When you have hypertension, a chronic condition where the force of blood against artery walls is too high. Also known as high blood pressure, it doesn’t always cause symptoms—but it quietly increases your risk of heart attack, stroke, and kidney damage. That’s why hypertension safety isn’t just about taking a pill. It’s about understanding how your meds work with your body, what to watch for, and how to avoid mistakes that could put you in danger.
Many people with hypertension take blood pressure meds, drugs designed to lower arterial pressure and reduce strain on the heart and vessels. Also known as antihypertensives, these include ACE inhibitors, beta-blockers, diuretics, and calcium channel blockers. But here’s the catch: some of these drugs interact with common over-the-counter painkillers, cold medicines, or even herbal supplements. For example, NSAIDs like ibuprofen can undo the effects of your blood pressure medication. And if you’re on a diuretic, skipping your potassium-rich foods might lead to dangerous electrolyte imbalances. These aren’t hypothetical risks—they’re documented in clinical studies and show up in pharmacy error reports every day.
medication side effects, unintended reactions that can range from mild dizziness to life-threatening arrhythmias. Also known as drug reactions, they’re often overlooked because they develop slowly. A slow heartbeat from a beta-blocker might seem normal until you start feeling faint climbing stairs. Swelling from a calcium channel blocker might look like aging—but it’s your body telling you the dose is too high. And if you’re taking more than one drug, the risk multiplies. That’s why monitoring isn’t optional. It’s part of hypertension safety. Regular check-ins with your doctor, tracking your blood pressure at home, and knowing which symptoms to report aren’t extra steps—they’re your first line of defense.
And it’s not just about the pills. Your lifestyle choices—salt intake, alcohol, sleep quality, stress levels—directly affect how well your treatment works. A poor night’s sleep can spike your blood pressure. Too much sodium can make your meds less effective. Even sitting too long can reduce circulation and make your heart work harder. Hypertension safety means connecting the dots between what you take, what you eat, and how you live.
What you’ll find below is a collection of real-world guides that cut through the noise. You’ll see how certain drugs can trigger rapid heartbeat, how acid-reducing meds change how your body absorbs other pills, and why monitoring levels like digoxin matters even if you’re not on it. There’s advice on avoiding dangerous interactions, spotting hidden risks, and making smart choices when your blood pressure meds don’t feel right. These aren’t theory pieces—they’re practical, tested insights from people who’ve been there. Whether you’re just starting out or have been managing hypertension for years, this isn’t about scare tactics. It’s about giving you the tools to stay safe, stay informed, and take real control.
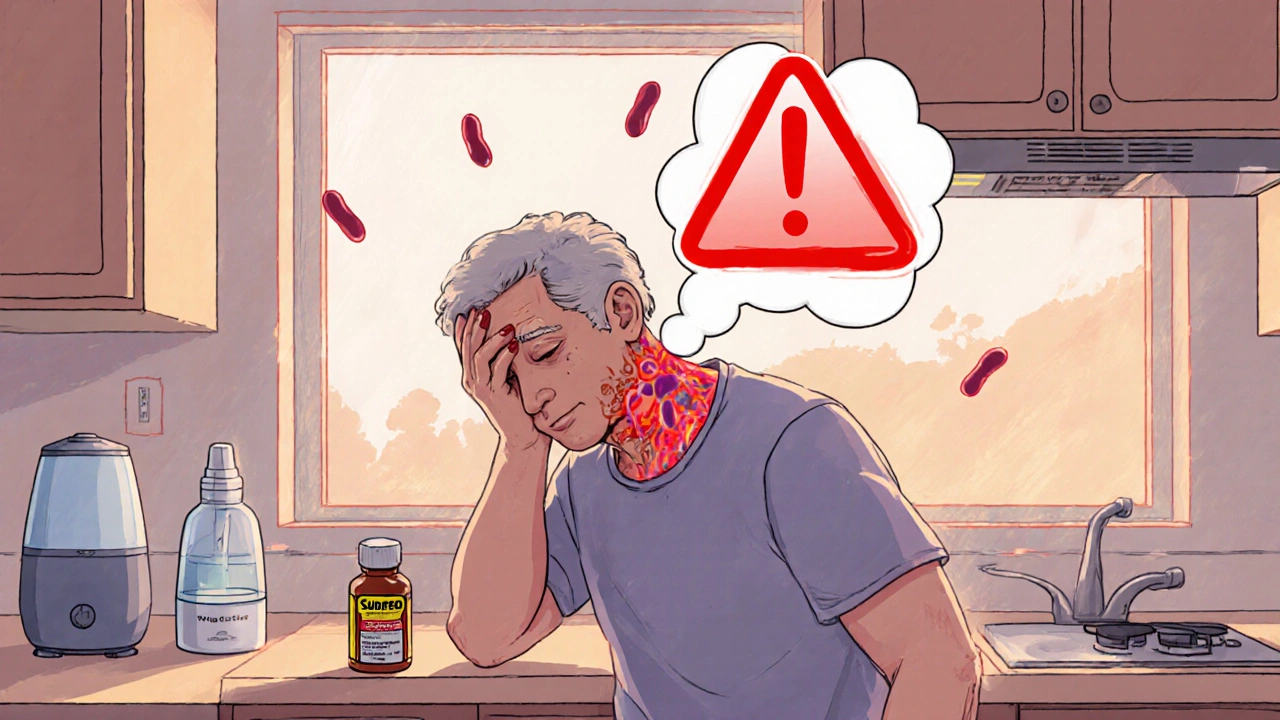
Nasal decongestants can dangerously raise blood pressure when taken with hypertension meds. Learn which ingredients to avoid, safe alternatives, and how to read labels to protect your heart.
read more