When a child takes a medicine, their body doesn’t respond the same way an adult’s does. It’s not just a smaller version of an adult - it’s a completely different system in motion. A baby’s liver is still learning how to break down drugs. A toddler’s kidneys are still growing into full function. Even their body water percentage changes dramatically as they grow. These differences aren’t minor tweaks - they’re life-or-death factors in how drugs work or harm children.
Why Kids React Differently
Children aren’t just small adults. Their bodies are changing every single day. In newborns, body water makes up 75-80% of their weight - compared to about 60% in adults. That means drugs spread differently through their tissues. A dose that works fine for a 150-pound teen might flood a 20-pound infant’s system with too much medication.
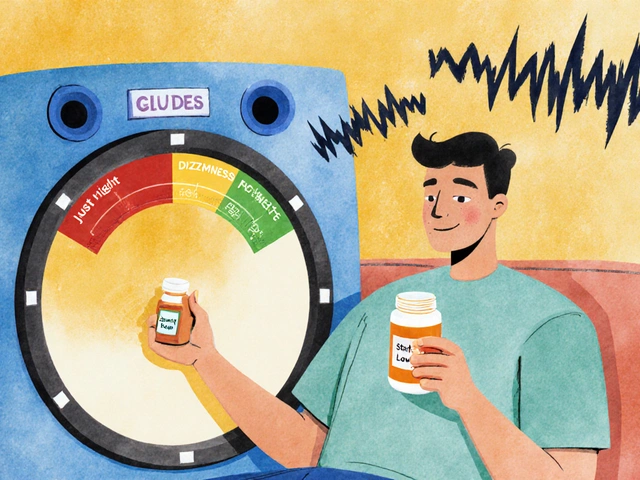
Enzymes in the liver - the body’s main drug-processing system - develop at different rates. For example, cytochrome P450 enzymes, which break down most medications, are only 30-40% active in newborns. By age one, some of those same enzymes are working at 200% of adult levels. That’s why a drug that causes drowsiness in an adult might make a toddler hyperactive: the drug isn’t being broken down fast enough, or it’s being broken down too fast.
And it’s not just the liver. Kidney function, gut absorption, blood-brain barrier maturity, and even how drugs move in and out of cells - all of these change with age. A drug that’s safe for a 10-year-old could be dangerous for a 2-year-old, even if they weigh the same.
The Most Dangerous Drugs for Kids
Not all medications are created equal when it comes to children. Some drugs that are routine for adults carry hidden risks for kids. The KIDs List - developed by Mayo Clinic researchers and published in American Family Physician in 2021 - highlights the most dangerous medications for children. Here are a few:
- Loperamide (Imodium): Used for diarrhea, but can cause fatal heart rhythm problems in children under 6. The FDA has issued multiple warnings about its use in young kids.
- Aspirin: Linked to Reye’s syndrome - a rare but deadly condition that causes swelling in the liver and brain. It’s been largely avoided in children with viral infections like the flu or chickenpox.
- Codeine: Metabolized differently in kids due to genetic variations. One in 30 children are ultra-rapid metabolizers, turning codeine into morphine too quickly - leading to breathing problems or even death.
- Benzocaine teething gels: Caused over 400 cases of methemoglobinemia (a condition that stops blood from carrying oxygen) between 2006 and 2011. The FDA banned their use in children under 2.
These aren’t rare cases. The FDA Adverse Event Reporting System (FAERS) recorded over 264,000 pediatric drug reactions between 2000 and 2023. Nearly half of those were serious enough to require hospitalization.
The Vulnerable Window: Age Two
One of the most surprising findings from recent research is that the second year of life - between ages 1 and 2 - is a high-risk period for certain drug reactions. A 2023 Columbia University study found that children in this age group had a 3.2-fold higher risk of psychiatric side effects from montelukast, a common asthma medication.
Why? At this age, brain development is accelerating. Neurotransmitter systems are still wiring themselves. The liver enzymes processing the drug are maturing unevenly. The blood-brain barrier - which normally blocks harmful substances - isn’t fully formed yet. So a drug that might cause mild sleepiness in an adult can trigger anxiety, aggression, or hallucinations in a toddler.
That’s why pediatric drug safety isn’t just about weight-based dosing anymore. It’s about developmental stage. Two 20-pound children - one 14 months old, one 22 months old - may need completely different dosing strategies because their bodies are at different biological turning points.

How Common Are Side Effects?
Adults experience adverse drug reactions in about 6.7% of cases, according to a 2017 JAMA study. For children, the numbers are more complex.
- Outpatient prescriptions: 2-5% of children have side effects (older studies).
- Hospitalized children: Up to 18% experience at least one adverse drug reaction (2021 study).
- Of those hospital reactions: Nearly half are serious or life-threatening.
Some drug classes are especially risky:
- Antihistamines: Cause CNS effects (drowsiness, agitation) in 15-20% of kids - double the rate in adults.
- Antibiotics: Cause GI upset (diarrhea, vomiting) in 25-30% of children - compared to 10-15% in adults.
- Psychiatric drugs: Children under 12 have 2-3 times the risk of severe reactions like suicidal thoughts or movement disorders.
The most common side effects reported to the FDA in 2022? Antibiotics (48%), central nervous system drugs (18%), and respiratory meds (12%).
Why So Many Drugs Are Used Off-Label
Here’s the uncomfortable truth: about half of all medications prescribed to children have never been formally tested for safety or dosing in pediatric populations. That’s not because doctors are careless - it’s because the science hasn’t caught up.
Only 50% of drugs approved for adults since 2002 have received pediatric labeling. The Best Pharmaceuticals for Children Act (2002) and the Pediatric Research Equity Act (2003) helped, but progress is slow. Pharmaceutical companies still see pediatric trials as expensive and logistically hard.
As a result, 79% of drugs used in neonatal intensive care units are given off-label. In children with rare diseases? That number jumps to 95%. Many of these kids are getting drugs that were never designed for them - dosed by guesswork, based on adult formulas.
What Parents and Doctors Can Do
There’s no perfect solution - but there are smart steps:
- Ask if the drug has been studied in children. If it’s been approved for adults but not kids, ask why - and what alternatives exist.
- Use weight-based dosing. Never assume an adult dose scaled down by size. Use mg/kg calculations and check against pediatric dosing charts.
- Track symptoms. Keep a simple log: what was given, when, and any changes in behavior, sleep, appetite, or skin. Side effects often show up in subtle ways - irritability, refusal to eat, or unusual sleep patterns.
- Know the red flags. Seek immediate help if your child has difficulty breathing, facial swelling, rapid heartbeat not explained by the drug (like antibiotics causing tachycardia), or sudden confusion or seizures.
- Use trusted resources. The Pediatric Drug Safety portal (PDSportal) and KidSIDES (both launched in 2023) offer free, evidence-based data on drug reactions by age.
For mild reactions - like a temporary rash or upset stomach - doctors often advise continuing the medication. These often fade after a few days. But don’t assume it’s harmless. Always report it.
The Future: Precision Pediatric Medicine
The next big shift is moving from "one size fits all" to precision dosing. Researchers are now using pharmacogenomics - testing a child’s genes to predict how they’ll respond to drugs.
The NIH just funded a $15 million study (R01-GM141804) to build age-specific genetic guidelines. Imagine a child getting a DNA test at their first doctor’s visit that tells the doctor: "This kid metabolizes codeine dangerously fast. Avoid it completely."
Also emerging: better computer models that simulate how drugs behave in growing bodies. These aren’t just guesses - they’re built from real data on enzyme activity, organ development, and body composition across hundreds of pediatric patients.
The American Academy of Pediatrics is now pushing for a new rule: all new drugs targeting conditions that affect children must be developed with pediatric formulations from day one. That could prevent 30,000-50,000 hospitalizations each year.
Final Thoughts
Children aren’t small adults. They’re developing organisms with unique, changing biology. What works safely in a 10-year-old might be dangerous for a 3-year-old. What’s routine for a parent might be risky for their child.
The science is catching up - but slowly. Until then, parents and doctors need to be extra cautious. Ask questions. Track symptoms. Use updated tools. And remember: a child’s reaction to a drug isn’t just about dose - it’s about development.
Are all side effects in children serious?
No. Many side effects - like mild nausea, drowsiness, or a temporary rash - are common and go away after a few days. But up to half of all pediatric drug reactions are serious enough to require hospitalization. The key is knowing which symptoms to watch for and when to call a doctor. Don’t ignore changes in behavior, breathing, or heart rate.
Why aren’t more drugs tested on children?
Testing drugs on children is expensive, slow, and ethically complex. Companies don’t always see a big enough market to justify the cost. Even though children make up 22% of the U.S. population, pediatric drugs only account for 12-15% of the global pharmaceutical market. Regulatory incentives exist, but they haven’t closed the gap. That’s why so many drugs are used off-label - because there’s no data for kids.
Can I give my child an adult medication if I cut the dose in half?
Never. Pediatric dosing isn’t just about weight. It’s about how the child’s body absorbs, processes, and eliminates the drug - and those systems change dramatically with age. A 10-year-old might handle a half-dose of an adult drug safely, but a 3-year-old might overdose. Always use a pediatric-specific formulation or consult a pediatric pharmacist.
What should I do if my child has a reaction to a new medication?
For mild symptoms like upset stomach or drowsiness, keep giving the medicine and monitor. These often pass in 2-3 days. For serious symptoms - trouble breathing, swelling, fast heartbeat, seizures, or extreme drowsiness - stop the medicine and seek emergency care immediately. Report the reaction to the FDA’s MedWatch program or your child’s doctor.
Is there a list of drugs I should avoid for my child?
Yes. The KIDs List identifies 12 high-risk medications for children, including loperamide, aspirin, codeine, and benzocaine gels. It’s updated annually and available through the American Academy of Pediatrics and the FDA’s Pediatric Drug Safety portal. Always check this list before giving any new medication to a child under 12.





Lyle Whyatt
February 8, 2026 AT 23:17 PMMan, I never realized how wild it is that a baby's liver is basically a toddler learning to drive a car while the engine's still being built. I had my daughter on amoxicillin last year, and she went from sweet as pie to screaming at 3am like she was possessed. We thought it was teething. Turns out? The drug was just sitting in her system like a drunk uncle at a family reunion. The liver enzymes weren't ready. And now I'm reading up on the KIDs List like it's a survival manual. Seriously, if you're giving your kid anything that says "adult dosage" on the bottle - pause. Breathe. Ask your pharmacist. I did. They gave me a pamphlet. I cried. Not because I'm weak - because this stuff is terrifyingly under-discussed.
My son's 18 months now. I keep a Google Doc. Every med. Every dose. Every weird behavior change. "Day 3: Refused oatmeal. Stared at ceiling fan for 45 mins." That's not a phase. That's a pharmacokinetic nightmare. We need better labeling. We need pediatric-specific trials. We need to stop pretending kids are just tiny adults with better sleep schedules.
And honestly? I'm mad. Pharma companies know this. They've known for decades. But the ROI on pediatric trials? Too low. So kids become collateral damage in a profit-driven system. I get it - science is hard. But we're not talking about rare diseases here. We're talking about antibiotics, antihistamines, asthma meds - stuff every kid gets. This isn't niche. This is every parent. And we're being left in the dark.
I'm not saying don't medicate. I'm saying: know what you're giving. Track it. Question it. Demand better. My kid's not a lab rat. And neither are yours.
Tatiana Barbosa
February 10, 2026 AT 22:37 PMJust read this and I’m so glad I found this thread. My daughter was on montelukast for mild asthma and started having nightmares so intense she’d wake up screaming ‘the monsters are in the walls!’ We thought it was trauma from daycare. Nope. 3.2x risk at age 2. That’s not a coincidence. I’m telling every mom I know. You have to ask about developmental stage, not just weight. I’m sharing this post. Someone needs to make a TikTok series on this. #PediatricMedSafety #AskYourPharmacist
Ryan Vargas
February 11, 2026 AT 09:09 AMLet’s be honest: the entire pediatric pharmacology system is a Ponzi scheme built on the assumption that children are disposable test subjects. The FDA’s Adverse Event Reporting System? A joke. 264,000 reactions and zero mandatory reporting from pharma. The KIDs List? A PR stunt. They don’t ban drugs - they just slap on a warning and call it a day. And the Best Pharmaceuticals for Children Act? A toothless tiger. The real problem isn’t lack of data - it’s lack of accountability. Who profits? The same people who designed the system. Who pays? The parents. Who gets punished? No one. This isn’t negligence. It’s structural violence disguised as medical science. And until we start holding executives accountable - not just doctors - we’re just rearranging deck chairs on the Titanic.
Simon Critchley
February 13, 2026 AT 00:02 AMOkay, so we’ve got enzymes at 200% adult capacity in toddlers? That’s wild. I mean, imagine your body’s a car and suddenly the engine revs to redline every time you take a Tylenol. And benzocaine gels? 400 cases of methemoglobinemia? That’s not an accident - that’s a systemic failure. I’ve seen parents give kids OTC meds like candy. "It’s just a little something for the cough." No. It’s a chemical gamble. And the worst part? The pediatric pharmacists are the unsung heroes here. They’re the ones doing the math, the cross-references, the risk assessments. We need to pay them more. And train more. And stop treating them like pharmacy assistants. They’re pediatric pharmacokinetic engineers. And we’re not even giving them a medal.
John McDonald
February 14, 2026 AT 07:47 AMMy son had a reaction to amoxicillin too - rash, fever, super irritable. We thought it was a virus. Turns out, it was a mild hypersensitivity. We stopped it, and he bounced back in 48 hours. The doc said "common" and moved on. But reading this? I realized how lucky we were. I’m now keeping a meds journal. Every pill. Every time. Every weird behavior. It’s not paranoia - it’s protection. And yeah, off-label use is everywhere. But if you’re asking "is this safe?" - you’re already doing better than 90% of parents. Keep going. You’re not alone.
Chelsea Cook
February 16, 2026 AT 06:45 AMOh honey, you’re telling me that a 20-pound toddler can get a drug that turns into morphine because of their genes? And no one told you until it was too late? Welcome to parenting in 2025. I had to Google "codeine genetic metabolizer" after my niece almost died. It’s not about being paranoid - it’s about being informed. And if your pediatrician says "it’s fine" without checking the KIDs List? Find a new one. Seriously. Your kid’s brain is a minefield. And you’re the bomb squad. Don’t let anyone tell you otherwise.
John Sonnenberg
February 16, 2026 AT 18:12 PMWHEN I WAS A KID, WE TOOK ASPIRIN FOR FEVERS. NOW WE’RE TOLD IT CAN KILL THEM. WHEN I WAS A KID, WE GOT ANTIBIOTICS FOR EVERY COUGH. NOW WE’RE TOLD THEY CAUSE 30% GI ISSUES. WHEN I WAS A KID, WE WERE GIVEN MEDS WITHOUT A CLUE. NOW WE’RE TOLD TO TRACK EVERY SNEEZE. I’M NOT SAYING WE SHOULD STOP MEDS. I’M SAYING WE’VE GONE FROM "NO RULES" TO "PARANOIA AS STANDARD PRACTICE." AND NOW PARENTS ARE SCARED TO GIVE A CHILD A SINGLE PILLS. WHAT’S NEXT? DO WE NEED A BACKGROUND CHECK BEFORE GIVING A BAND-AID?
Joshua Smith
February 16, 2026 AT 18:58 PMThis is fascinating. I work in bioinformatics and I’ve seen how messy pediatric pharmacokinetic data is. We’re trying to model enzyme development across age groups - but the datasets are tiny. Most studies have under 200 kids. How do you build a predictive model on that? And yet, we’re dosing millions of children with this data. The NIH’s $15M project? A start. But we need global collaboration. Not just U.S. trials. We need data from Brazil, India, Nigeria - kids with different genetics, diets, microbiomes. This isn’t just about weight. It’s about biology in context. And we’re still in the Stone Age.
Jessica Klaar
February 18, 2026 AT 18:01 PMAs a mom of two and a former nurse in a pediatric ER, I’ve seen the fallout. A 14-month-old with loperamide-induced cardiac arrest. A 3-year-old with codeine-induced respiratory failure. I’ve held mothers while they sobbed because they thought they were doing the right thing. This isn’t about blame. It’s about awareness. We need mandatory pediatric pharmacology training for all pediatricians. Not optional. Not "if you have time." Mandatory. And we need a national database - like a CDC registry - for every pediatric drug reaction. Not just "report if you want." We need to track this like we track measles outbreaks. Because it’s just as deadly.
PAUL MCQUEEN
February 19, 2026 AT 14:13 PMYeah, sure. Another article about how scary drugs are. I’ve been giving my kids ibuprofen since they were 6 months old. No issues. My neighbor’s kid took codeine and had a bad reaction? Maybe she didn’t read the label. Or maybe she’s just a bad parent. This whole thing feels like fearmongering. We’ve been giving kids meds for 100 years. We’re not all dying. Maybe the system isn’t broken - maybe you’re just overthinking it.
glenn mendoza
February 19, 2026 AT 20:13 PMIt is with profound gravity that I acknowledge the profound vulnerability of the pediatric population in the context of pharmacological intervention. The physiological discontinuities between neonatal, infant, and juvenile metabolic pathways are not merely quantitative differences, but qualitative transformations in homeostatic regulation. The absence of standardized, age-stratified pharmacokinetic models constitutes a systemic deficiency in clinical translational science. I respectfully urge the medical community to prioritize the integration of developmental pharmacology into core medical curricula, and to advocate for legislative mandates requiring pediatric-specific formulation development as a prerequisite for FDA approval of any drug with pediatric indication potential. The moral imperative is unequivocal.
Kathryn Lenn
February 20, 2026 AT 11:45 AMLet’s be real - the whole "pediatric drug safety" movement is just Big Pharma’s way of pushing expensive genetic testing. They don’t care about kids. They care about patent extensions. The KIDs List? A marketing tool. The NIH study? Funded by a pharma-linked foundation. The "precision dosing" dream? A cash grab. They’ll sell you a $500 DNA test and then charge $200 for a "personalized" dose. Meanwhile, generic amoxicillin? Still $4. Who benefits? Not you. Not your kid. The system is rigged. And the "experts" are just the paid shills.
John Watts
February 21, 2026 AT 03:06 AMI work in global health in Kenya. We don’t have pediatric-specific formulations. We crush adult pills. We use weight-based dosing because we have no choice. And guess what? Kids survive. Sometimes they don’t. But we don’t have the luxury of waiting for FDA-approved labels. This post is great for the U.S. - but for the rest of the world? It’s a luxury. We need affordable, scalable solutions - not just fancy genetic testing. Can we get a global database? Can we get donated pediatric formulations? Can we stop assuming that every solution has to be high-tech? Sometimes, the right answer is just a better pill crusher and a trained community health worker.
Angie Datuin
February 21, 2026 AT 08:51 AMMy son had a rash after his first antibiotic. We thought it was an allergy. We stopped it. He got better. Two months later, he got sick again. We gave the same antibiotic. No rash. Turned out it was a coincidence. I didn’t know side effects could be temporary. I thought "reaction" meant "permanent." So I learned. And now I don’t panic. I observe. I wait. I call the pediatrician. Not because I’m scared - because I’m informed.