When a patient walks into the ER with shortness of breath, the clock starts ticking. Is it heart failure? COPD? A pulmonary embolism? In the past, doctors relied on chest X-rays, EKGs, and clinical gut feelings. Now, there’s a simple blood test that can cut through the noise: NT-proBNP. This isn’t just another lab order-it’s one of the most reliable tools we have to rule out heart failure in minutes, not days.
What NT-proBNP Actually Measures
NT-proBNP stands for N-terminal pro-B-type Natriuretic Peptide. It’s a piece of a hormone your heart releases when it’s under stress-like when the ventricles are stretched from too much fluid or high pressure. Think of it as your heart screaming for help in chemical form. The test measures this fragment in the blood, and the higher the number, the more likely your heart is struggling.
Unlike BNP, which breaks down quickly in the bloodstream, NT-proBNP is stable. That means you can draw the blood, send it to the lab, and even wait a few hours without the result going bad. It’s why most hospitals now use NT-proBNP instead of BNP. The Roche Elecsys assay, the most common one in the U.S., can detect levels as low as 5 pg/mL and goes up to 35,000 pg/mL. Results typically come back in under an hour.
When to Order NT-proBNP: The 5 Key Scenarios
Not every patient with breathing trouble needs this test. But if they fit one of these five situations, you’re missing a critical opportunity if you don’t order it.
- Suspected acute heart failure-especially in patients over 65 with new-onset dyspnea, fatigue, or edema. If the NT-proBNP is below 300 pg/mL, heart failure is effectively ruled out with 98% confidence. That’s huge. It means you can avoid unnecessary hospital admissions, echocardiograms, and CT scans.
- Emergency department triage-NICE guidelines in the UK and ESC guidelines in Europe both recommend NT-proBNP as a first-line test for all patients presenting with acute dyspnea. A 2022 UK audit showed a 19% drop in unnecessary echocardiograms after implementing this protocol.
- Patients with ambiguous symptoms-Think of the 82-year-old with COPD who’s wheezing. Is it worsening lung disease or early heart failure? An NT-proBNP of 120 pg/mL tells you it’s probably not the heart. One cardiologist on Reddit shared how this saved a $3,000 echo and led to the right diagnosis: a COPD flare.
- Monitoring high-risk patients-If someone has diabetes, hypertension, or prior heart attack, their NT-proBNP level can serve as an early warning system. Rising levels over time, even within normal range, can signal developing dysfunction before symptoms appear.
- Post-ACS risk stratification-Starting in 2024, new ACC/AHA guidelines will expand NT-proBNP use to patients after a heart attack. Studies show those with elevated levels after an acute coronary syndrome have a 35% higher risk of death or hospitalization within a year. This test helps identify who needs more aggressive follow-up.
How to Interpret the Numbers: Age, Kidneys, and Obesity
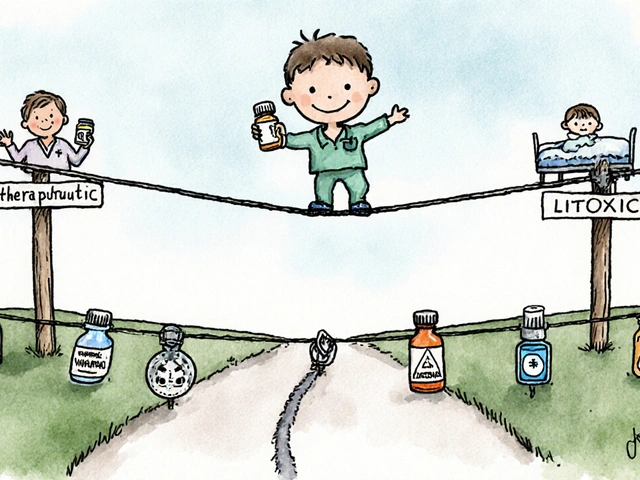
Here’s where things get tricky. NT-proBNP isn’t a yes/no number. It’s a sliding scale that changes with age, kidney function, and body weight.
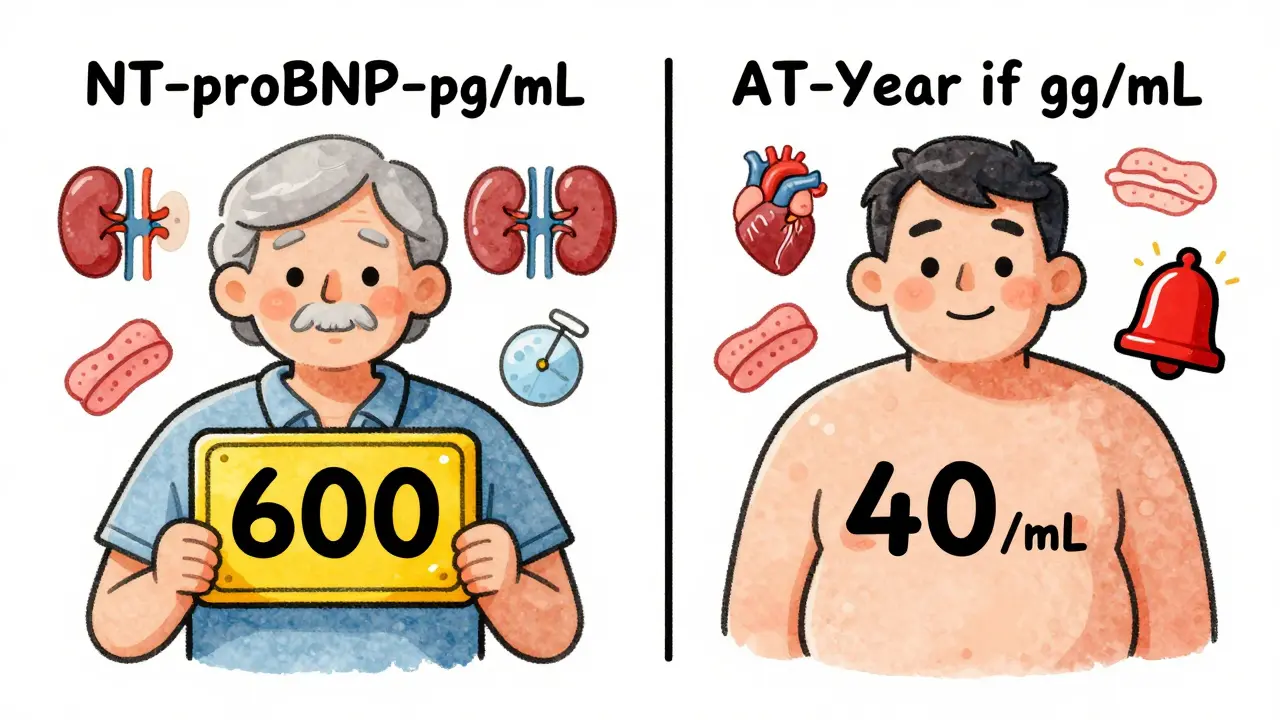
Age matters. Levels naturally rise about 15-20% every decade after age 50. So a 70-year-old with 600 pg/mL might be perfectly normal, while the same number in a 40-year-old is a red flag. ESC guidelines use age-adjusted cutoffs: under 50 = 450 pg/mL, 50-75 = 900 pg/mL, over 75 = 1,800 pg/mL. Don’t use a one-size-fits-all number.
Kidney disease changes everything. If a patient has CKD stage 3 or worse, NT-proBNP levels can be 28-40% higher than normal-even without heart failure. That’s because the kidneys clear the peptide. So if someone with stage 4 kidney disease has a level of 1,100 pg/mL, that doesn’t mean they have acute heart failure. Use a modified cutoff of <1,200 pg/mL for rule-out in these patients.
Obesity lowers levels. Fat tissue absorbs some of the peptide, so obese patients often have lower readings than expected. For every 5-point increase in BMI, NT-proBNP drops 25-30%. That means you might miss heart failure in someone who’s overweight if you rely on standard cutoffs. Always combine the number with physical exam findings and symptoms.
What NT-proBNP Won’t Tell You
This test is powerful, but it’s not magic. It doesn’t diagnose the cause of heart failure. It doesn’t tell you if it’s systolic or diastolic. It won’t tell you if the patient has atrial fibrillation, pulmonary hypertension, or sepsis-all of which can raise NT-proBNP.
Dr. Allan Jaffe from Mayo Clinic puts it bluntly: “NT-proBNP should never be used in isolation.” A 78-year-old with AFib, CKD, and a level of 850 pg/mL? That’s a classic gray zone. You need the full picture: lung sounds, jugular venous pressure, leg swelling, chest X-ray, maybe even an echo. The test is a gatekeeper-not the whole diagnosis.
What’s New in 2026
Point-of-care testing is finally here. In late 2023, the FDA cleared Roche’s Cobas h 232-a device that gives NT-proBNP results in 12 minutes at the bedside. It’s already being rolled out in ERs and ICUs. Concordance with lab results? 94.7%. That means you can make decisions in real time, not wait for a lab report.
Also, starting January 2025, Medicare began requiring prior authorization for NT-proBNP tests in asymptomatic patients. Why? Because 18% of tests were being ordered on people with no symptoms-mostly in nursing homes or during routine checkups. That’s waste. The test has value only when symptoms are present.

Why This Test Saves Time and Money
Here’s the bottom line: if you order NT-proBNP in the right patients, you reduce unnecessary hospitalizations, avoid expensive imaging, and shorten ER stays. A 2022 JAMA study found hospitals with standardized NT-proBNP protocols cut inappropriate testing by 33%. That’s not just efficiency-it’s better care.
And the cost? Medicare pays $18.42 per test. Compare that to a $3,000 echocardiogram or a $1,500 CT pulmonary angiogram. One test can prevent dozens of them.
Cardiologists surveyed in 2023 said 89% consider NT-proBNP “essential.” Seven out of ten say it’s prevented at least one unnecessary admission per month.
Common Pitfalls and How to Avoid Them
- Ordering it too early-Don’t test someone with stable COPD and no new symptoms. Wait until they’re acutely unwell.
- Ignoring age and kidney function-Using the same cutoff for everyone leads to misdiagnosis. Always adjust.
- Overinterpreting borderline values-A level of 400 pg/mL in a 70-year-old with hypertension? Probably not heart failure. But if they’re also swollen and breathless? It’s a signal to dig deeper.
- Forgetting to correlate-A normal NT-proBNP doesn’t rule out all causes of dyspnea. Always look at the whole picture.
There’s a free hotline-1-800-NT-PROBNP-run by the Heart Failure Society of America. They get over 1,200 calls a month from clinicians stuck on tricky cases. Use it.
Final Thought
NT-proBNP isn’t just a lab test. It’s a decision-making tool. Used right, it prevents overtesting, reduces hospital stays, and gets patients the right care faster. Used wrong, it leads to false reassurance or unnecessary panic. The science is solid. The guidelines are clear. The tools are available. The question isn’t whether to use it-it’s whether you’re using it well.
Is NT-proBNP the same as BNP?
No. NT-proBNP is the inactive fragment of the same hormone that BNP comes from. BNP is the active hormone that helps the body get rid of fluid. NT-proBNP doesn’t have biological activity, but it’s more stable in the blood, making it better for testing. Most labs now use NT-proBNP because it’s less affected by delays in sample processing.
Can NT-proBNP be used to diagnose heart failure in young patients?
Yes, but the cutoff is lower. For patients under 50, a level above 450 pg/mL is considered abnormal and suggests heart failure. In younger patients, elevated NT-proBNP is often linked to conditions like myocarditis, congenital heart disease, or severe hypertension. Always combine it with clinical signs-like a new murmur, gallop rhythm, or signs of fluid overload.
What if NT-proBNP is normal but I still suspect heart failure?
A normal NT-proBNP (<300 pg/mL) rules out acute heart failure with 98% accuracy. If the patient still has symptoms, look elsewhere: lung disease, anemia, anxiety, or even a pulmonary embolism. Don’t order an echo just because the patient feels short of breath. NT-proBNP’s strength is ruling out-not ruling in.
Do I need to repeat the NT-proBNP test during hospitalization?
Not routinely. The initial value is most useful for diagnosis. Repeating it during admission doesn’t change management unless the patient is deteriorating. If levels drop significantly after treatment, it’s a good sign. If they rise, it may mean the treatment isn’t working or the diagnosis was wrong. But don’t order it just to check-use it to guide therapy only if the patient’s condition changes.
Can obesity cause a false low NT-proBNP?
Yes. Fat tissue absorbs NT-proBNP, so obese patients often have lower levels than expected-even if their heart is failing. Studies show levels drop 25-30% for every 5-point increase in BMI. That means a patient with a BMI of 35 might have a reading of 200 pg/mL even with moderate heart failure. Always interpret results in context. If symptoms are strong but the number is low, trust the clinical picture over the number.
Is NT-proBNP testing covered by insurance?
Yes, in most cases. Medicare pays $18.42 per test, and private insurers typically cover it when ordered for suspected acute heart failure or acute dyspnea. Starting in 2025, prior authorization is required for testing in asymptomatic patients to prevent overuse. As long as the patient has symptoms and the test is medically justified, coverage is standard.




Daniel Dover
February 15, 2026 AT 02:30 AMThis is one of those tests that should be in every ER protocol. Simple, fast, and saves so much time and money. I've seen patients get discharged within an hour because of it.
Josiah Demara
February 16, 2026 AT 02:43 AMYou're overselling this. NT-proBNP is useless in obese patients and those with renal disease. Half the time it's just noise. And don't get me started on how hospitals treat it like a magic bullet.
Kaye Alcaraz
February 16, 2026 AT 10:18 AMI appreciate how you laid out the clinical scenarios. This test has changed how we triage in my unit. We've cut unnecessary admissions by nearly 30% since implementing the age-adjusted cutoffs. Thank you for the clear guidance.
Betty Kirby
February 17, 2026 AT 19:07 PMThe fact that we're still debating whether to order this test in 2024 is ridiculous. It's not even close to controversial. If you're not using NT-proBNP for dyspnea, you're practicing medicine from 2005.
Virginia Kimball
February 19, 2026 AT 00:24 AMI love how this test turns guesswork into science. Last week, a 78-year-old came in with 'just a cough'-NT-proBNP was 2100. Turned out to be early HF. We caught it before she crashed. This is why I love cardiology.
Kapil Verma
February 20, 2026 AT 04:40 AMIn India, we don't even have access to this test in 80% of rural hospitals. You Americans act like this is common sense. Meanwhile, my cousin in Bihar died because they didn't have the machine to run it. This is elitist healthcare.
Mandeep Singh
February 21, 2026 AT 06:34 AMYou think this is revolutionary? In Mumbai, we've been using NT-proBNP for over a decade. The real issue is that Western guidelines ignore global variability. Renal cutoffs? Age adjustments? We've been adjusting for decades. Your guidelines are just catching up.
Mike Hammer
February 22, 2026 AT 18:38 PMi once saw a guy with an nt-probnp of 8000 and no symptoms. turned out he was just really dehydrated. sometimes the numbers lie. also, why do we always blame the heart? could be a bad thyroid. or anxiety. or just old age.
Joe Grushkin
February 23, 2026 AT 15:32 PMLet me guess-this was written by someone who got paid by Roche. NT-proBNP is expensive, it’s overused, and it’s turning primary care into a lab report reading contest. Real medicine is listening. Not chasing biomarkers.
Erica Banatao Darilag
February 24, 2026 AT 22:58 PMi think this is really important. i just wish more docs knew how to interpret it. i had a patient last month with a level of 700 and everyone thought it was heart failure. turns out she had stage 3 ckd and was on diuretics. it's not just the number-it's the context.
Michael Page
February 25, 2026 AT 16:25 PMThe real question isn't whether to order it-it's what we do with the data. We're drowning in numbers and starving for wisdom. NT-proBNP doesn't diagnose heart failure. It reveals the heart's distress call. The real diagnosis is the human story behind the number.
Charlotte Dacre
February 27, 2026 AT 09:00 AMOh look, another study that proves doctors love to order tests they can't explain. Next you'll be telling us to check cortisol for coffee cravings.
Esha Pathak
February 28, 2026 AT 17:10 PMI'm from Delhi and we use this test daily. But here's the truth: no one in rural India has access. We need to stop talking about guidelines and start talking about equity. This test is life-saving… if you can afford it. 🙏
Chiruvella Pardha Krishna
March 1, 2026 AT 20:01 PMPerhaps the deeper issue is that we've outsourced clinical judgment to algorithms. NT-proBNP is a tool-not a replacement for intuition. The patient who smiles while saying 'I can't catch my breath' still needs to be heard.
Sarah Barrett
March 3, 2026 AT 15:52 PMI've been practicing for 22 years. When I first saw NT-proBNP in the 2000s, I thought it was hype. Now I can't imagine managing dyspnea without it. The evidence is overwhelming. This isn't trend-following-it's evidence-based evolution.