What Is Peripheral Neuropathy?
Peripheral neuropathy isn’t one disease-it’s a group of conditions caused by damage to the nerves outside your brain and spinal cord. These nerves connect your limbs, skin, muscles, and organs to your central nervous system. When they get damaged, you might feel tingling, burning, or numbness, usually starting in your feet or hands. Over 20 million Americans live with this condition, and for many, it’s not just uncomfortable-it’s disabling.
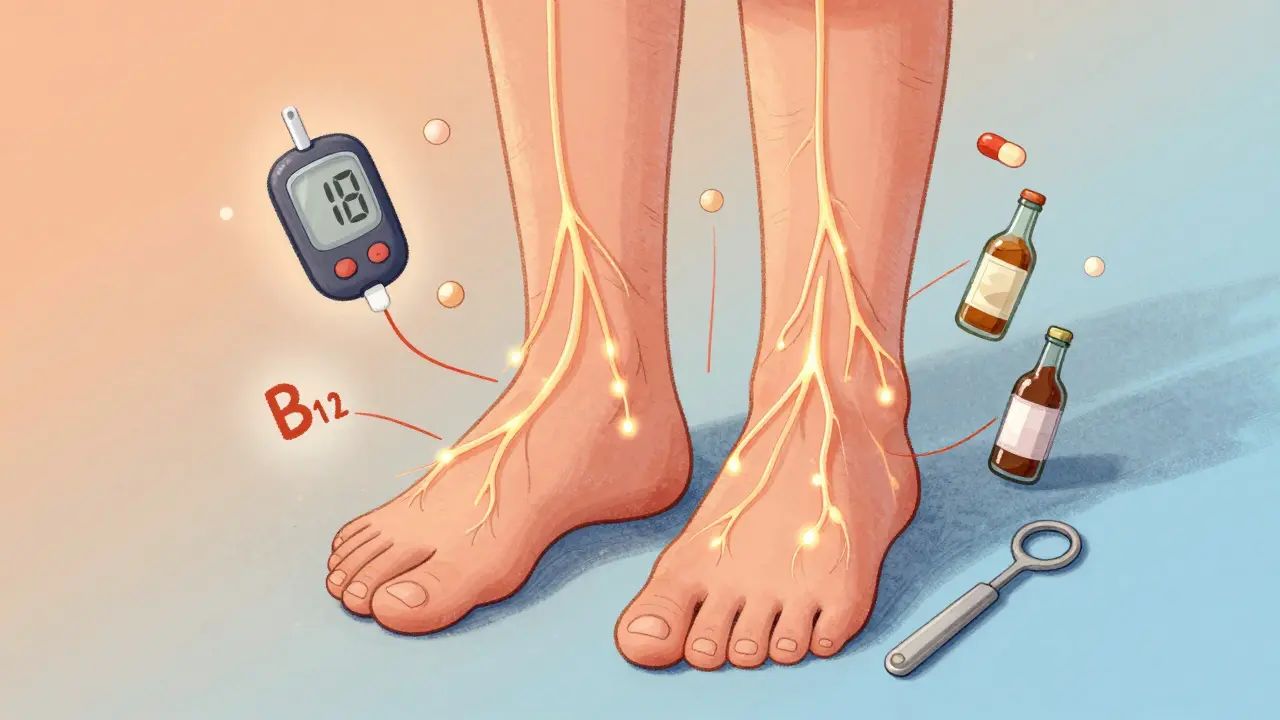
The most common cause? Diabetes. About half of all people with diabetes develop some form of nerve damage over time. But it’s not just diabetes. Chemotherapy, vitamin B12 deficiency, alcohol abuse, autoimmune disorders, and even certain infections can trigger it. In about 20% of cases, doctors can’t find a clear cause at all-these are called idiopathic neuropathies.
How Do You Know If It’s Neuropathy?
People often ignore early symptoms, thinking it’s just aging or tired feet. But there are clear signs that point to nerve damage:
- Sharp, burning, or electric-like pain in feet or hands
- Numbness that feels like wearing invisible gloves or socks
- Tingling or crawling sensations, especially at night
- Loss of balance or frequent tripping
- Muscle weakness in hands or feet
- Extreme sensitivity to light touch-even sheets feeling painful
Doctors use simple tests to confirm it. A 10-gram monofilament pressed against your foot checks for loss of sensation. A tuning fork tests vibration sense. Nerve conduction studies measure how fast signals travel through your nerves-slower than 40 meters per second usually means damage. These aren’t fancy lab tests; they’re routine, quick, and reliable.
Why Does It Hurt So Much?
Unlike regular pain from a cut or sprain, neuropathic pain doesn’t come from tissue injury. It’s the nerves themselves sending wrong signals. Think of it like a frayed wire in your home-instead of turning on the light, it sparks and shocks you randomly. That’s why over-the-counter painkillers like ibuprofen or acetaminophen barely help. They’re designed for inflammation or tissue pain, not nerve misfires.
The brain starts misinterpreting harmless sensations as pain. Light pressure from a sock can feel like a knife. A cool breeze might burn. This isn’t in your head-it’s in your nerves. And the longer it goes untreated, the more the nervous system rewires itself to amplify the pain. That’s why early intervention matters.
Diabetes and Neuropathy: The Biggest Link
If you have diabetes, your risk of neuropathy jumps dramatically. About 50% of the 34 million Americans with diabetes develop nerve damage. But here’s the good news: keeping your HbA1c below 7% cuts your risk of progression by 60%, according to the landmark Diabetes Control and Complications Trial.
High blood sugar slowly damages the small blood vessels that feed your nerves. Without enough oxygen and nutrients, the nerves start to die. That’s why foot ulcers and infections are so common-your nerves can’t tell you when you’ve stepped on something sharp, and your circulation can’t heal the wound fast enough.
Managing blood sugar isn’t just about avoiding complications-it’s the single most effective way to stop neuropathy from getting worse. That means daily monitoring, consistent meals, and working with your doctor to adjust medications like SGLT2 inhibitors, which new research shows may reduce neuropathy risk by 30%.

Treatment Options That Actually Work
There’s no magic cure, but several treatments have proven results:
- Pregabalin (Lyrica): Reduces pain by 50% in about 37% of users. Side effects? Dizziness and drowsiness, especially at first.
- Duloxetine (Cymbalta): Works for 35% of people. Helps with both pain and depression, which often come together.
- Amitriptyline: An old antidepressant that still works well-41% of patients get 50% pain relief. But it causes dry mouth in 75% and makes you sleepy.
These aren’t one-size-fits-all. What works for one person might make another feel worse. That’s why doctors start low and go slow. Many people quit because of side effects-nearly two-thirds stop within three months.
Non-drug options can be just as powerful. Scrambler therapy, which uses electrical signals to “reset” pain pathways, helped 85% of patients in Mayo Clinic trials get at least 50% pain relief after 10 sessions. Spinal cord stimulation works for tough cases, with 65% of patients reporting major improvement.
Physical Therapy and Daily Habits That Help
Medications don’t fix balance or strength. That’s where physical therapy comes in. A 12-week program focused on balance and leg strength improves your “timed up and go” score by 25%. That means fewer falls, more confidence walking, and less fear.
Simple daily habits make a huge difference:
- Check your feet twice a day for cuts, blisters, or redness-use a mirror if you can’t see the bottom of your feet.
- Wear custom orthotics or therapeutic shoes. People who do report 82% satisfaction.
- Take off your shoes and socks before bed. Cold feet can worsen pain. Warm socks help.
- Stretch your calves and feet every morning. Tight muscles add pressure to already sensitive nerves.
One patient on Reddit said she stopped falling after starting daily heel raises and toe curls. Another said he finally slept through the night after switching to cotton socks and keeping his bedroom cool.
What Doesn’t Work-and What to Avoid
Many people try remedies that sound logical but don’t help:
- Alcohol: It’s a nerve poison. Even moderate drinking can make neuropathy worse.
- Opioids: They work for about 30% of people, but addiction rates hit 15% with long-term use. Experts strongly discourage them.
- Over-the-counter painkillers: Ibuprofen or aspirin might reduce inflammation, but they cut neuropathic pain by only 10-15%. Not worth the stomach risk.
- Unproven supplements: Some claim miracle cures with alpha-lipoic acid or B vitamins. While B12 helps if you’re deficient, taking extra without a diagnosis won’t help-and can mask other problems.
Don’t waste time or money on gimmicks. Stick to science-backed approaches.

When to Seek Help-and What to Expect
Too many people wait over a year before seeing a doctor. The average time from first symptom to diagnosis? 18 months. That’s too long. Early treatment improves outcomes by 40%.
When you go in, expect:
- A full medical history-what you eat, what meds you take, your alcohol use, your diabetes control
- Physical exams with tuning forks and monofilaments
- Optional nerve conduction studies (costs $500-$1,500)
- Blood tests for B12, thyroid, glucose, and autoimmune markers
If your doctor doesn’t test for the most common causes, ask. Don’t accept “it’s just aging.”
What’s Next? New Treatments on the Horizon
Research is moving fast. In 2020, the FDA approved Qutenza-a capsaicin patch applied once every three months. It numbs the nerve endings in your skin and gives lasting relief. In clinical trials, 31% of users had significant pain reduction.
The Foundation for Peripheral Neuropathy launched the Neuropathy Genomics Project in 2023, aiming to identify genetic causes for over 50 types of neuropathy by 2026. That could lead to personalized treatments.
Wearable nerve stimulators are in development and expected to hit the market in 2024. Early tests show they can reduce pain by 40% with daily use. And gene therapies for inherited forms like Charcot-Marie-Tooth disease are showing promise in early trials.
Living With It: Real Life, Real Adjustments
People with neuropathy aren’t just managing pain-they’re rebuilding their lives. Many quit driving because dizziness from meds makes it unsafe. Others give up their jobs. One in four end up retiring early.
But many find ways to adapt:
- Using a cane or walker for balance
- Installing grab bars in the bathroom
- Switching to slip-on shoes with no laces
- Joining support groups-Reddit’s r/neuropathy has over 12,000 members sharing tips
One man in Colorado started walking his dog every morning in a quiet park. He said the routine gave him structure. The fresh air helped his mood. The movement kept his legs strong. He didn’t get cured-but he got his life back.
Can peripheral neuropathy be reversed?
In some cases, yes-if the cause is treatable. If it’s due to vitamin B12 deficiency, correcting the deficiency can reverse nerve damage over weeks to months. If it’s caused by chemotherapy or alcohol, stopping the trigger can prevent further damage and sometimes allow nerves to heal slowly. But if the damage is long-standing, especially from uncontrolled diabetes, full reversal is rare. The goal shifts to stopping progression and managing symptoms.
Is neuropathy the same as carpal tunnel?
Carpal tunnel is a type of mononeuropathy-it’s damage to one specific nerve, the median nerve, in your wrist. Peripheral neuropathy usually refers to polyneuropathy, which affects many nerves throughout the body, often symmetrically in the hands and feet. So carpal tunnel is one kind of nerve damage, but not the same as the widespread nerve damage seen in diabetic or idiopathic neuropathy.
Do I need to stop working if I have neuropathy?
Not necessarily. Many people continue working with adjustments. If your job requires standing or fine motor skills, talk to your employer about ergonomic changes-sitting stools, cushioned mats, voice-to-text software. The Americans with Disabilities Act protects you. Only about 25% of people with neuropathy end up retiring early, usually because of severe pain or balance issues that make safety a concern.
Can diet help with neuropathy pain?
Yes, but only if you’re deficient in certain nutrients. Vitamin B12, B6, and folate are critical for nerve health. Eating more eggs, lean meats, leafy greens, and fortified cereals helps. For people with diabetes, a low-sugar, high-fiber diet improves blood sugar control-which directly slows nerve damage. No special “neuropathy diet” exists, but a balanced, whole-foods approach supports overall nerve function.
Why do symptoms get worse at night?
At night, distractions fade, so your brain focuses more on pain signals. Also, your body temperature drops slightly, which can make damaged nerves more sensitive. Lying still for long periods can also increase pressure on nerves. Keeping your room cool, wearing soft socks, and doing light stretching before bed can help reduce nighttime flare-ups.






June Richards
February 2, 2026 AT 06:47 AMUgh I hate how doctors just hand you Lyrica like it's candy. I took it for 3 weeks and felt like a zombie. My feet still burned but now I couldn't remember where I put my keys. 😴💊
Jaden Green
February 3, 2026 AT 14:25 PMIt's fascinating how modern medicine continues to pathologize normal aging. The notion that tingling in the extremities requires pharmaceutical intervention is a product of corporate-driven healthcare. The body is not a machine to be fixed with SSRIs and anticonvulsants-it's an organic system that responds to holistic recalibration. Have you considered the metaphysical implications of neuropathic pain as a somatic manifestation of disconnection from ancestral rhythms? I've read extensively on the topic.
Lu Gao
February 4, 2026 AT 11:38 AMI love how this article mentions Qutenza but doesn't say it costs $1,000 per application 😅 Also, 'cotton socks' are not a treatment, they're a basic hygiene practice. Can we please stop pretending lifestyle tweaks are cures? 🙃
Angel Fitzpatrick
February 5, 2026 AT 06:59 AMLet me guess-Big Pharma paid the Mayo Clinic to run those scrambler therapy trials. They don’t want you to know that the FDA banned capsaicin patches in ’18 for neurotoxicity. Qutenza? It’s just a rebranded rat poison with a patent. And why no mention of 5G radiation disrupting peripheral nerve signaling? I’ve got 17 years of medical records showing a spike after my smart meter installation. The government won’t admit it, but your nerves are being hacked.
Melissa Melville
February 7, 2026 AT 06:07 AMSo you're telling me my grandma's advice to 'put on socks and drink milk' was actually kinda right? 🤔
Ed Di Cristofaro
February 8, 2026 AT 21:19 PMAlcohol is a nerve poison? Duh. I knew that since I was 16. But you wanna know what’s really toxic? Lying to people and telling them their pain is 'all in their head' because they're not diabetic. I’ve got neuropathy from chemo and zero sugar issues. Stop acting like diabetes is the only valid reason to hurt.
Lilliana Lowe
February 9, 2026 AT 22:40 PMThe article inaccurately conflates mononeuropathies with polyneuropathies in the carpal tunnel section. Furthermore, the citation of the Diabetes Control and Complications Trial is outdated; the follow-up study DCCT/EDIC demonstrated a 57% reduction in progression over 18 years, not 60%. Additionally, the claim that '82% satisfaction' with orthotics is misleading-it's based on a 2018 non-blinded survey of 87 patients, not a RCT. I'm surprised such sloppy science made it past peer review.
Lisa Rodriguez
February 11, 2026 AT 17:52 PMI’ve had this for 12 years. Took me 8 years to get diagnosed. I didn’t know it wasn’t normal to cry because my socks felt like sandpaper. I’m not here to argue about studies or blame Big Pharma. I just want to say: if you’re reading this and you’re scared or alone-please know you’re not. I started walking my dog every morning too. The world doesn’t have to end just because your feet hurt. Small things matter. Warm socks. A quiet room. A friend who listens. That’s the real treatment. And yeah, I still take Lyrica. And I’m not ashamed.