When your heart doesn’t get enough oxygen, trimetazidine, a metabolic modulator used to treat angina by shifting heart energy use from fat to glucose and ranolazine, a late sodium current inhibitor that reduces heart muscle strain without affecting heart rate or blood pressure are two options doctors may consider. Neither is a first-line treatment like beta-blockers or calcium channel blockers, but they’re often added when those aren’t enough—or when side effects make them hard to tolerate. Both aim to reduce chest pain by helping the heart work more efficiently, but they do it in completely different ways.
Trimetazidine is common in Europe and parts of Asia, where it’s been used for decades. It doesn’t lower blood pressure or slow your heart rate, which makes it useful for people who can’t take those kinds of drugs. Instead, it changes how the heart uses fuel, pushing it to burn glucose instead of fatty acids—a cleaner, oxygen-sparing process. Ranolazine, approved by the FDA in 2006, works by blocking a specific ion channel in heart cells that gets overactive during ischemia. This reduces the heart’s workload without changing heart rhythm or blood pressure. Studies show both drugs reduce angina episodes and improve exercise tolerance, but ranolazine has more robust data from U.S.-based trials, while trimetazidine’s strongest evidence comes from European studies.
Side effects differ too. Trimetazidine can cause dizziness, stomach upset, and, rarely, movement disorders like parkinsonism—especially in older adults. Ranolazine may lead to nausea, constipation, or dizziness, and it can affect heart rhythm in people with existing QT prolongation. It also interacts with common drugs like statins and antifungals, so dosing needs care. Neither drug is for everyone, but for someone with stable angina who’s already on beta-blockers and still having symptoms, one of these might be the missing piece.
Cost and availability matter. Trimetazidine is often cheaper and available as a generic in many countries. Ranolazine is still mostly brand-name in the U.S., though generics are starting to appear. Insurance coverage varies widely, so out-of-pocket cost can swing the decision. If you’re on a tight budget and your doctor thinks either could help, asking about generic trimetazidine first makes sense.
What’s clear is that neither drug fixes the root cause—narrowed arteries. They’re symptom managers, not cures. But for people who can’t have stents or bypass surgery, or who still feel chest tightness despite optimal treatment, these two drugs offer real relief. The choice between them often comes down to what your body tolerates, what your doctor knows works in your region, and whether cost or side effects tip the scale.
Below, you’ll find real-world comparisons, patient experiences, and clinical insights that show exactly how these two drugs stack up—and which one might be right for your situation.
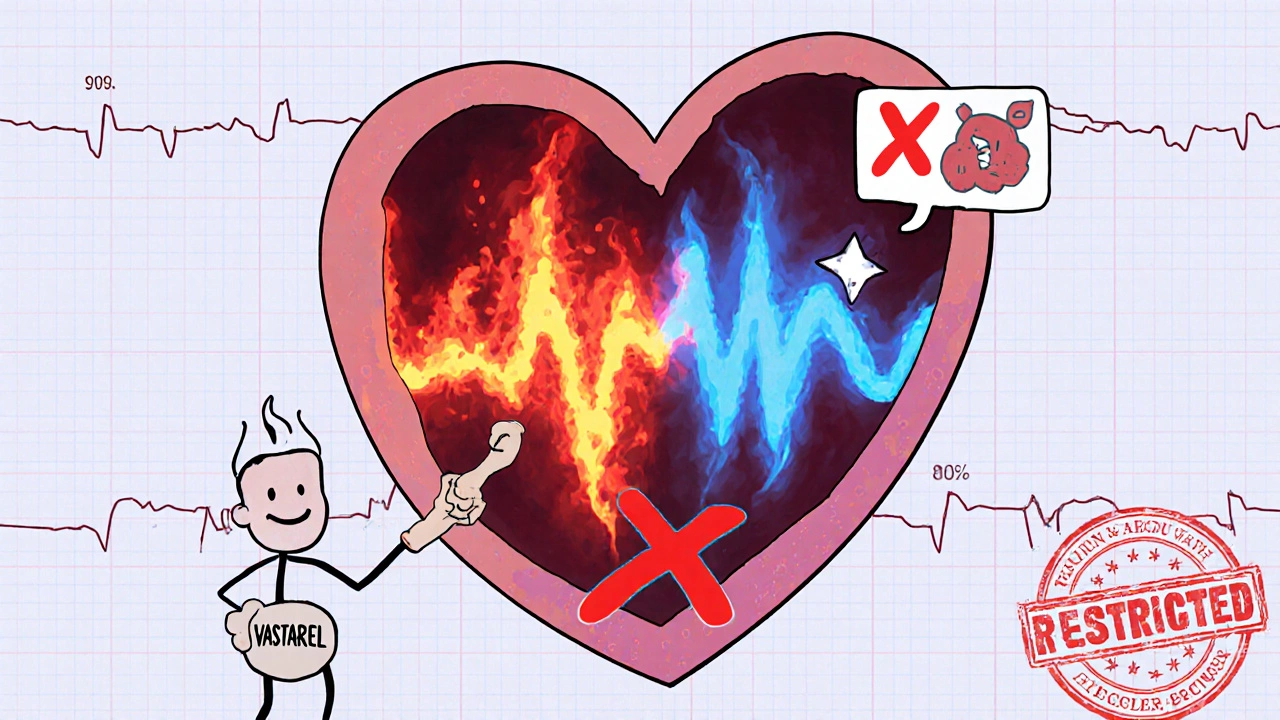
Compare Vastarel (trimetazidine) with safer, better-studied alternatives like ranolazine, beta-blockers, and nitroglycerin for managing angina. Learn what doctors recommend in 2025 and which options carry fewer risks.
read more