Managing bipolar disorder isn’t about finding one magic pill-it’s about finding the right balance between control and comfort.
For millions of people living with bipolar disorder, medication is not optional. It’s the foundation. But too many people stop taking their meds-not because they don’t believe in them, but because the side effects feel worse than the illness. Weight gain so heavy you can’t recognize yourself. Constant thirst that doesn’t go away. Brain fog that turns simple tasks into nightmares. These aren’t rare side effects. They’re common. And they’re why nearly half of people with bipolar disorder quit their medication within a year.
The truth? Mood stabilizers and antipsychotics work. But they’re not perfect. And the best treatment isn’t the one with the strongest science on paper-it’s the one you can actually live with.
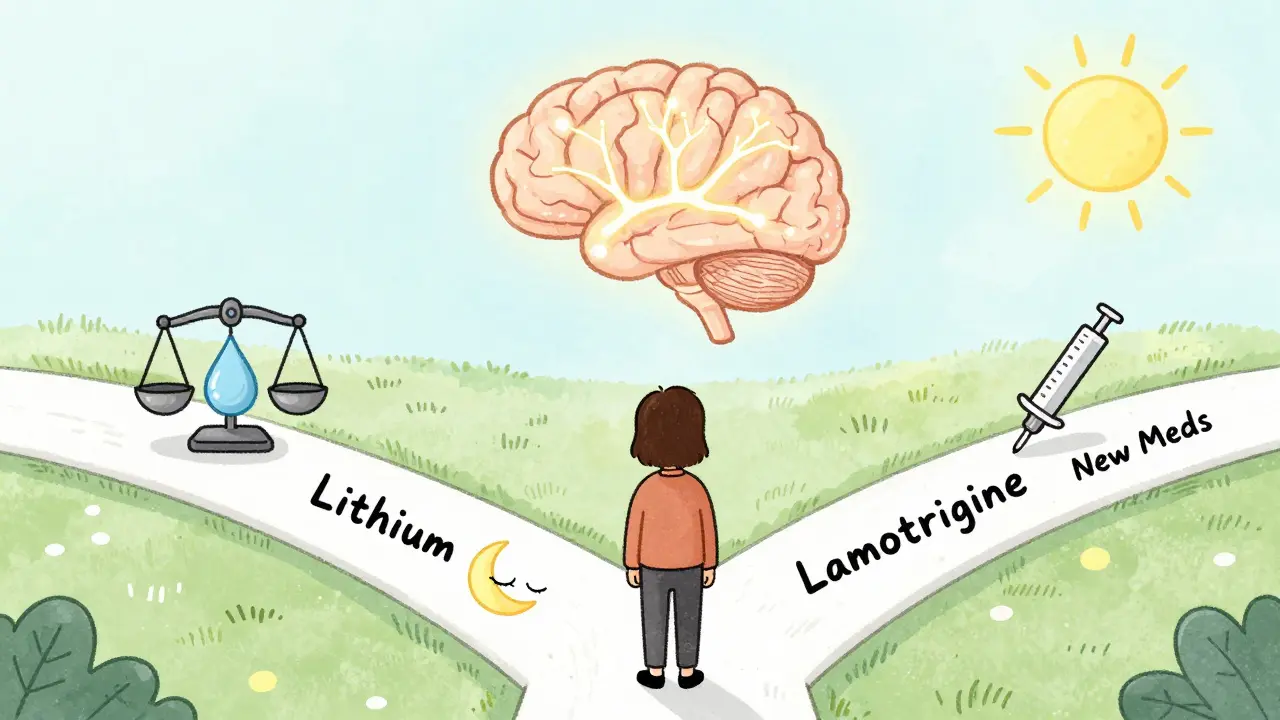
Lithium: The Original, Still the Most Powerful
Lithium has been around since the 1970s, and it’s still the most studied mood stabilizer for bipolar disorder. It doesn’t just calm mania-it prevents suicide. Studies show people taking lithium have an 80% lower risk of dying by suicide than those on placebo. That’s not a small benefit. That’s life-saving.
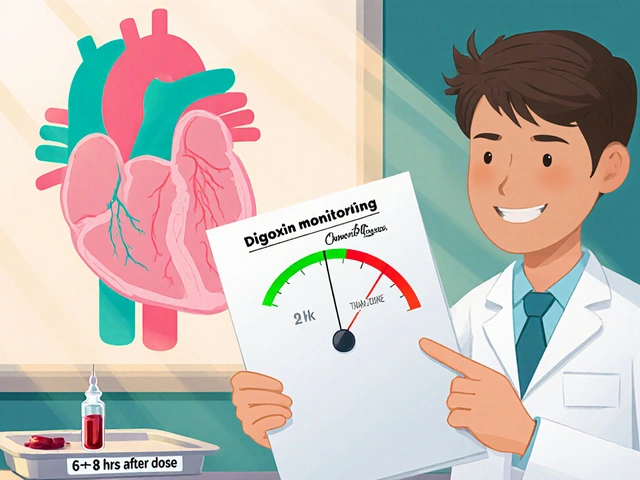
But lithium isn’t easy. You need regular blood tests. Every week at first, then every few months once you’re stable. The goal? Keep your blood level between 0.6 and 1.0 mmol/L. Too low? It won’t work. Too high? You risk toxicity-slurred speech, shaky hands, even seizures. That’s why doctors start low: 300 mg a day, then slowly increase every few days while watching your blood levels.
Side effects? Almost everyone gets them. Thirst and frequent urination hit 30-40% of users. You might drink three liters of water a day and still feel dry. Tremors in your hands? That’s common. Weight gain? On average, 10 to 15 pounds in the first year. Nausea? Happens to 20-30%. Some people manage by taking lithium with food. Others split their dose-half in the morning, half at night-to make it easier on their stomach.
Still, for many, it’s worth it. One Reddit user wrote: “After three meds failed, lithium finally stopped my weekly suicidal depression. I gained 15 pounds. But I’m alive.”
Antipsychotics: Faster Relief, Heavier Costs
If lithium feels slow, antipsychotics like quetiapine (Seroquel), olanzapine (Zyprexa), and aripiprazole (Abilify) move faster. Quetiapine can start working in as little as seven days. That’s a big deal when you’re in the middle of a depressive episode or a manic crash.
Quetiapine is especially used for bipolar depression. In clinical trials, over half of people taking it saw real improvement-compared to just 32% on placebo. But the trade-off? Weight gain. On average, users gain 4 to 6 kilograms in six weeks. That’s not just a few pounds-it’s a change in how you feel in your own skin. Metabolic risks climb too: 20-30% higher chance of developing type 2 diabetes with olanzapine. Sedation is another issue-60-70% of people on quetiapine feel drowsy, sometimes all day.
And it’s not just quetiapine. Olanzapine causes more weight gain than any other antipsychotic. Risperidone can trigger akathisia-a restlessness so intense you can’t sit still. Aripiprazole has less weight gain but can cause jitteriness or insomnia.
On PatientsLikeMe, users gave quetiapine a 3.7 out of 5 for effectiveness, but only 2.8 for tolerability. Two-thirds reported weight gain averaging 22 pounds. That’s not a side effect-it’s a lifestyle shift.
Lamotrigine: The Depression Specialist
Not all mood stabilizers are created equal. Lamotrigine (Lamictal) doesn’t help much with mania. But for depression? It’s one of the best. In trials, 47% of people on lamotrigine improved-compared to 28% on placebo. And unlike lithium or antipsychotics, it doesn’t cause weight gain. Many users report no change in appetite.
But here’s the catch: lamotrigine can cause a rare but dangerous skin rash. The risk is low-about 1% overall-but it can turn into Stevens-Johnson syndrome, a life-threatening condition. That’s why doctors start at 25 mg and increase by 25 mg every two weeks. Rushing the dose increase is the #1 mistake. Slow and steady saves lives.
Some users hate it for the opposite reason: insomnia. One Reddit user said, “Lithium made me thirsty. Lamotrigine kept me awake for nights on end. I had to switch again.”
Combination Therapy: When One Drug Isn’t Enough
Many people need more than one medication. That’s where combination therapy comes in: a mood stabilizer plus an antipsychotic. This approach works for about 70% of treatment-resistant cases. If lithium alone isn’t enough, adding quetiapine or lurasidone can push you into remission.
But combining drugs doubles the side effect risk. You might get the mood control you need-but also the weight gain, fatigue, and metabolic issues from both. A 2003 study found combination therapy increased side effects by 25-30%. That’s why doctors don’t start here. They start with one, then add only if needed.
Some newer antipsychotics like lumateperone (Caplyta) were designed to avoid this. Approved in 2023 for bipolar depression, it causes only 0.8 kg of weight gain in six weeks-far less than quetiapine’s 3.5 kg. That’s a big win for people who’ve struggled with weight gain.
Monitoring: What Your Doctor Should Be Checking
Medication isn’t a set-it-and-forget-it deal. It needs tracking. The American Psychiatric Association says you need quarterly checks for:
- Weight and waist size (over 40 inches for men, 35 for women = metabolic risk)
- Fasting blood sugar
- Lipid panel (cholesterol and triglycerides)
- Thyroid and kidney function (especially if you’re on lithium)
For lithium users, blood tests are non-negotiable. If you skip them, you’re gambling with your kidneys and brain. For antipsychotic users, skipping metabolic checks means missing early signs of diabetes-signs you can still reverse if caught in time.
Also watch for drug interactions. NSAIDs like ibuprofen can spike lithium levels by 25-60%. That’s dangerous. Many antipsychotics interact with over 40 common medications. Always tell your doctor what else you’re taking-even supplements.
Why People Quit-and What to Do Instead
A 2022 NAMI survey found 45% of people with bipolar disorder stopped their meds because of side effects. Top reasons? Weight gain (78%), brain fog (65%), and sexual dysfunction (52%).
But quitting doesn’t fix the problem. It makes it worse. Without treatment, relapse rates jump to 80% within two years. Suicidal episodes become more frequent.
So what’s the alternative? Don’t quit. Talk. Adjust. Switch.
If weight gain is crushing you, ask about metformin. It’s not a mood stabilizer-but it helps reverse insulin resistance caused by antipsychotics. Many users report losing 10-20 pounds after adding it.
If sedation is too much, ask about switching to aripiprazole or lurasidone. If tremors from lithium are unbearable, try valproate. If lamotrigine gives you insomnia, try adding a low-dose trazodone at night.
There’s no shame in trying again. The first med you try rarely works perfectly. It’s the third or fourth that often clicks.
The Future: Personalized Treatment Is Here
Genetic testing is starting to change the game. Companies like Genomind test for CYP2D6 and CYP2C19 gene variants-enzymes that break down most bipolar meds. If you’re a slow metabolizer, standard doses can overload your system. If you’re fast, they won’t work at all. Testing can improve medication selection accuracy by 30%.
Long-acting injectables like Abilify Maintena are another shift. Instead of swallowing a pill daily, you get one shot every month. No more forgetting. No more daily guilt. Just steady levels.
And new drugs are coming. Ketamine derivatives, glutamate modulators-these aren’t sci-fi. They’re in trials. They could offer rapid relief for depression without the weight gain.
But here’s the bottom line: none of this replaces the core truth. Lithium still reduces suicide risk more than anything else. Antipsychotics still stop mania faster. The goal isn’t to find the perfect drug. It’s to find the right one for you.
What Works for One Person Won’t Work for Another
There’s no universal answer. One person thrives on lithium. Another can’t tolerate it. One finds peace with quetiapine. Another can’t sleep or eat after starting it. That’s not failure. That’s biology.
What matters is this: you’re not broken because your first med didn’t work. You’re not weak because you struggled with side effects. You’re doing the hardest thing possible-you’re trying to stay alive while your brain fights you.
Keep talking. Keep tracking. Keep adjusting. The right balance is out there. It might take time. But it’s worth it.
Can you treat bipolar disorder with just one medication?
Yes, some people do. Lithium or lamotrigine can be enough for mild to moderate cases. But for severe mania or treatment-resistant depression, most people need a combination-usually a mood stabilizer plus an antipsychotic. About 70% of those who don’t respond to one drug improve with two.
Do antipsychotics make you gain weight no matter what?
Not all of them. Olanzapine and quetiapine cause the most weight gain-often 10-20 pounds in a few months. But lurasidone, cariprazine, and lumateperone have minimal weight effects. Aripiprazole is in the middle. If weight is a concern, ask your doctor about switching to one of the newer, metabolically neutral options.
Is lithium dangerous long-term?
It can be, if not monitored. Long-term lithium use can affect kidney function and thyroid health. But with regular blood tests (every 3-6 months), most people stay safe. Many live on lithium for decades without major issues. The risk of kidney damage is higher if you’re dehydrated or take NSAIDs regularly. Staying hydrated and avoiding ibuprofen helps.
Can you use antidepressants for bipolar depression?
Some doctors use them cautiously, but only with a mood stabilizer attached. Without one, antidepressants can trigger mania in 10-25% of people. SSRIs like fluoxetine have a 50% response rate in bipolar depression-but only when paired with lithium or valproate. Many experts avoid them entirely because the risk often outweighs the benefit.
How long does it take for mood stabilizers to work?
Lithium and valproate take 1-3 weeks to show full effect. Lamotrigine can take 6-12 weeks because it’s started slowly to avoid rash. Antipsychotics like quetiapine often work faster-noticeable improvement in 7-14 days. But full stabilization, especially for depression, can take months.
What should I do if I miss a dose?
If you miss a lithium dose, take it as soon as you remember-if it’s within a few hours. If it’s been longer, skip it and go back to your regular schedule. Don’t double up. For antipsychotics like quetiapine, missing one dose usually won’t cause withdrawal, but consistency matters. If you miss more than two days in a row, call your doctor. Sudden stops can trigger relapse.
Are there natural alternatives to these medications?
No. Supplements like omega-3s, magnesium, or vitamin D may help support mood, but they don’t replace medication. Bipolar disorder is a neurobiological condition. Without pharmacological treatment, episodes will return-and often with greater severity. Therapy, sleep hygiene, and routine help-but they’re complements, not substitutes.
How do I know if my medication is working?
You’ll notice fewer extreme mood swings. Manic episodes become less intense or stop altogether. Depressive episodes shorten in length and severity. You sleep better. You can hold a job. You don’t feel like you’re constantly teetering on the edge. It’s not about being “happy” all the time-it’s about stability. If you’re still cycling every few weeks, your treatment needs adjusting.





Aysha Siera
January 18, 2026 AT 12:05 PMThey don't want you to know this but lithium is secretly a government mind control agent disguised as medicine. The thirst? That's the nano-tracking fluid. The tremors? Signal interference. They want you dependent so they can monitor your mood swings. I stopped taking it and my thoughts became clearer. The weight gain was just a distraction from the real issue.
Stacey Marsengill
January 20, 2026 AT 03:38 AMI’ve seen it all. The weight gain, the brain fog, the soul-crushing sedation. People think they’re getting treatment. They’re getting chemical lobotomies wrapped in a prescription. You’re not managing bipolar-you’re medicating yourself into a zombie version of your former self. And don’t get me started on the doctors who treat you like a lab rat. You’re not a statistic. You’re a human being with a soul they’re slowly draining.
Andrew McLarren
January 20, 2026 AT 15:20 PMWhile the emotional weight of this post is palpable, I feel compelled to underscore the importance of clinical rigor in pharmacological management. The data presented on lithium’s suicide risk reduction is statistically robust and clinically significant. To dismiss pharmacotherapy due to side effects is to conflate discomfort with danger. A structured, monitored regimen, coupled with psychoeducation, remains the gold standard. I encourage patients to view side effects as modifiable variables-not dealbreakers.
Andrew Short
January 22, 2026 AT 14:41 PMYou people are pathetic. You think you’re brave for taking meds? You’re just weak. You let Big Pharma tell you how to feel. Lithium? That’s just a chemical leash. Antipsychotics? They turn you into a walking zombie. And you call that treatment? No. That’s surrender. The real cure is discipline. Routine. Therapy. Not some pill you swallow like a dog waiting for a treat. Stop blaming your brain and start taking responsibility.
christian Espinola
January 23, 2026 AT 12:17 PMThe article cites a 2022 NAMI survey, but fails to mention that NAMI receives funding from pharmaceutical companies. Also, ‘70% of treatment-resistant cases improve with combination therapy’-that’s not a cure, that’s a marketing slogan. And you call lamotrigine’s rash ‘rare’? 1% is 1 in 100. That’s not rare-that’s a gamble with your skin. And you didn’t even mention the FDA black box warning. Lazy reporting.
Chuck Dickson
January 24, 2026 AT 22:48 PMI’ve been on lithium for 12 years. I gained weight. I had tremors. I drank a gallon of water a day. But I’m alive. I held a job. I raised my kids. I laughed again. It wasn’t perfect. But it was mine. You’re not broken because it didn’t work the first time. You’re not weak because you cried over the scale. You’re human. And you deserve to feel stable-not perfect. Try again. Talk to your doc. Switch. Adjust. You’ve got this.
Naomi Keyes
January 24, 2026 AT 22:57 PMI’m sorry, but I have to correct a few inaccuracies here. First, lithium’s therapeutic range is 0.6–1.0 mEq/L, not mmol/L-those are not interchangeable units. Second, lamotrigine’s rash incidence is actually 0.3–0.8% in adults when titrated properly, not 1%. Third, the 80% suicide risk reduction is from a meta-analysis of 1990s studies-more recent data suggests 50–60%. Also, you said NSAIDs increase lithium levels by 25–60%-that’s only true with chronic, high-dose use. Please be more precise.
Dayanara Villafuerte
January 25, 2026 AT 01:02 AMLithium = 🥲💧🧠. Lamotrigine = 😴🌙. Quetiapine = 🍔💤. But I’m alive. And I can text my mom without crying. So I’ll take the 15 lbs and the 3 a.m. thirst. 🤷♀️✨ #BipolarAndProud #MedicationIsMyCape
Jodi Harding
January 26, 2026 AT 16:23 PMThey say ‘find the right balance.’ But balance implies choice. I didn’t choose this. I didn’t choose the pills. I didn’t choose the weight gain. I chose to live. That’s not balance. That’s survival. And if that’s the only option, then the system is broken-not me.
Danny Gray
January 27, 2026 AT 14:17 PMInteresting how we frame this as ‘medication vs. self-control.’ But what if the real issue isn’t the drugs-it’s the isolation? The stigma? The fact that we’re expected to manage a neurological condition with no social support, no financial safety net, and no real access to therapy? The pills are just the bandage on a wound that never got stitched. We’re treating symptoms while ignoring the systemic rot.