Most people know to tell their doctor about their prescriptions. But how many of them mention the turmeric pill they take every morning, the calcium supplement from the health food store, or the grapefruit they eat with breakfast? If you’re taking any kind of medication - whether it’s for high blood pressure, diabetes, or depression - those seemingly harmless supplements and foods could be quietly messing with your treatment. And your pharmacist is the one person who can spot the danger before it happens.
Why This Conversation Matters More Than You Think
Over half of American adults take dietary supplements. That’s more than 180 million people. And nearly one in four of those people are also on prescription meds. The problem? Most don’t tell their doctor or pharmacist about it. A 2025 study found that only 6.7% of pharmacists were even asked about supplement use during a routine visit. That’s not because patients are hiding anything - it’s because they don’t realize it matters.
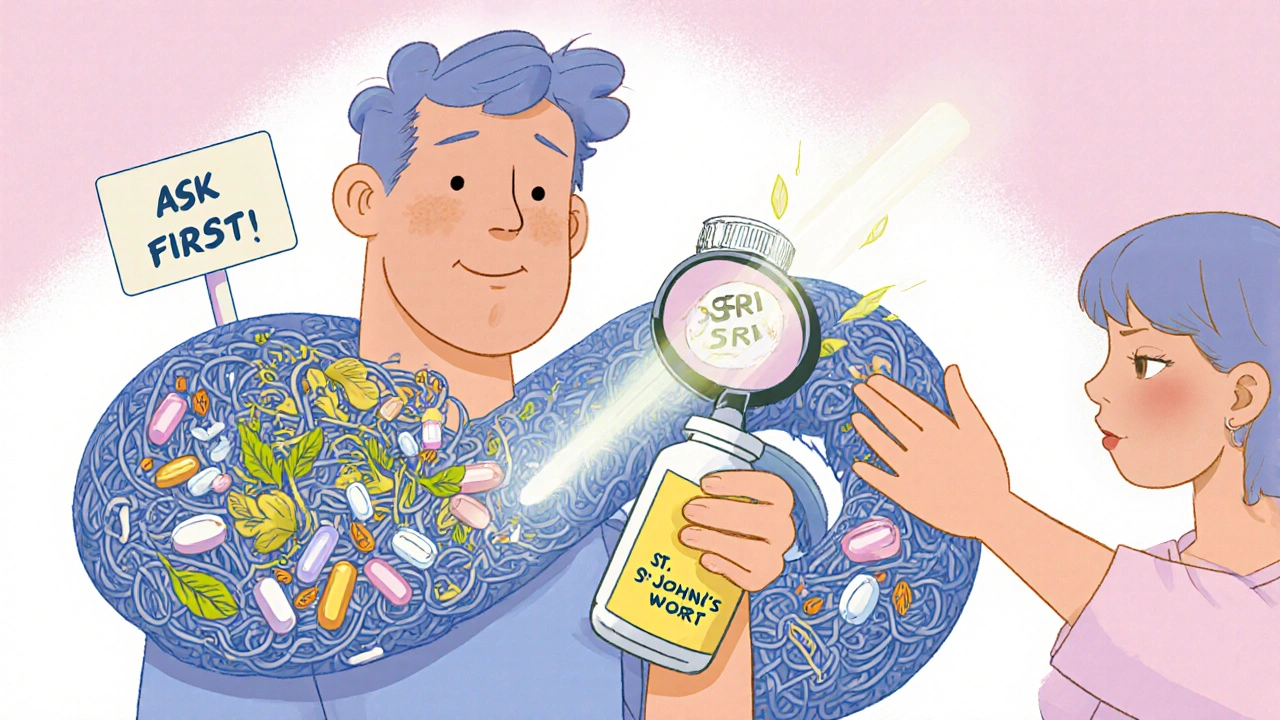
Here’s the reality: supplements aren’t regulated like drugs. The FDA doesn’t test them for safety or effectiveness before they hit store shelves. That means a bottle labeled "St. John’s wort" could contain anything from the real herb to a completely different plant, or even a hidden drug. And when you mix it with your antidepressant, it can trigger serotonin syndrome - a life-threatening condition.
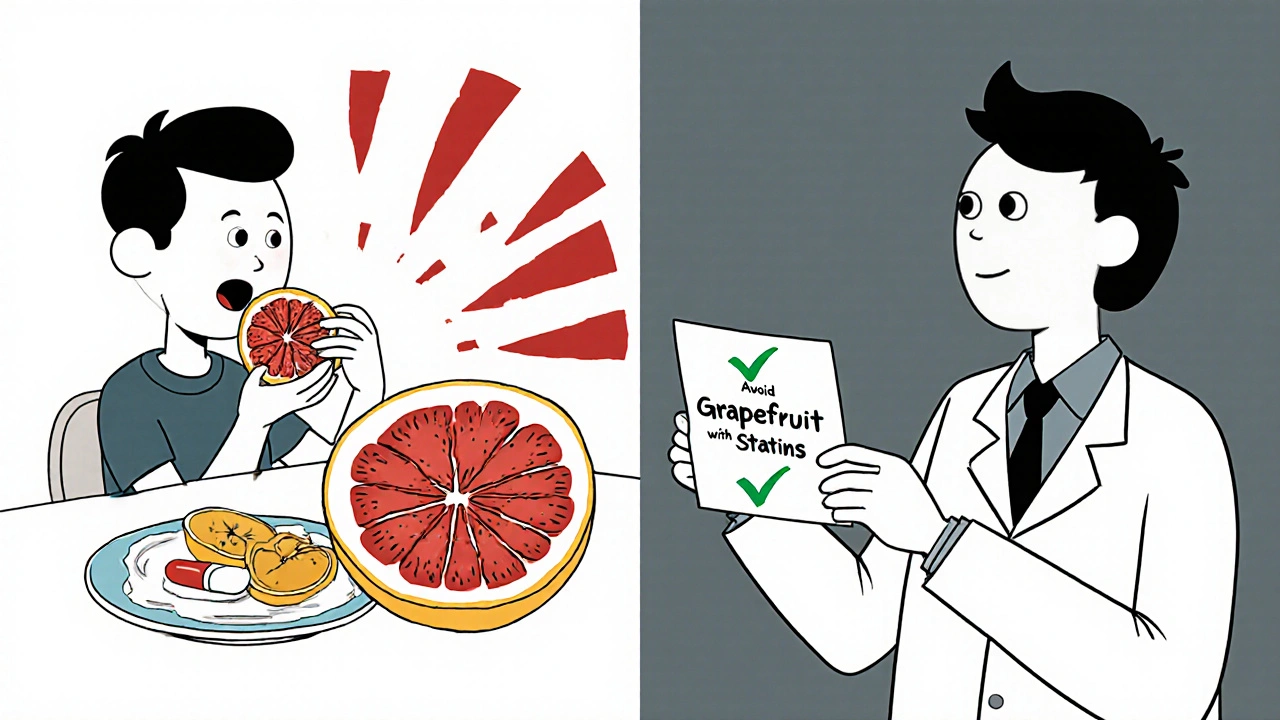
Food matters too. Grapefruit can make your cholesterol drug too strong. Dairy can block your antibiotic. Even a simple avocado could interfere with blood thinners. These aren’t myths. These are documented, dangerous interactions.
What You Need to Bring to Your Pharmacist
Don’t rely on memory. Walk in with a written list. Not just your prescriptions. Everything.
- Brand names and dosages of every supplement (vitamins, herbs, probiotics, fish oil, etc.)
- How often you take each one (morning, night, with food?)
- Any over-the-counter meds you use regularly (ibuprofen, antacids, sleep aids)
- Your daily diet habits - especially if you eat grapefruit, dairy, leafy greens, or alcohol regularly
Don’t say, "I take some vitamins." Say, "I take Nature Made B12 1000 mcg daily and Garden of Life Vitamin D3 5000 IU every morning with breakfast." Specifics save lives.
High-Risk Supplements You Must Mention
Not all supplements are equal. Some are ticking time bombs when mixed with common meds.
- St. John’s wort - interferes with antidepressants (SSRIs), birth control, blood thinners, and heart meds. Can cause serotonin syndrome.
- Goldenseal - blocks liver enzymes that break down dozens of drugs, including statins and blood pressure meds. Can lead to toxic buildup.
- Ginkgo biloba - increases bleeding risk, especially with warfarin, aspirin, or NSAIDs.
- Milk thistle - may alter how your body processes diabetes meds and statins.
- Calcium and iron supplements - bind to antibiotics like ciprofloxacin and tetracycline, making them useless if taken at the same time.
If you’re taking any of these, don’t wait for your pharmacist to ask. Bring them up first.
Food Interactions You Can’t Ignore
Food isn’t just fuel. It’s chemistry.
- Grapefruit and citrus - stops your body from breaking down statins, blood pressure meds, and some anti-anxiety drugs. One grapefruit can cause effects that last 72 hours.
- Dairy products - calcium in milk, yogurt, and cheese blocks absorption of antibiotics like doxycycline and ciprofloxacin. Take them 2-4 hours apart.
- Leafy greens (kale, spinach, broccoli) - high in vitamin K, which can reduce the effect of blood thinners like warfarin. Keep your intake consistent - don’t suddenly eat a salad every day if you didn’t before.
- Alcohol - makes sedatives, painkillers, and some antidepressants more dangerous. Can cause liver damage when mixed with acetaminophen.
- High-sodium foods - can counteract blood pressure meds and worsen fluid retention.
Your pharmacist doesn’t need your full meal plan. Just know what you eat daily and if it’s changed recently.
What Your Pharmacist Should Tell You
When you bring up supplements and food, you deserve more than a nod. You should get clear, actionable advice.
Ask these questions:
- "Is this supplement safe with my current meds?"
- "Should I take this at a different time than my pill?"
- "Is there a food I should avoid while taking this?"
- "Could this be causing the side effects I’ve been feeling?"
- "Is there a better, safer option?"
Pharmacists are trained to check for interactions using databases that link supplements to drug metabolism. By 2025, most major pharmacy chains like CVS and Walgreens have integrated these tools into their systems. But they can’t use them if you don’t tell them what you’re taking.
Medications That Drain Your Nutrients
Some drugs don’t just interact - they deplete your body of essential nutrients. And you might not even know it.
- Proton pump inhibitors (PPIs) - like omeprazole - lower vitamin B12, magnesium, and calcium. Long-term use can lead to nerve damage and bone loss.
- Metformin - for diabetes - reduces B12 and folate. Low levels can cause fatigue, brain fog, and tingling in hands and feet.
- Statins - lower coenzyme Q10. That’s linked to muscle pain and weakness - a common complaint among users.
- Diuretics - drain potassium and magnesium. Can cause cramps, irregular heartbeat, and dizziness.
- Birth control pills - reduce B vitamins and magnesium. May contribute to mood swings and headaches.
If you’ve been on any of these meds for over a year, ask your pharmacist: "Could this be making me deficient in something? Should I be taking a supplement to balance it?"
What to Do If Your Pharmacist Doesn’t Ask
Don’t wait. If your pharmacist doesn’t bring up supplements, you’re the one who has to.
Pharmacists are busy. But they’re also trained for this. A 2025 study showed that when pharmacists were trained to ask specific questions - like "Do you take St. John’s wort or ginkgo?" - they caught 4 times as many dangerous interactions. Generic questions like "Do you take any supplements?" get vague answers. Specific ones get real ones.
Use California’s "Talk to the Expert" campaign as your script: "I want to make sure my supplements aren’t messing with my meds. Can we check?"
And if they brush you off? Go to another pharmacy. Pharmacists who don’t take supplement safety seriously aren’t serving you well.
What You Should Never Do
Stop taking your meds or supplements without talking to someone. That’s just as dangerous as mixing them wrong.
Don’t assume "natural" means safe. Don’t trust labels that say "pure" or "premium." Don’t believe marketing claims about "boosting immunity" or "detoxing." And don’t rely on internet forums or YouTube videos for medical advice.
Look for third-party verification on your supplement bottles: USP, NSF, or ConsumerLab. These logos mean the product was tested for what’s actually inside. It doesn’t guarantee safety, but it’s a start.
When to Schedule a Follow-Up
Don’t treat this as a one-time chat. Your body changes. Your meds change. Your diet changes.
Revisit this conversation:
- Every time you get a new prescription
- When you start or stop a supplement
- After a major diet change (like going vegan or keto)
- If you feel new side effects - fatigue, dizziness, nausea, muscle pain
Many pharmacies now offer free 10-minute supplement reviews. Ask if they have one. If not, ask if you can schedule a 15-minute consultation. It’s your right. And it’s worth it.
Final Thought: You’re the CEO of Your Health
Your pharmacist isn’t your enemy. They’re your ally. But they can’t help if they don’t know the full picture. The system isn’t perfect. Supplements aren’t regulated. Doctors don’t always ask. But you can fill the gap.
Take the list. Ask the questions. Push for answers. You’re not being difficult. You’re being smart. And in a world where a grapefruit can undo a month of heart medication, that’s not just advice - it’s protection.
Should I tell my pharmacist about vitamins and herbal supplements?
Yes - absolutely. Even common vitamins like B12, D, or magnesium can interact with medications. Herbs like St. John’s wort, ginkgo, or goldenseal can cause serious, even life-threatening reactions when mixed with antidepressants, blood thinners, or heart drugs. Pharmacists need the full list to keep you safe.
Can food really interfere with my medication?
Yes. Grapefruit can make cholesterol and blood pressure drugs dangerously strong. Dairy can block antibiotics like ciprofloxacin. Leafy greens can reduce the effect of warfarin. Even a daily glass of orange juice can interfere with some allergy or heart meds. Your pharmacist can tell you which foods to avoid or time separately from your pills.
How do I know if a supplement is safe?
There’s no perfect way, but look for third-party seals like USP, NSF, or ConsumerLab on the bottle. These mean the product was tested for ingredients and purity. Still, safety depends on your meds. Always check with your pharmacist before starting anything new - even if it’s labeled "natural" or "organic."
What if my pharmacist says a supplement is fine, but I’m still having side effects?
Trust your body. Go back with a list of your symptoms and ask if the supplement could be the cause. Some interactions take weeks to show up. If your pharmacist doesn’t investigate further, ask for a referral to a clinical pharmacist or medication therapy management service. Your health is worth a second opinion.
Can I just stop taking a supplement if I’m worried?
Not without talking to your pharmacist or doctor first. Some supplements, like magnesium or melatonin, are safe to stop quickly. Others, like herbal extracts or high-dose vitamins, can cause withdrawal or rebound effects. Plus, stopping one thing might make another interaction worse. Always get guidance before making a change.
Do pharmacists get enough training on supplements?
Since 2023, all U.S. pharmacy schools are required to teach supplement interactions. But real-world practice varies. Many pharmacists still don’t ask about supplements unless patients bring it up. That’s why you need to lead the conversation. Don’t wait for them to know - tell them what you’re taking.
Are there supplements that are generally safe with most meds?
Some have low interaction risk when used properly - like vitamin C in standard doses, or a basic multivitamin without megadoses. But "generally safe" doesn’t mean "always safe." Even a simple calcium pill can block antibiotics. Always check with your pharmacist. There’s no universal green light - only context-specific safety.
Can I use my pharmacy’s app to check for interactions?
Some apps can help, but they’re not foolproof. Many don’t include supplements, or they use outdated databases. A 2025 study found that even pharmacy apps missed 40% of known supplement-drug interactions. Use them as a starting point, not a final answer. Always confirm with your pharmacist.
How often should I review my supplements with my pharmacist?
At least once a year - and every time you start or stop a medication, change your diet, or feel new side effects. Your body changes. Your meds change. Your supplement needs change. Regular check-ins are part of responsible health management, not an extra chore.
What if I can’t afford to buy all the supplements my pharmacist recommends?
Tell them. Many pharmacists know about patient assistance programs, generic brands, or discount cards. Some pharmacies offer free samples of essential supplements like vitamin D or B12 for patients on long-term meds. Never assume cost means you can’t get help - ask. Your pharmacist’s job is to make your treatment work, not just sell products.
Supplements and food aren’t the enemy. But treating them like harmless extras is. The truth is, your pharmacist is one of the most underused resources in healthcare. They’re not just the person who hands you your pills. They’re the one who can tell you if that green smoothie is saving your heart - or sabotaging your blood thinner. Don’t wait for them to ask. Ask them first.




Asia Roveda
November 25, 2025 AT 17:59 PMSo let me get this straight - you’re telling me I need to list every damn vitamin I take like I’m signing a CIA contract? I take B12 and fish oil. That’s it. And now I’m supposed to walk into a pharmacy with a spreadsheet? LOL. Next they’ll want my grocery receipts.
Micaela Yarman
November 27, 2025 AT 00:54 AMIt is imperative to recognize that the current regulatory vacuum surrounding dietary supplements constitutes a profound public health vulnerability. The absence of pre-market verification protocols permits the proliferation of adulterated products, thereby placing patients at significant risk of iatrogenic harm. It is incumbent upon the layperson to assume proactive responsibility for disclosing all ingestibles to licensed pharmacists, who serve as the final bulwark against pharmacokinetic catastrophe.
Cynthia Springer
November 28, 2025 AT 09:27 AMI’ve been taking turmeric for my knees and metformin for prediabetes. I never thought they’d interact. But now I’m wondering - does the curcumin mess with how metformin gets absorbed? I’ve had weird stomach cramps lately. Should I space them out or just stop the turmeric? I don’t want to be one of those people who ‘just takes herbs’ and ends up in the ER.
Marissa Coratti
November 29, 2025 AT 04:52 AMLet me be unequivocally clear: the notion that supplements are ‘harmless’ is not merely incorrect - it is a dangerously pervasive cultural delusion perpetuated by wellness influencers and supplement marketers who profit from your ignorance. The FDA’s regulatory framework for dietary supplements was designed in 1994 to protect corporate interests, not public safety. Consequently, the market is flooded with products containing undisclosed pharmaceuticals, heavy metals, and untested botanical extracts. When you ingest ‘St. John’s wort’ from a store shelf, you are not ingesting a standardized herbal extract - you are ingesting a gamble. And when you combine that with SSRIs? You are courting serotonin syndrome - a condition that can kill you in hours. This is not hyperbole. This is pharmacology. Your pharmacist is not a clerk. They are a clinical scientist trained to interpret drug-metabolizing enzyme interactions. You owe them the truth - not because it’s polite, but because your life depends on it.
Rachel Whip
November 30, 2025 AT 21:04 PMI work in a pharmacy and I can tell you - the people who get it right are the ones who come in with a list. Not ‘I take vitamins.’ Not ‘I use herbal stuff.’ Actual names, doses, times. One guy brought a photo of his supplement cabinet. We caught he was taking ginkgo with warfarin - he was about to bleed out. We got him switched to a different blood thinner. You don’t need to be a genius. Just be organized. It saves lives.
Ezequiel adrian
December 1, 2025 AT 16:18 PMbro i take ashwagandha and lisinopril and i just thought it was chill 😌 but now im scared lmao should i stop? 🤔
Joe bailey
December 2, 2025 AT 22:55 PMThis is such a vital topic - seriously, why isn’t this taught in high school? I used to think ‘natural’ meant safe, until my mom ended up in the hospital because she took garlic pills with her blood thinner. She didn’t even know it was a problem. We need more awareness, not more ads for ‘immune-boosting’ powders that do nothing but empty your wallet. Talk to your pharmacist. It’s not weird. It’s smart.
Amanda Wong
December 4, 2025 AT 16:44 PMOf course you should tell your pharmacist. But let’s be real - most of them don’t know anything. They’re just cashiers with a white coat. I asked mine about milk thistle and my statin, and she said ‘Oh, that’s fine!’ - then I looked it up myself and found it can increase liver toxicity. Don’t trust them. Trust your own research. And if you’re gonna take supplements, buy only USP-certified ones - anything else is snake oil.
Stephen Adeyanju
December 5, 2025 AT 12:43 PMSo grapefruit messes with my blood pressure med huh well guess what I eat half a grapefruit every morning and I feel great so maybe your ‘science’ is wrong maybe my body knows better
james thomas
December 5, 2025 AT 22:08 PMLet me guess - the FDA is in on this. They don’t regulate supplements because they’re working with Big Pharma to keep you dependent on pills. Your pharmacist? Probably on commission for selling you overpriced ‘premium’ vitamins. They want you scared so you’ll buy more. St. John’s wort? It’s been used for centuries. The real danger is the pharmaceutical monopoly. Don’t be a sheep. Question everything.
Sanjay Menon
December 6, 2025 AT 08:08 AMIt is both tragic and predictable that the average American confuses dietary supplementation with therapeutic intervention. One does not ‘boost immunity’ with a capsule of echinacea any more than one ‘detoxifies’ the liver with a $30 bottle of dandelion root. The pharmacological literacy of the populace has collapsed into a morass of Instagram wellness gurus and Amazon influencer marketing. The true tragedy is not the interactions - it is the surrender of critical thinking to commodified pseudoscience.
Brittany Medley
December 7, 2025 AT 02:47 AMI’m a nurse, and I’ve seen too many patients come in with weird side effects - fatigue, dizziness, muscle pain - and it turns out they’ve been taking magnesium with their blood pressure med, or iron with their antibiotic. Just write it down. Keep a small notebook. Even if you think it’s ‘nothing.’ I promise you, your pharmacist will thank you. And you’ll sleep better knowing you didn’t accidentally poison yourself.
Ali Miller
December 7, 2025 AT 23:39 PMWhy do we even have pharmacies if the government won’t regulate supplements? This is a corporate scam. The FDA doesn’t care. Big Pharma doesn’t care. Your pharmacist? Probably got trained on this for 20 minutes in pharmacy school and forgot it by Tuesday. I’m not trusting my life to a guy who’s counting out ibuprofen while scrolling TikTok. I’m going to a naturopath who actually knows what’s in my supplements. At least they admit they’re not doctors.
JAY OKE
December 8, 2025 AT 20:47 PMYeah I’ve been taking vitamin D and fish oil with my thyroid med for years. Never had an issue. Maybe the article is overblown? I mean, I’m not dying, right? Maybe just keep taking what works and don’t stress?
Deborah Williams
December 10, 2025 AT 05:41 AMIt’s funny how we’ve turned healthcare into a transactional checklist - ‘List your supplements.’ ‘Ask your pharmacist.’ ‘Check for interactions.’ But what if the real problem is that we’ve outsourced our health to experts while abandoning our own intuition? You don’t need a 10-minute consultation to know that if you feel weird after taking something, you should stop. Maybe the answer isn’t more lists - maybe it’s more self-awareness. Or maybe we’re just too busy scrolling to notice our own bodies screaming.