When you're taking digoxin, a heart medication used to treat atrial fibrillation and heart failure by slowing the heart rate and strengthening contractions. Also known as digitalis, it's powerful—but narrow in its safe range. Too little won't help your heart. Too much can stop it. That’s why digoxin monitoring isn’t optional. It’s essential. Doctors don’t just prescribe it and walk away. They track your blood levels, watch for symptoms, and adjust based on how your body responds.
Why does this matter so much? Because serum digoxin levels, the measured amount of digoxin in your bloodstream need to stay between 0.5 and 2.0 ng/mL. Even a small rise above that can cause nausea, confusion, blurred vision, or dangerous heart rhythms. And it’s not just about the dose you take. Things like kidney function, how well your kidneys clear digoxin from your body play a huge role. If your kidneys slow down—common in older adults or people with chronic disease—digoxin builds up fast. Other drugs, like diuretics, medications that flush out fluid and can lower potassium levels, make things worse. Low potassium? That makes your heart extra sensitive to digoxin’s toxic effects. Even something as simple as dehydration or a change in diet can throw your levels off.
That’s why regular blood tests aren’t just routine—they’re lifesaving. You won’t feel toxicity until it’s advanced. By the time you’re dizzy or your heart is skipping beats, it’s already too late. Monitoring catches problems before they escalate. Your doctor will check levels after starting the drug, after any dose change, and if you get sick or start a new medication. They’ll also look at your electrolytes, especially potassium and magnesium, because those are digoxin’s silent partners in crime.
People on digoxin often take it for years. It’s not a quick fix. It’s part of a long-term plan for heart health. But that long-term use means you need to stay alert. If you’re on other meds—like antibiotics, antifungals, or even over-the-counter supplements—you need to tell your doctor. Some of those can spike your digoxin levels without you knowing. And if you’ve ever had a bad reaction to heart meds before, that’s even more reason to stay on top of monitoring.
The posts below give you real-world context: how digoxin interacts with other drugs, what symptoms to watch for, how kidney issues change dosing, and why some patients need more frequent checks than others. You’ll find comparisons with similar heart medications, tips for avoiding dangerous combinations, and what to ask your doctor during your next visit. This isn’t theory. It’s what people actually deal with—and what works when the stakes are high.
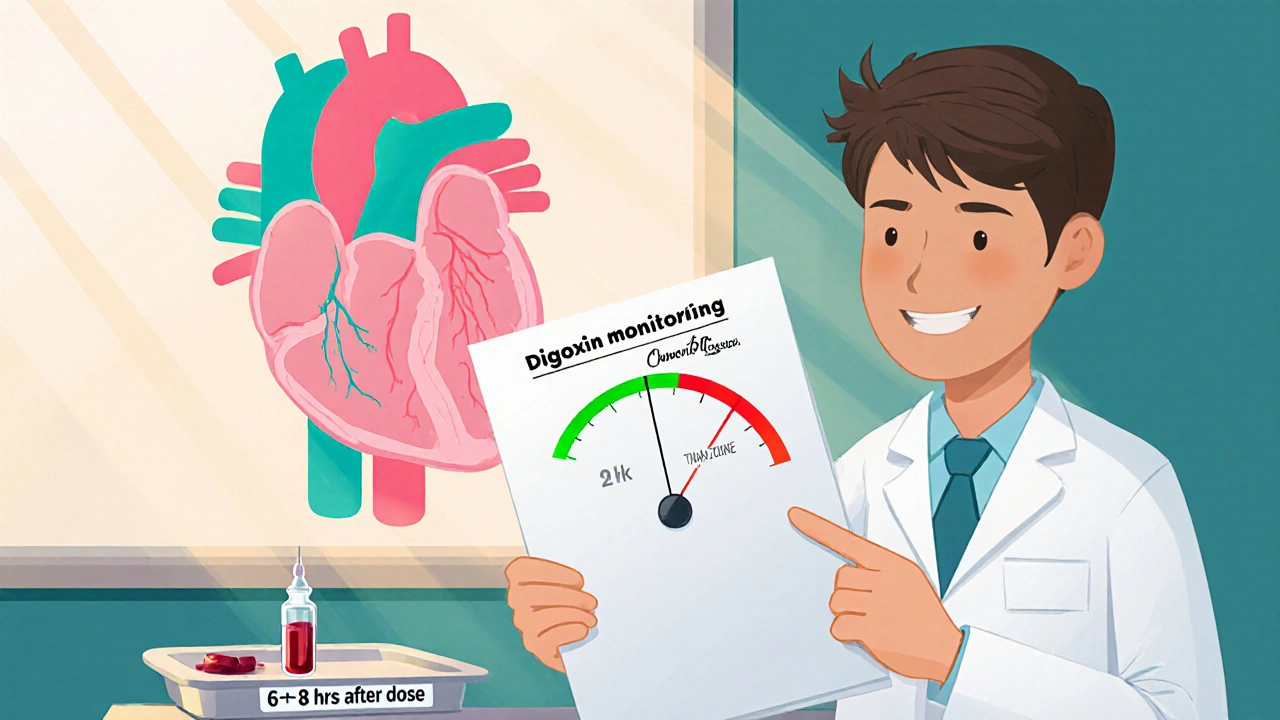
Learn why regular digoxin monitoring saves lives, how to interpret serum levels, and practical steps for safe dosing.
read more