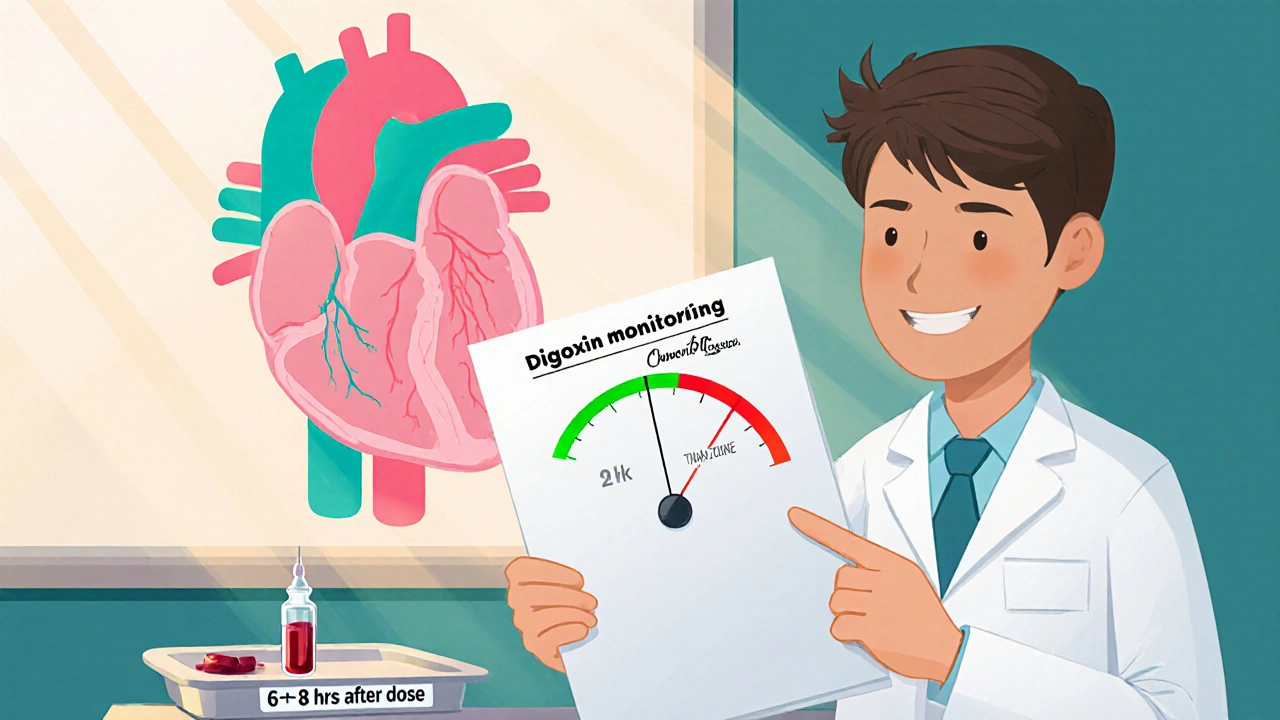
When prescribing digoxin is a cardiac glycoside used to treat heart failure and atrial fibrillation. its narrow safety window means that even small changes in blood concentration can flip the switch from therapeutic benefit to dangerous toxicity. That’s why digoxin monitoring isn’t a box‑checking chore-it’s a lifesaving practice.
What is therapeutic drug monitoring (TDM) and why does it matter for digoxin?
Therapeutic drug monitoring is a clinical process that measures specific drug levels in a patient’s blood at designated times to maintain a concentration within a target range. For digoxin, the therapeutic window is famously tight: the difference between 0.5 ng/mL (effective) and 2.0 ng/mL (toxic) can be a matter of life or death. TDM helps clinicians adjust dosages before adverse effects appear.
How digoxin works in the heart
Digoxin binds to the Na⁺/K⁺‑ATPase pump on cardiac myocytes. By inhibiting this pump, intracellular sodium rises, which indirectly increases calcium influx via the Na⁺/Ca²⁺ exchanger. The added calcium boosts contractility (positive inotropy) and slows conduction through the AV node (negative chronotropy), making it useful for both heart failure and atrial fibrillation.
Defining the therapeutic and toxic serum ranges
The target serum digoxin concentration (SDC) is typically 0.5-0.9 ng/mL for most adults with heart failure. In atrial fibrillation, some clinicians accept up to 1.2 ng/mL because the rate‑controlling effect can outweigh the modest risk increase.
| Level (ng/mL) | Clinical Interpretation |
|---|---|
| 0.5-0.9 | Therapeutic for heart failure |
| 1.0-1.2 | Acceptable for atrial fibrillation, monitor closely |
| > 2.0 | Potential toxicity; act immediately |
Warning signs of digoxin toxicity
- Gastrointestinal upset - nausea, vomiting, loss of appetite
- Visual disturbances - yellow‑green halos, blurred vision
- Arrhythmias - premature ventricular beats, atrioventricular block, ventricular tachycardia
- Neuro‑cognitive changes - confusion, fatigue, dizziness
Because many of these symptoms overlap with heart failure exacerbations, a measured SDC is often the decisive clue.

How to measure digoxin levels accurately
Blood is drawn 6-8 hours after the last dose (steady‑state timing). Immunoassays, such as fluorescence polarization immunoassay (FPIA) or chemiluminescent immunoassay (CLIA), are the standard methods. Laboratories report results in ng/mL; ensure the report includes the assay’s reference range, as methods can differ slightly.
When to check levels - frequency guidelines
- Before initiating therapy - obtain a baseline SDC if the patient is already on digoxin.
- After a dose change - re‑check 6-8 hours after the new dose reaches steady state (usually after 5-7 days).
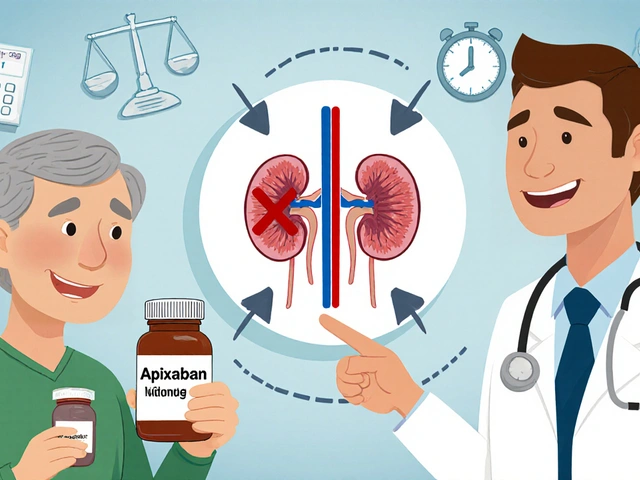
- When renal function shifts - kidneys clear about 50 % of digoxin; any abrupt eGFR change warrants re‑measurement.
- When interacting drugs are added - especially amiodarone, quinidine, verapamil, or certain antibiotics.
- When clinical signs of toxicity appear - don’t wait for lab results; act on the suspicion.
Key patient factors that alter digoxin levels
Renal function is the single biggest determinant of digoxin clearance. An eGFR < 50 mL/min/1.73 m² generally calls for a 25-50 % dose reduction. Age matters too - elderly patients often have reduced muscle mass and lower volume of distribution, increasing serum concentrations. Low potassium level (hypokalemia) sensitises the myocardium to digoxin, raising the risk of arrhythmias. Concurrent medications can either boost digoxin (e.g., amiodarone, quinidine) or lower it (e.g., rifampin, carbamazepine). Finally, body weight influences the loading dose; calculations should be based on lean body mass, not total weight.

Practical steps for clinicians
- Use weight‑based dosing: 0.01 mg/kg loading dose, then 0.125-0.25 mg maintenance depending on renal function.
- Document baseline SDC, eGFR, serum potassium, and any interacting drugs.
- Implement a monitoring schedule in the electronic health record with alerts for overdue labs.
- Educate patients to report visual changes, nausea, or palpitations immediately.
- Consider dose‑adjusted digoxin‑specific antibody fragments (Digibind) for severe toxicity.
Common pitfalls and how to avoid them
1. Assuming stability after the first level. Digoxin can accumulate over weeks; re‑check after any change in renal function or weight.
2. Relying on symptoms alone. Early toxicity is often silent; a routine SDC catches problems before they manifest.
3. Ignoring drug‑drug interactions. Even over‑the‑counter meds like laxatives containing magnesium can shift electrolytes and alter digoxin safety.
Quick checklist for safe digoxin therapy
- Baseline: weight, eGFR, serum potassium, current meds.
- Start dose: 0.01 mg/kg loading (max 0.5 mg), then maintenance 0.125 mg (adjust for renal function).
- First level: 6-8 hours after the third dose (steady state).
- Target SDC: 0.5-0.9 ng/mL (HF) or 0.5-1.2 ng/mL (AF).
- Re‑measure after any dose change, renal decline, new interacting drug, or toxicity signs.
- Patient education: report visual halos, nausea, or irregular heartbeat.
Bottom line
Digoxin’s efficacy hinges on staying inside a razor‑thin therapeutic window. Regular, well‑timed digoxin monitoring-combined with attention to kidney function, electrolytes, and co‑medications-keeps patients benefiting from its powerful inotropic and rate‑controlling effects while steering clear of life‑threatening toxicity.
How often should digoxin levels be checked in a stable patient?
In a clinically stable adult with normal renal function, a level every 6-12 months is sufficient. Any change in kidney function, weight, or concomitant drugs shortens the interval.
Can a low potassium level increase digoxin toxicity?
Yes. Hypokalemia enhances digoxin’s binding to the Na⁺/K⁺‑ATPase pump, making arrhythmias more likely even at therapeutic serum concentrations.
What is the antidote for severe digoxin poisoning?
Digoxin‑specific antibody fragments (e.g., DigiBind) bind free digoxin and are the treatment of choice for life‑threatening toxicity.
Does age alone require dose reduction?
Age per se isn’t a dose‑adjustment factor, but older adults often have reduced renal clearance and lower lean body mass, so a careful review of eGFR and weight is essential.
Which heart conditions benefit most from digoxin?
Digoxin is most useful in systolic heart failure (to improve contractility) and in atrial fibrillation with rapid ventricular response (to slow the heart rate).





sarah basarya
October 26, 2025 AT 17:40 PMOh, the drama of chasing that tiny digoxin window! You think a single dose is a breeze, but the serum level flips like a bad plot twist. If you skip the 6‑8 hour draw, you’re basically gambling with your heart’s rhythm. And those visual halos? Not just a quirky side effect, they’re screaming “stop” in neon. So yes, monitoring isn’t a checkbox-it’s the lifeline you wish you’d set up sooner.
Samantha Taylor
October 30, 2025 AT 05:00 AMIt is truly astonishing how many clinicians treat therapeutic drug monitoring as an optional garnish rather than an essential main course. The pharmacokinetic nuances of digoxin, with its narrow therapeutic index, demand a level of vigilance that borders on the obsessive. One would think that a drug capable of both inotropy and arrhythmogenesis could be left to the whims of “clinical judgment” alone. Yet the literature, replete with case reports of fatal toxicity, leaves no room for such cavalier optimism. The serum concentration window of 0.5 to 0.9 ng/mL for heart failure, extending to a dubious 1.2 ng/mL for atrial fibrillation, is not a suggestion but a hard‑wired safety barrier. Renal function, as you well know, is the single most influential covariate; a sudden dip in eGFR should trigger an immediate re‑check rather than a hopeful “wait and see.” Electrolyte disturbances, especially hypokalemia, act as silent amplifiers of digoxin’s pro‑arrhythmic potential, turning even therapeutic levels into lethal ones. Drug‑drug interactions, such as the infamous trio of amiodarone, quinidine, and verapamil, can double the serum concentration overnight, a fact that is neither obscure nor optional knowledge. Moreover, the timing of the blood draw-6 to 8 hours post‑dose after reaching steady state-cannot be brushed aside as a mere technicality; it is the cornerstone of accurate interpretation. The allure of convenience must not outweigh the grim reality of digitalis‑induced ventricular tachycardia, which, let me remind you, is a leading cause of sudden cardiac death in this patient population. While some practitioners might argue that clinical acumen supersedes laboratory values, the evidence suggests otherwise: reliance on subjective symptomatology alone is a recipe for disaster. In practice, the implementation of automated alerts in electronic health records can bridge the gap between theory and bedside care, ensuring no level is missed. Patient education, too, should be emphasized, because a layperson who notices yellow‑green halos is far more likely to seek help than a clinician who dismisses vague nausea. In short, the mantra should be simple: digoxin is a high‑stakes drug, and monitoring is non‑negotiable. Any deviation from this protocol is, at best, negligent, and at worst, fatal.
Joe Langner
November 2, 2025 AT 16:20 PMhey folks, just want to throw in a little encouragement here – staying on top of those digoxin labs might feel like pulling teeth, but trust me, it pays off. think of it as a tiny check‑in with your body’s own engine, making sure it runs smooth. i know the numbers can look scary, especially when you see that 2.0 ng/mL red flag, but remember that a lot of that comes down to kidney health and diet. if your eGFR is good and you’re keeping potassium up, you’re already doing half the work. also, i love the idea of setting a reminder in your phone or the clinic’s portal – that way you’re not relying on memory alone. keep the communication open with your doc, let them know about any new meds, and don’t be shy about asking why a level is being checked. you’ve got this, and the more you’re involved, the safer your heart will stay.
Ben Dover
November 6, 2025 AT 03:40 AMNeglecting monitoring is a reckless gamble.
Katherine Brown
November 9, 2025 AT 15:00 PMColleagues, I would like to emphasize that the integration of systematic digoxin level assessments within our standard care pathways is paramount for patient safety. The evidence underscores the necessity of aligning dosage adjustments with renal function trends and electrolyte balance. By adhering to a protocol that mandates level checks upon any modification of therapy, we mitigate the risk of inadvertent toxicity. I appreciate the collective commitment to uphold these best practices for the benefit of our patients.
Ben Durham
November 13, 2025 AT 02:20 AMAbsolutely, Katherine. Setting up a standing order for a digoxin level every six months in stable patients is a smart move, and we should flag any change in eGFR or potassium as a trigger for an earlier draw. I’ve found that a brief note in the chart, like “monitor digoxin q6‑12 mo – renal function stable,” keeps the team on the same page. Also, reminding patients to report visual changes or palpitations can catch problems before they become critical. Let’s keep the workflow simple and the communication clear.
Tony Stolfa
November 16, 2025 AT 13:40 PMListen up, people – if you think you can wing it with digoxin and skip the labs, you’re asking for trouble. This isn’t some optional supplement; it’s a potent drug that can kill you if you’re sloppy. Get your levels checked, adjust for kidney function, and stop acting like you’re above basic medical protocol.
Joy Dua
November 20, 2025 AT 01:00 AMIndeed the very act of ignoring serum digoxin concentrations becomes a philosophical affront to the sanctity of evidence based medicine the heart demands precision not guesswork each measurement is a stanza in the poem of patient safety illustrating the fragile balance between therapeutic benefit and lethal excess we must listen to the silent numbers they speak of renal clearance and electrolyte harmony lest we compose a tragic epic of arrhythmia
Holly Kress
November 23, 2025 AT 12:20 PMThanks for sharing these perspectives, everyone. It’s clear that diligent monitoring, clear communication, and patient education all play vital roles in safe digoxin use. Let’s continue to support each other in setting up reminders and checking labs promptly, especially when things change. Together we can keep our patients both safe and informed.