Decongestant Safety Checker
Is This Combination Safe?
Check if your blood pressure medication and decongestant are safe to use together. Based on guidelines from the American Heart Association and FDA.
If you’re on blood pressure medication and get a stuffy nose, you might reach for a decongestant without thinking twice. But here’s the truth: that little bottle of Sudafed or a cold tablet from the pharmacy could be quietly raising your blood pressure - and putting your heart at risk.
Why Decongestants Are Dangerous with High Blood Pressure
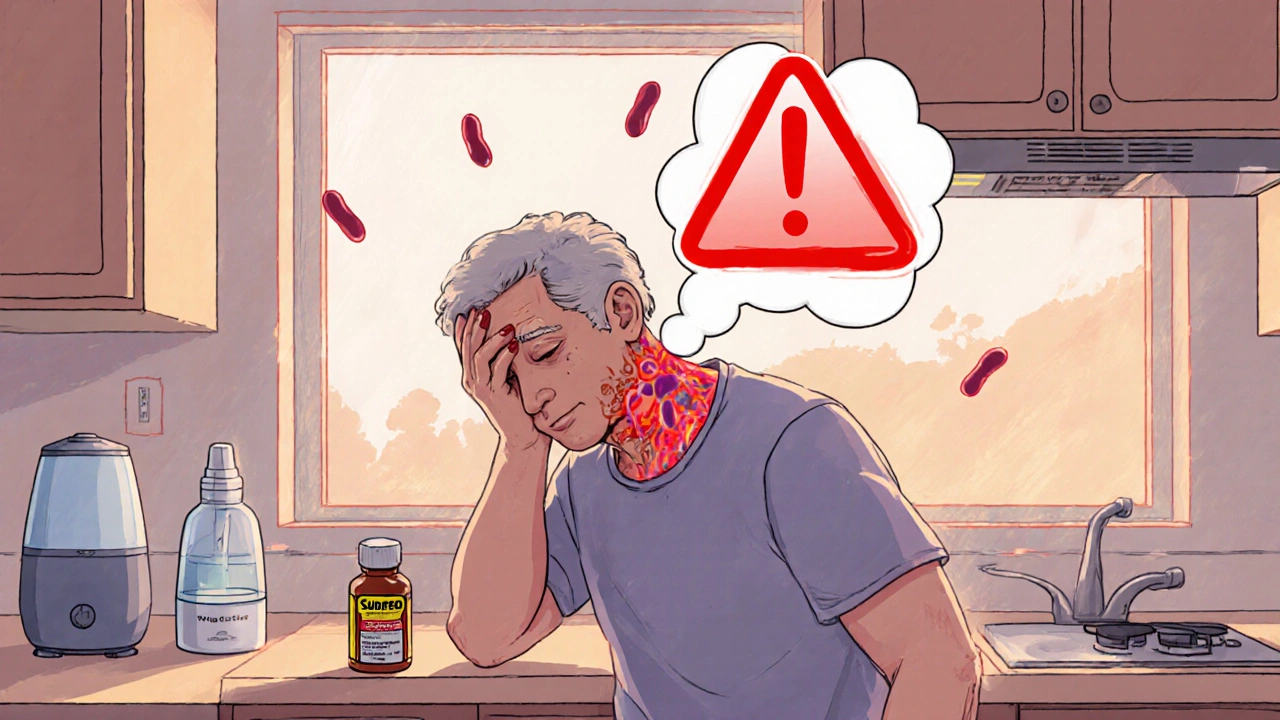
Nasal decongestants like pseudoephedrine and phenylephrine work by shrinking swollen blood vessels in your nose. That sounds helpful, right? But here’s the catch: they don’t just shrink vessels in your nose. They tighten blood vessels everywhere - including those around your heart and brain. This vasoconstriction forces your heart to pump harder, which can spike your blood pressure. Even if your hypertension is usually well-controlled, a single dose of pseudoephedrine can push systolic pressure up by 5 to 10 mmHg. That might not sound like much, but for someone with heart disease or kidney issues, it’s enough to trigger chest pain, dizziness, or even a stroke. The American Heart Association says this isn’t just a theory. Between 2020 and 2024, over 22% of emergency visits for uncontrolled high blood pressure in adults over 50 were linked to over-the-counter decongestants. Many patients didn’t even realize they were taking one. These ingredients hide in multi-symptom cold and flu products - often labeled as "sinus relief," "allergy and cold," or "nighttime formula."Which Decongestants to Avoid Completely
Not all decongestants are the same, but the most common ones are all risky if you’re on blood pressure meds:- Pseudoephedrine - Found in Sudafed, Claritin-D, Zyrtec-D, and many generic cold tablets. This is the most potent and most dangerous for people with hypertension.
- Phenylephrine - Now the most common decongestant in store brands, after pseudoephedrine was restricted behind pharmacy counters. But studies show it still raises blood pressure, especially in higher doses or with repeated use.
- Oxymetazoline - Found in nasal sprays like Afrin. Many people think topical means safe. It doesn’t. Even a few days of use can lead to systemic absorption and dangerous spikes in blood pressure.
- Ephedrine - Rare in the U.S. now, but still found in some herbal supplements and older formulas. Extremely dangerous - linked to heart attacks and strokes.
What Happens When Decongestants Mix With Your Blood Pressure Pills
Your blood pressure medication doesn’t just lower pressure - it keeps your heart rhythm steady, reduces strain on your arteries, and protects your kidneys. Decongestants undo all that. Take metoprolol, for example. It slows your heart rate and reduces how hard your heart pumps. Pseudoephedrine does the opposite: it speeds up your heart and makes it pump harder. When taken together, your body gets conflicting signals. The result? Unpredictable blood pressure swings, palpitations, or even irregular heartbeats. Calcium channel blockers like amlodipine or felodipine relax your arteries. Decongestants force them to tighten. This creates a tug-of-war that can lead to sudden spikes - sometimes over 180/110 mmHg - which is a medical emergency. And it’s not just about the decongestant itself. Many cold medicines are loaded with sodium. The American Heart Association warns that high-sodium medications can worsen fluid retention and raise blood pressure even more. A single tablet might contain 200-500 mg of sodium - that’s nearly a quarter of your daily limit.
Safe Alternatives for Congestion Relief
You don’t need to suffer through a stuffy nose. There are safer ways to breathe easier - and none of them involve vasoconstrictors.- Nasal saline spray - Plain saltwater spray or a neti pot rinses out mucus and irritants without affecting your blood pressure. Use it 2-3 times a day.
- Humidifiers and steam - Breathing warm, moist air from a shower or a bowl of hot water helps open nasal passages. Add a drop of eucalyptus oil if you like - it’s safe and soothing.
- Antihistamines - If your congestion is from allergies (not a cold), loratadine (Claritin) or cetirizine (Zyrtec) can help. They reduce inflammation, not blood vessel size. Avoid combination products with decongestants - check the label.
- Hydration and rest - Drink plenty of water. Sleep with your head slightly elevated. Your body heals faster when it’s not fighting dehydration or exhaustion.
How to Read Labels Like a Pro
You can’t trust the front of the box. The word "cold" or "sinus" doesn’t tell you what’s inside. You have to look at the active ingredients. Here’s what to scan for:- Pseudoephedrine
- Phenylephrine
- Oxymetazoline
- Ephedrine
- Any product labeled "D" or "-D" - like Claritin-D - means it contains a decongestant.
What to Do If You’ve Already Taken a Decongestant
If you accidentally took a decongestant and you’re on blood pressure medication, don’t panic - but act fast.- Check your blood pressure immediately. If it’s over 160/100, call your doctor or go to urgent care.
- Stop taking the product. Don’t wait for symptoms. Even if you feel fine, your blood pressure could be climbing.
- Drink water. Hydration helps flush out the medication faster.
- Monitor for signs of trouble: chest pain, rapid heartbeat, severe headache, blurred vision, or shortness of breath. These are red flags.
When a Decongestant Might Be Okay (With Doctor’s Approval)
There are rare cases where a doctor might say it’s okay to use a decongestant - but only under strict conditions:- Your blood pressure is well-controlled (below 140/90) for at least 3 months.
- You’re using the lowest possible dose - one tablet, not two.
- You’re taking it for no more than 3 days.
- You’re checking your blood pressure twice a day during use.
- You’re not taking any other meds that interact with decongestants - like antidepressants or MAO inhibitors.
Why Most People Don’t Realize the Risk
A 2024 survey by the Cleveland Clinic found that only 38% of people with high blood pressure knew decongestants could raise their blood pressure. Most assume: "It’s just a nose spray," or "I’ve taken this before and felt fine." But here’s the problem: the effects are cumulative. One dose might not do much. Two doses over a few days? That’s when blood pressure starts to climb. And if you’re taking it every time you get a cold - which could be 3-4 times a year - you’re slowly undermining your treatment. Pharmacists are your best defense. Studies show that when patients get a simple 5-minute consultation from a pharmacist about OTC meds, inappropriate decongestant use drops by 47%. Don’t skip that step.What’s Changing in 2025 and Beyond
The medical community is waking up to this issue. The American Heart Association updated its guidelines in 2023 to make warnings stronger. The FDA now requires all decongestant labels to say: "Ask a doctor before use if you have high blood pressure." Pharmaceutical companies are also working on new options. As of mid-2025, at least three companies are in Phase 2 trials for non-vasoconstrictive decongestants - drugs that open nasal passages without affecting blood pressure. These could be available by 2027. Until then, the safest choice is simple: skip the decongestant. Your heart will thank you.Can I use saline nasal spray if I have high blood pressure?
Yes, saline nasal spray is completely safe for people with high blood pressure. It works by moisturizing and flushing out mucus without affecting blood vessels or heart rate. It’s one of the top recommended alternatives by the American Heart Association and major clinics like Mayo and Cleveland Clinic.
Is phenylephrine safer than pseudoephedrine for high blood pressure?
No, phenylephrine is not safer. Although it’s now the most common decongestant in OTC products, studies show it still raises blood pressure - sometimes just as much as pseudoephedrine. Both are risky for people with hypertension. Neither should be used without a doctor’s approval.
Can I use Afrin (oxymetazoline) nasal spray with high blood pressure?
No. Even though it’s a nasal spray, oxymetazoline can be absorbed into your bloodstream and raise your blood pressure. The FDA and American Heart Association warn against its use in people with hypertension. Using it for more than 3 days can also cause rebound congestion, making your nose worse.
What cold medicine is safe for high blood pressure?
Avoid all multi-symptom cold medicines unless they’re labeled "for high blood pressure" - and even then, check the ingredients. Safe options are single-ingredient: saline spray, antihistamines like loratadine (if allergies are the cause), or plain pain relievers like acetaminophen for fever or aches. Always read the active ingredients list.
How long does it take for decongestants to affect blood pressure?
Effects can start within 30 to 60 minutes after taking an oral decongestant. Blood pressure may peak within 2-4 hours. For nasal sprays, effects can be faster - sometimes within 15 minutes. That’s why it’s critical to check your blood pressure right after taking one, especially if you’ve never taken it before.
Should I stop my blood pressure medication if I need a decongestant?
Never stop your blood pressure medication without talking to your doctor. Stopping it suddenly can cause dangerous spikes in pressure. Instead, avoid the decongestant or ask your doctor for a safer alternative. Your blood pressure meds are protecting your heart - don’t risk it.





Julie Roe
November 18, 2025 AT 09:45 AMJust took Sudafed last week for my cold and felt like my heart was gonna explode bruh
jalyssa chea
November 19, 2025 AT 07:49 AMi always thought nasal spray was safe cause its local but turns out its not lol
Gary Lam
November 21, 2025 AT 01:46 AMSo the FDA finally added a warning like 50 years after people started dropping dead from decongestants? Classic. Guess we need another 20 years before they admit sugar is just as bad.
Andrew Cairney
November 23, 2025 AT 01:23 AMThey’re hiding this on purpose. Big Pharma makes billions off people like us buying decongestants every season. The real cure? Stop trusting corporations and start using salt water. They don’t want you to know that saline costs 3 cents and doesn’t need a patent.
And don’t get me started on how the FDA lets phenylephrine stay on shelves when studies prove it’s useless and dangerous. This is all a scam. I’ve seen the documents. They know. They just don’t care.
My uncle had a stroke after taking DayQuil. They told him it was "just a cold." Now he’s on a feeding tube. Coincidence? I think not. 🤔
Next time you reach for that bottle, ask yourself: Who profits? Who benefits? Who’s silent?
It’s not paranoia if they’re really out to get you.
Rob Goldstein
November 24, 2025 AT 02:31 AMAs a clinical pharmacist, I see this every single week. Patients come in with BP readings over 180/110 after taking "just one pill" for congestion. The worst part? They never connect the dots because the label doesn’t scream "DANGER."
Here’s what I tell everyone: if you’re on antihypertensives, treat every OTC cold med like a controlled substance. Read the active ingredients like your life depends on it - because it does.
Saline sprays, humidifiers, hydration, and rest aren’t just "alternatives" - they’re the gold standard. And yes, they work. I’ve had patients go from 170/100 to 125/80 in 48 hours just by ditching the decongestants.
Pro tip: if it says "-D" on the box, walk away. That D stands for "dangerous" in my book.
Also, don’t forget the sodium. Some cold tablets have more salt than a bag of chips. That’s two mechanisms wrecking your BP at once. It’s not a coincidence.
Pharmacists are here to help. Don’t be shy. Bring your bottle in. We’ve seen it all. We’ve saved lives just by asking, "What else are you taking?"
vinod mali
November 24, 2025 AT 08:32 AMin india we use steam and tulsi leaves for cold no need for chemicals
Jennie Zhu
November 26, 2025 AT 03:14 AMIt is imperative to underscore the pharmacodynamic antagonism between sympathomimetic agents and antihypertensive regimens, particularly beta-adrenergic blockers and calcium channel blockers. The resultant vasoconstriction induces a compensatory increase in systemic vascular resistance, thereby negating therapeutic efficacy and precipitating hypertensive crises.
Furthermore, the concomitant administration of sodium-laden excipients exacerbates fluid retention, further compromising cardiovascular homeostasis.
Adherence to non-pharmacologic interventions - including isotonic saline irrigation, environmental humidification, and positional elevation - constitutes the current standard of care for upper respiratory congestion in patients with hypertension.
Physician and pharmacist collaboration remains indispensable in mitigating inadvertent iatrogenic harm.
Kathy Grant
November 26, 2025 AT 21:28 PMI used to think I was being smart - taking "just one" decongestant every time I got a cold. Like a little reward for suffering through sniffles.
Turns out, I was slowly sabotaging my own health. Every time I took it, I’d feel jittery, my heart would race, and I’d blame stress or coffee.
Then I started tracking my BP. One day, after taking a "safe" allergy pill, my reading jumped from 128/80 to 172/104. I sat there, staring at the machine, thinking, "Wait… did I just do this to myself?"
It wasn’t the cold that was dangerous. It was the solution I kept choosing.
Now I keep saline spray on my nightstand. I breathe steam before bed. I drink water like it’s my job.
And I don’t feel like I’m missing out anymore. I feel like I’m finally listening to my body - not the marketing on the bottle.
It’s not about being perfect. It’s about being aware.
And awareness? That’s the real medicine.
Robert Merril
November 27, 2025 AT 17:29 PMphenylephrine is useless anyway why even bother its just sugar water with a fancy name
also why is pseudoephedrine behind the counter but phenylephrine everywhere? because they knew it was garbage and wanted to sell the fake one instead
and dont even get me started on how they hide sodium in the inactive ingredients like its a secret
Noel Molina Mattinez
November 28, 2025 AT 01:25 AMmy mom died from a stroke after taking cold medicine she thought was safe
they never told her
why dont they just put red warnings on everything
Roberta Colombin
November 29, 2025 AT 03:57 AMThank you for sharing this so clearly. I’ve shared this with my elderly neighbors who don’t always read labels. One of them was taking NyQuil every night for weeks. We switched her to saline and steam - her BP dropped by 15 points in two weeks. Small changes matter.
Let’s keep talking about this. So many people are unaware. We can help each other stay safe.
Peter Stephen .O
November 30, 2025 AT 08:11 AMBro I just found out my "allergy relief" pill had phenylephrine in it and I’ve been taking it for 3 years 😳
My BP was always "borderline" - now I get it. I switched to saline spray and feel way better. No more headaches. No more heart pounding after a nap.
Also, eucalyptus steam is my new BFF. Smells like a spa, works like magic. No pills. No panic. Just breathe.
PS: If you’re still using Afrin… put it down. Walk away. Your nose will thank you. And so will your heart ❤️
Dave Feland
December 1, 2025 AT 21:00 PMLet us not conflate anecdotal evidence with clinical epidemiology. The 22% statistic cited is misleading without adjustment for confounding variables - age, comorbidities, medication noncompliance, and polypharmacy. Moreover, the FDA’s labeling requirement is a defensive legal maneuver, not a reflection of causal certainty.
Phenylephrine’s efficacy remains questionable, but its cardiovascular risk profile is not statistically distinct from placebo in many meta-analyses. The hysteria surrounding decongestants is disproportionate to the actual incidence of adverse events.
One must also consider that the majority of patients with well-controlled hypertension tolerate these agents without incident. The real issue lies in patient education, not product demonization.
It is the duty of the informed to avoid fearmongering - not to amplify it.