When your body turns on its own pancreas, life changes overnight. Type 1 diabetes isn’t just about high blood sugar-it’s the result of your immune system attacking the insulin-producing cells in your pancreas. This isn’t a lifestyle mistake. It’s not caused by eating too much sugar. It’s an autoimmune disease, and it starts long before you ever feel sick.
The Pancreas Under Attack
Your pancreas does two big jobs: it makes digestive enzymes and it makes insulin. In type 1 diabetes, only the insulin-making part gets destroyed. Special immune cells-called T-cells-mistake your beta cells for invaders. They swarm into the islets of Langerhans, the tiny clusters where insulin is made, and wipe them out. This process, called insulitis, can begin years before symptoms show up.By the time someone is diagnosed, they’ve usually lost more than 90% of their insulin-producing cells. Blood tests show C-peptide levels below 0.2 nmol/L-almost nothing. That’s why insulin injections aren’t optional. They’re survival.
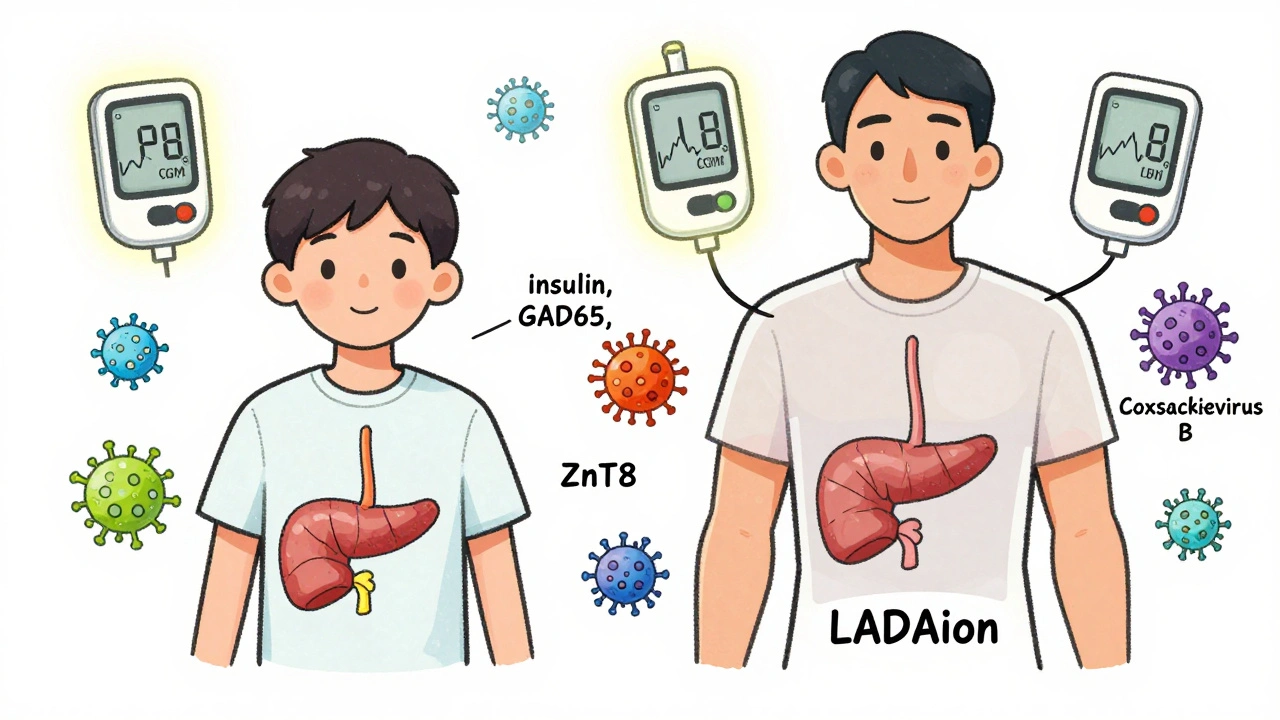
Autoantibodies are the fingerprints of this attack. The most common ones target insulin itself, GAD65, IA-2, and ZnT8. Finding two or more of these in a person’s blood, even before they’re diabetic, means they’re in Stage 1 of type 1 diabetes. That’s when researchers can step in-before the damage is total.
It’s Not Just One Disease
People think type 1 diabetes is the same for everyone. It’s not. Some kids crash into diagnosis in weeks. Others, especially adults, slowly lose insulin over years. That’s LADA-Latent Autoimmune Diabetes in Adults. Many are misdiagnosed as type 2 because they’re not overweight or young. They’re told to diet and exercise. They wait months before realizing insulin is their only real option.Genetics play a huge role. If you carry the HLA-DR3/DR4 genes, your risk jumps 20 to 30 times higher than average. But genes alone don’t cause it. Something triggers the immune system. Viruses, especially coxsackievirus B, show up in the blood of many newly diagnosed patients. Gut health matters too-studies show 67% of people with type 1 have fewer good gut bacteria that help calm inflammation.
And then there’s the rare twist: autoimmune pancreatitis. In about 1 in 300 cases, the immune system attacks both the insulin cells and the enzyme-producing parts of the pancreas. This isn’t common, but if someone with type 1 has unexplained belly pain, nausea, or weight loss, doctors need to check for it. Treatment? Steroids. But steroids raise blood sugar-so insulin doses have to be adjusted fast.
Managing the Daily Battle
There’s no cure yet. But management has changed dramatically. The old way-two shots a day, finger pricks four times a day-is outdated. Today’s standard is multiple daily injections (MDI) or an insulin pump, paired with continuous glucose monitoring (CGM).Devices like the Dexcom G7 or Abbott FreeStyle Libre don’t just track sugar-they predict drops and spikes. The DIAMOND trial showed people using CGM lowered their A1c by 0.4-0.6% and had 40-50% fewer low-blood-sugar events. That’s not just numbers. It’s fewer panic attacks at 3 a.m., fewer missed school days, fewer ER visits.
For those ready to go further, closed-loop systems-sometimes called artificial pancreases-do the heavy lifting. Tandem’s Control-IQ adjusts insulin automatically based on real-time glucose data. Users spend 71-74% of the day in the target range (70-180 mg/dL). Without it? Only 51-55%. That difference is life-changing.
When someone is first diagnosed, they start with about 0.5 units of insulin per kilogram of body weight each day. Half is long-acting (like insulin glargine U-300) to cover baseline needs. The other half is rapid-acting (like insulin aspart) for meals. Dosing isn’t set in stone. It’s adjusted daily based on food, activity, stress, illness.
Emerging Hope: Slowing the Disease
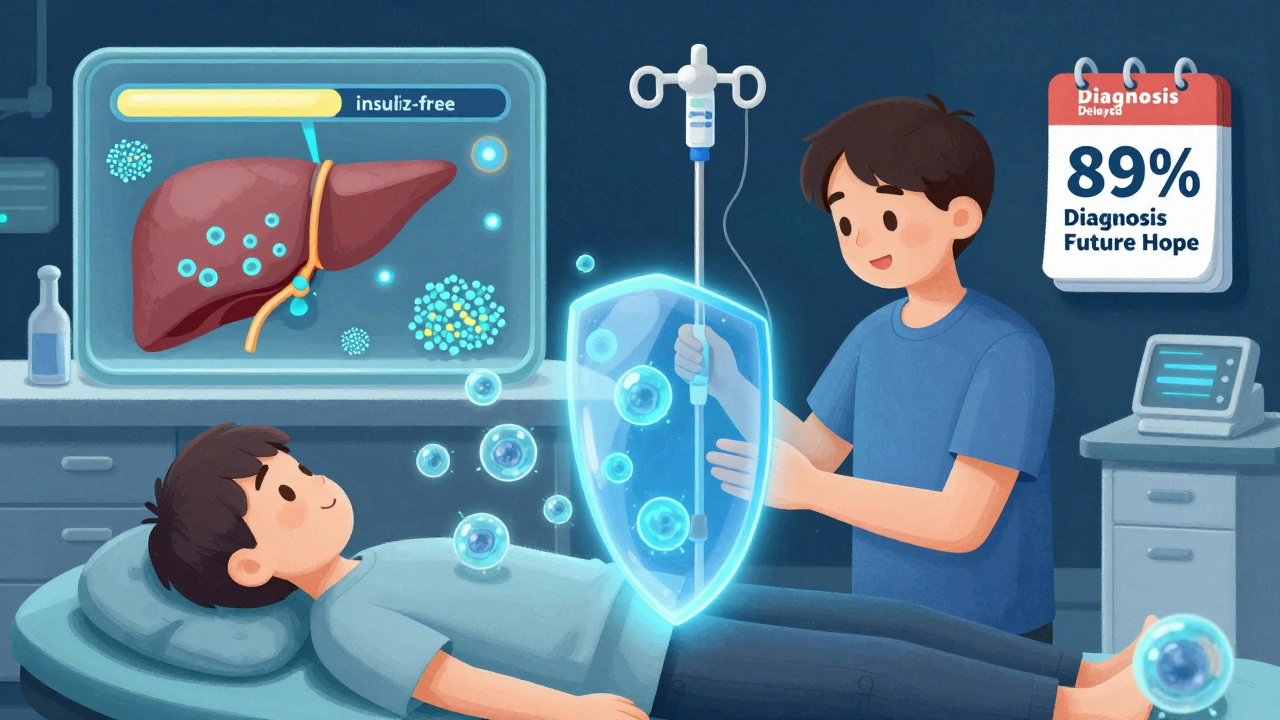
The biggest breakthrough in decades? Teplizumab (Tzield). Approved by the FDA in 2022, it’s the first drug that can delay type 1 diabetes onset. It doesn’t cure it. But in people with Stage 2-autoantibodies plus abnormal blood sugar but no symptoms-it pushes diagnosis back by nearly 2.5 years on average.How? It targets the immune cells that kill beta cells. It doesn’t shut down the whole immune system. Just the ones going rogue. It’s given as a 14-day IV infusion. Not for everyone. Only those with confirmed autoantibodies and early signs of glucose trouble. But for families with a child at high genetic risk, it’s a game-changer.
Other drugs are in the pipeline. Verapamil, a blood pressure medication, showed in a 2022 trial that it preserved 30% more insulin production over a year. Abatacept, used for rheumatoid arthritis, cut C-peptide decline by 59% in new-onset patients. And then there’s Vertex’s VX-880-stem cell-derived islets transplanted into the liver. In a 2023 trial, 89% of 12 participants became insulin-free after 90 days.
These aren’t fantasy treatments. They’re real. They’re being tested right now. The NIH’s TrialNet is running 15 active studies, testing everything from oral insulin to gut microbiome transplants.
What About Insulin Costs?
Even with all the advances, insulin is still a daily burden. In the U.S., the average person with type 1 spends $9,600 a year just on insulin. That’s 33% of their total healthcare costs. Newer analogs like insulin glulisine or aspart are more precise-but three to five times pricier than human insulin from the 1980s.Some people ration insulin. That’s deadly. The FDA has approved lower-cost insulin options, and some states now cap copays at $35 a month. But access still varies wildly. Globally, the insulin market hit $27.3 billion in 2022. Yet millions still can’t get it.
Looking Ahead
The future of type 1 diabetes isn’t just about better insulin. It’s about stopping the attack before it starts. Combining immunotherapy with drugs that protect surviving beta cells is the new frontier. The 2024 ADA/EASD guidelines call this the “next generation” of care.For now, the goal is simple: keep blood sugar in range, avoid complications, and stay alive until the next breakthrough. With CGM, automated insulin delivery, and emerging therapies, people with type 1 are living longer, healthier lives than ever before.
It’s not a cure. But it’s progress. And for a disease that was once a death sentence, that’s everything.
Is type 1 diabetes the same as autoimmune pancreatitis?
No. Type 1 diabetes attacks only the insulin-producing beta cells in the pancreas. Autoimmune pancreatitis attacks the enzyme-producing cells, causing digestive problems. They’re separate conditions, but they can rarely happen together-about 1 in 300 people with type 1 also develop autoimmune pancreatitis. When they do, treatment requires both insulin and steroids, with close monitoring of blood sugar.
Can you reverse type 1 diabetes?
Not yet. But some treatments can slow or delay it. Teplizumab can delay diagnosis by over two years in high-risk people. Stem cell transplants have restored insulin production in early trials. Some patients with recent-onset type 1 have temporarily reduced insulin needs using drugs like verapamil. But no one has fully reversed the disease and stopped insulin forever.
Why do some adults get misdiagnosed with type 2 diabetes?
Because type 1 in adults (LADA) looks like type 2. They’re often older, not obese, and don’t have obvious symptoms at first. Doctors assume insulin resistance. But if they test for autoantibodies and C-peptide, they’ll find the immune system is destroying beta cells. Around 12% of adults with type 1 are misdiagnosed, leading to delayed insulin and dangerous complications.
What’s the role of C-peptide in diagnosis?
C-peptide is a byproduct of insulin production. If your body is still making insulin, C-peptide is present. In type 1 diabetes, levels drop below 0.2 nmol/L at diagnosis-proof the beta cells are gone. In type 2, levels are usually above 0.6 nmol/L because the body still makes insulin, just can’t use it well. Testing C-peptide helps tell the two apart.
How does teplizumab work?
Teplizumab targets a specific protein on immune T-cells that attack beta cells. By binding to these cells, it temporarily reduces their activity, slowing the destruction of insulin-producing cells. It’s given as a 14-day IV infusion and only works for people in Stage 2-those with autoantibodies and abnormal blood sugar but no symptoms yet. It doesn’t cure diabetes, but it delays diagnosis by an average of 29.8 months.
Are there any new insulin-free treatments on the horizon?
Yes. Vertex’s VX-880 stem cell therapy has restored insulin production in early trials, with 89% of participants becoming insulin-free after 90 days. Other approaches include oral insulin vaccines, gut microbiome therapies, and drugs like verapamil that protect remaining beta cells. These aren’t widely available yet, but they’re in active clinical trials and represent the most promising path toward insulin independence.
Can diet or fasting cure type 1 diabetes?
No. While diet affects blood sugar levels, it cannot stop the autoimmune attack or restore destroyed beta cells. Some people report feeling better on low-carb diets, but that’s because they’re reducing insulin demand-not reversing the disease. Fasting or extreme diets can be dangerous and increase the risk of ketoacidosis. Medical nutrition therapy helps manage blood sugar, but it doesn’t replace insulin.
Why is time-in-range more important than A1c?
A1c gives an average over three months, but it hides dangerous swings. Someone could have an A1c of 7% but spend half their day below 70 mg/dL and half above 200 mg/dL. Time-in-range (70-180 mg/dL) shows how often glucose stays in the safe zone. Studies show people spending over 70% of the day in range have far fewer complications. CGM and automated insulin systems make tracking this possible-and it’s now a key goal in modern diabetes care.





Suzanne Johnston
December 10, 2025 AT 16:59 PMIt's wild how we treat autoimmune diseases like they're personal failures. Type 1 isn't a lack of discipline-it's biology turning against itself. The fact that we've spent decades blaming diet and lifestyle while real science pointed to immune dysfunction is a moral failure of medicine.
And yet here we are, with teplizumab finally offering a real path to delay, not just manage. This isn't just medical progress-it's validation for every kid who was told to 'just eat less sugar.'
People don't realize how much emotional labor goes into just surviving this. Not just the injections, but the constant fear, the isolation, the guilt from strangers who think you 'brought this on yourself.'
We need to stop treating diabetes as a personal responsibility and start treating it like the systemic failure it is-funding research, lowering insulin costs, and ending the stigma.
Maybe one day, we'll look back at this era the way we look at tuberculosis in the 1800s: a disease we blamed on weak willpower, while the real solution was right in front of us.
Andrea Petrov
December 10, 2025 AT 17:31 PMThey say it's autoimmune but nobody talks about the vaccines. Did you know the coxsackievirus B strain was in the rotavirus trials? And the gut microbiome disruption? That's from glyphosate in our food supply. Big Pharma doesn't want you to know this-they profit off insulin forever.
They're pushing teplizumab like it's a miracle, but it's just a Band-Aid. The real cure? Remove the toxins. Eat organic. Heal your gut. But they won't tell you that because it doesn't involve a $10,000 drug.
I know a woman who reversed her type 1 with a 30-day water fast and probiotics. They called her a fraud. But her C-peptide went from 0.1 to 0.8. The system hates success that doesn't come with a price tag.
Graham Abbas
December 12, 2025 AT 10:01 AMReading this felt like someone finally wrote the book I've been trying to explain to my friends for years.
I used to think diabetes was just about numbers-glucose, A1c, carbs. But it's not. It's about living in a body that's been hijacked. The fear of a low at 2 a.m., the shame of needing insulin in public, the loneliness of being the only one who gets it.
And yet... there's beauty here too. The community. The innovation. The way we've turned survival into science. CGMs aren't just devices-they're lifelines. Closed-loop systems aren't tech-they're freedom.
I wish more people saw this as a human story, not a medical case study.
Chris Marel
December 14, 2025 AT 02:16 AMI'm from Nigeria, and here insulin is a luxury. Some of us use expired vials just to survive. I read this and cried-not because I didn't know, but because I didn't think anyone else cared.
The cost numbers? They're not stats. They're death sentences. I have a cousin who lost a leg because she rationed insulin. No one talks about that.
I hope your breakthroughs reach places like mine too. Science shouldn't have borders.
Haley P Law
December 16, 2025 AT 01:35 AMOMG I JUST FOUND OUT MY COUSIN HAS TYPE 1 AND I THOUGHT IT WAS JUST FROM EATING TOO MUCH CAKE 😭 I FEEL SO BAD
Also the Dexcom G7 is so cute?? Like a little sci-fi bracelet?? I want one 😍
Andrea DeWinter
December 17, 2025 AT 11:19 AMTeplizumab is huge but it's only for Stage 2. What about the people who don't get tested until they're in DKA? We need universal autoantibody screening for kids with family history. It's cheap. It's simple. Why aren't we doing it?
And for anyone saying diet can cure this-stop. You're not helping. You're hurting. This isn't a cleanse. It's a lifelong battle.
Also if you're using insulin from the 80s because you can't afford the new stuff-you're not being brave. You're being failed by a broken system.
Let's stop romanticizing survival and start demanding justice.
Steve Sullivan
December 17, 2025 AT 12:58 PMSo like... if your body attacks its own pancreas, does that mean you're basically fighting yourself? Like a civil war inside your cells? Wild.
I got my CGM last year and it changed my life. No more guessing. No more panic. Just data. It's like having a tiny robot buddy watching your blood sugar 24/7. 💪🤖
Also verapamil? That's a blood pressure pill?? So we're repurposing old meds to save lives? That's the real MVP move right there.
And yeah insulin costs are insane. I paid $400 for one vial last month. I'm not even mad. I'm just tired.
George Taylor
December 19, 2025 AT 02:02 AMLet's be honest: this whole 'progress' narrative is just corporate PR.
Teplizumab? A 2.5-year delay? That's not a cure-it's a delay tactic so they can keep selling insulin for another 30 months.
Stem cell transplants? 89% insulin-free? But only 12 people. And the trial was funded by Vertex, who will charge $1M per treatment. This isn't medicine-it's capitalism with a lab coat.
And don't get me started on CGMs. They're expensive, fragile, and require constant calibration. Who's really benefiting? The companies selling them.
Real progress would be making insulin free. But that's not profitable.
ian septian
December 20, 2025 AT 12:43 PMInsulin isn't optional. It's survival.
Carina M
December 22, 2025 AT 09:53 AMIt is both lamentable and profoundly disconcerting that the public discourse surrounding Type 1 Diabetes remains so egregiously misinformed, despite the overwhelming volume of peer-reviewed literature elucidating its autoimmune etiology. One is compelled to note, with considerable consternation, that the persistent conflation of this condition with lifestyle-related metabolic dysfunction constitutes not merely an epistemic failure, but a moral one.
Furthermore, the commodification of therapeutic interventions-such as teplizumab-within a profit-driven healthcare architecture, while simultaneously denying access to life-sustaining insulin, represents a systemic pathology that transcends medical science and enters the realm of bioethical abdication.
One must, therefore, implore the medical establishment, policymakers, and the general public to transcend the reductive narratives perpetuated by social media influencers and pharmaceutical marketing departments, and instead engage with the scientific consensus with the gravity it demands.
There is no 'cure' via dietary modification. There is no 'detox.' There is only biology, and the moral imperative to treat it with dignity.