. Yet the most profound shift is psychological – the self‑image reforms in tandem with the physical changes, prompting a mix of frustration and awe. It is essential to recognize that early biochemical testing, such as the oral glucose tolerance suppression test, can catch the disorder before the tumor presses on vision‑critical structures. An MRI then provides the map, revealing whether the adenoma is nestled safely within the sella or invading surrounding tissue. Surgical removal via the transsphenoidal route offers the best chance at remission, yet the decision must balance tumor size, surgeon expertise, and patient health. For those where surgery falls short, medical therapy with somatostatin analogues or GH receptor antagonists steps in to tame the hormone surge. Radiotherapy, though less commonly first‑line, remains a valuable tool for residual disease. Throughout this therapeutic odyssey, regular monitoring of IGF‑1 levels ensures the treatment stays on target, preventing the silent creep of complications like cardiomyopathy or sleep apnea. Moreover, patients find strength in support groups where shared stories illuminate coping strategies and reduce isolation. Ultimately, understanding that acromegaly is a manageable condition, not a fate sealed by a mysterious tumor, empowers individuals to reclaim agency over their health and future.
Rebecca Mitchell
October 18, 2025 AT 17:06 PMthe changes can be subtle at first many people just think they are getting older however the growth of the hands and feet often goes unnoticed until a new ring won t fit the old finger size and shoes feel tighter than usual
Roberta Makaravage
October 19, 2025 AT 07:00 AMObviously the hallmark signs you described are textbook examples of hypersecretion, so if you’re still unsure just remember that GH never obeys the usual feedback loops 😊 – the OGTT will stay stubbornly high and the MRI will reveal the culprit adenoma, essentially confirming what any seasoned endocrinologist has known for decades 🤓.
Sara Werb
October 19, 2025 AT 20:53 PMDo you realize that the pharmaceutical “cure” they push is a massive cover‑up!!! The real reason they keep you on pricey somatostatin analogues is to line their pockets while the “big pharma” elite watches the silent takeover of our endocrine system!!! They even seed the research papers with fake success rates!!!
Winston Bar
October 20, 2025 AT 10:46 AMAll that surgery hype is just marketing fluff.
Russell Abelido
October 21, 2025 AT 00:40 AMI hear you, but many patients actually feel relief once the hormone levels drop – it’s not all doom and gloom 🙂. Getting the right meds can make a real difference.
Steve Holmes
October 21, 2025 AT 14:33 PMWell, the data shows that transsphenoidal surgery has a remission rate of seventy to eighty percent, which contradicts the idea that it’s merely hype!!! Plus, the long‑term outcomes improve quality of life dramatically!!!
Lauren Sproule
October 22, 2025 AT 04:26 AMyeah i think the support groups really help people cope with the changes and keep them from feeling alone its awesome how folks share tips for coping with joint pain and the eye issues