Osteoarthritis is a degenerative joint disease that gradually wears away cartilage, causing pain, stiffness, and reduced mobility. It most often affects the knees, hips, hands, and spine, and its prevalence rises sharply after age 50. In the UK, roughly 8 million adults live with symptomatic osteoarthritis, according to the National Health Service.
Why Joint Replacement Becomes the Next Step
When conservative measures-weight control, physiotherapy, analgesics, and injections-no longer keep pain under control, doctors may recommend joint replacement surgery. The decision hinges on three factors: persistent pain that interferes with daily life, functional limitation despite optimal medication, and radiographic evidence of joint degeneration.
Types of Joint Replacement Surgery
There are two main procedures for osteoarthritis of the lower limb:
- Total Hip Arthroplasty is a surgical replacement of the hip joint with a metal or ceramic ball and a plastic liner.
- Total Knee Arthroplasty is a procedure that substitutes the knee’s damaged surfaces with metal femoral and tibial components and a polyethylene spacer.
Both aim to restore alignment, relieve pain, and improve range of motion.
| Attribute | Total Hip Arthroplasty | Total Knee Arthroplasty |
|---|---|---|
| Typical Age | 60‑75 years | 65‑80 years |
| Average Hospital Stay | 2‑3 days | 3‑4 days |
| Rehabilitation Timeline | 4‑6 weeks for normal activities | 6‑12 weeks for full strength |
| Implant Materials | Metal‑on‑plastic, ceramic‑on‑plastic | Metal‑on‑plastic, highly cross‑linked polyethylene |
| Long‑Term Survival (10‑yr) | ~95% | ~90‑93% |
Preparing for Surgery
Preparation starts months before the knife goes in. A Pre‑operative Assessment includes blood tests, cardiac evaluation, and imaging to map the joint’s anatomy. Your surgeon-typically an orthopedic specialist-reviews the plan, discusses implant options, and sets realistic expectations.
Key steps include:
- Optimising weight: losing 5‑10% of body weight can cut surgical risk by up to 30%.
- Quitting smoking: smokers face a 2‑3× higher infection rate.
- Medication review: blood thinners, NSAIDs, and certain supplements may need to be paused.
Choosing the right Hospital with a dedicated orthopaedic unit and low infection rates improves outcomes. Facilities accredited by the NHS or private equivalents provide joint replacement pathways that meet national safety standards.
The Day of Surgery: What Happens in the OR
Most hip and knee replacements are now performed under spinal or regional anaesthesia, allowing faster mobilisation. The procedure itself typically lasts 1‑2 hours. Surgeons use Prosthetic Implants custom‑selected based on bone quality, activity level, and anatomy. Modern implants feature porous titanium surfaces that encourage bone ingrowth, enhancing long‑term stability.
During the operation:
- The damaged cartilage is removed.
- Bone is prepared to receive the implant.
- Components are inserted and secured, often with cement‑free fixation.
- Joint stability is tested before closing.
In most UK centres, patients are moved to a recovery area within minutes and encouraged to sit up and swing the leg.

Recovery, Rehabilitation, and Pain Management
Post‑operative care revolves around three pillars: pain control, early mobilisation, and structured physical therapy. A multidisciplinary team-surgeon, anaesthetist, Physical Therapist specialist in joint‑specific rehab exercises, and nursing staff-coordinates the plan.
Pain Management usually combines short‑acting opioids (for the first 24‑48hours) with NSAIDs and, if needed, a peripheral nerve block. By day three most patients report pain scores below 4/10.
Rehab milestones:
- Day 1‑2: Sit up, stand, and take short walks with a walker.
- Week 2‑4: Begin low‑impact exercises (stationary bike, pool therapy).
- Week 6‑12: Progress to strength training, balance drills, and gradual return to normal activities.
Compliance matters-studies from British Orthopaedic Association show that patients who attend at least 80% of prescribed sessions recover 30% faster.
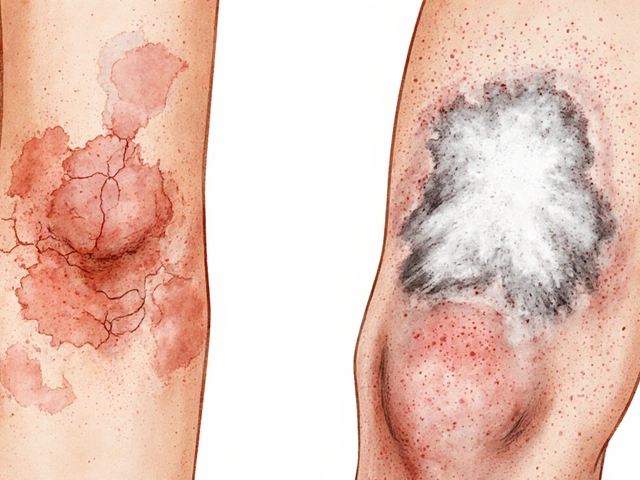
Potential Risks and Complications
While joint replacement is generally safe, every surgery carries risks. Common issues include:
- Infection (approx. 1% incidence, higher in diabetics).
- Blood clots-deep‑vein thrombosis or pulmonary embolism (prevented with anticoagulants).
- Implant loosening or wear, which may require revision surgery after 10‑15 years.
- Stiffness or limited range of motion, often mitigated by early physiotherapy.
Discuss these scenarios with your surgeon so you can weigh benefits against potential downsides.
Long‑Term Outlook and Lifestyle After Replacement
Most patients enjoy substantial pain relief for a decade or more. Research published by the British Medical Journal reports that 90% of hip replacement recipients resume low‑impact activities (walking, cycling) without pain after two years. Knee replacements show similar trends, though high‑impact sports like running may accelerate wear.
Maintaining a healthy weight, staying active, and attending regular follow‑up appointments extend implant lifespan. The implant itself does not “wear out” suddenly; gradual bone loss or polyethylene degradation is what triggers revision.
Related Concepts and Next Topics to Explore
Understanding osteoarthritis and joint replacement opens doors to other areas you might want to read about:
- Cartilage Regeneration: emerging stem‑cell and PRP therapies.
- Arthroscopy: minimally invasive techniques for early‑stage disease.
- Joint Preservation Surgery: osteotomy and unicompartmental knee replacement.
- Post‑Surgery Nutrition: protein‑rich diets that aid tissue healing.
Each of these topics ties back to the core goal of keeping joints functional and pain‑free.

Frequently Asked Questions
How long does a joint replacement surgery take?
A typical total hip or knee replacement lasts between one and two hours, not including anaesthesia preparation.
What is the average hospital stay after a knee replacement?
Most UK hospitals discharge patients after three to four days, provided pain is controlled and the patient can walk safely with assistance.
Can I drive after hip replacement?
Driving is generally safe once you can comfortably perform a left‑leg heel‑toe maneuver, usually about six weeks post‑op for a right‑hand drive.
What exercises are recommended in the first month?
Early range‑of‑motion stretches, ankle pumps, seated quadriceps sets, and short walks with a walker are the cornerstone of the first‑month programme.
How likely is a revision surgery?
Revision rates are around 5% at ten years for hips and 7‑9% for knees, rising to about 15% after twenty years, largely depending on activity level and implant type.
Is spinal anaesthesia safer than general anaesthesia?
Current evidence suggests spinal anaesthesia reduces blood loss and postoperative nausea, making it the preferred choice for most joint replacements.
Can I have a joint replacement if I have osteoporosis?
Yes, but bone density will be evaluated. Cemented implants are often chosen to provide better initial stability in osteoporotic bone.





Mike Privert
September 24, 2025 AT 22:00 PMThanks for the thorough guide! Remember, losing just 5‑10% of body weight can shave a lot off surgical risk, so keep that goal realistic. Stay consistent with the physio exercises; they really set the tone for a smoother rehab. And don’t forget to schedule that pre‑op cardiac check‑up early.
Veronica Lucia
September 26, 2025 AT 15:40 PMThe way joint replacement reshapes daily life is profound; it’s almost a rebirth of mobility. Still, patience during the rehab phase is key to long‑term success.
Sriram Musk
September 28, 2025 AT 09:20 AMThe data you’ve presented aligns well with NHS statistics, especially the 95% ten‑year survival for hips. It’s also worth noting that cement‑free fixation is becoming the norm in many UK centres. Overall, the guide balances risks and benefits effectively.
allison hill
September 30, 2025 AT 03:00 AMSure, but the data on revision rates is often cherry‑picked.
Tushar Agarwal
October 1, 2025 AT 20:40 PMLoved the detail, especially the part about quitting smoking – that can drop infection risk dramatically! 😊 Keep an eye on blood thinners before surgery, they can mess with clotting. Also, choosing a hospital with a dedicated orthopaedic unit really matters. Good luck to anyone heading to the OR!
Richard Leonhardt
October 3, 2025 AT 14:20 PMAwesome rundown! The only thing I'd tweak is to add a quick note about post‑surgery nutrition – protein helps heal faster. Also, a shout‑out to the physio team – they’re the unsung heroes.
Shaun Brown
October 5, 2025 AT 08:00 AMFirst of all, the so‑called ‘modern’ implants are nothing more than overpriced plastic and metal that manufacturers push onto unsuspecting patients.
The industry’s marketing machine has convinced surgeons that newer ceramic‑on‑plastic bearings are inherently superior, yet the long‑term data is still murky.
Patients are told to lose weight, but the underlying societal pressures that lead to obesity are never addressed.
Smoking cessation programs are mentioned, but hospitals often lack the resources to provide real support, so it becomes a mere checkbox.
The emphasis on swift discharge times-two to three days for hips-feels like a cost‑cutting measure rather than patient‑centred care.
Rehab timelines are presented as a one‑size‑fits‑all, ignoring individual variability in pain tolerance and home support.
Pain management protocols still rely heavily on opioids, despite the well‑documented risk of dependence.
Moreover, the statistics on infection rates gloss over the higher numbers observed in diabetic or immunocompromised populations.
Deep‑vein thrombosis prophylaxis is standard, yet many patients experience bleeding complications from anticoagulants.
The guide mentions revision rates around 5‑10% at ten years, but it fails to discuss the psychological toll of facing another major surgery.
Implant longevity is often touted as 15‑20 years, but real‑world wear can accelerate with high‑impact activities like running.
There is a glaring omission of alternative treatments such as stem‑cell therapy, which, while experimental, deserve mention.
Furthermore, the cost burden on the NHS is massive, and taxpayers are rarely informed about the true financial implications.
The ethical considerations of using proprietary implants versus off‑the‑shelf options are absent from the discussion.
In summary, while the guide is comprehensive on the procedural side, it lacks critical analysis of systemic issues surrounding joint replacement.
Damon Dewey
October 7, 2025 AT 01:40 AMEarly mobilisation is crucial; it cuts complications dramatically. Stick to the physio plan and you’ll bounce back faster.
Dan Barreto da Silva
October 8, 2025 AT 19:20 PMWow, this guide feels like a lifeline for anyone terrified of the OR. The step‑by‑step breakdown strips away the drama and replaces it with clear action items.
Ariel Munoz
October 10, 2025 AT 13:00 PMHonestly, if you’re not from a top‑tier hospital, you’re probably getting sub‑par implants. Our country’s health system should prioritize quality over quantity.
Ryan Hlavaty
October 12, 2025 AT 06:40 AMPeople need to understand that opting for surgery isn’t a vanity choice; it’s a medical necessity when pain dominates daily life.
Chris Faber
October 14, 2025 AT 00:20 AMCheers for sharing this, mate. The rehab timeline is spot on – just remember to keep the workouts fun, otherwise motivation drops.
aura green
October 15, 2025 AT 18:00 PMOh great, another checklist of things to do before you cut into your own hip.
Because nothing says ‘I’m ready for surgery’ like counting calories while your knee screams.
I guess the real miracle is how quickly hospitals will discharge you once you can barely stand.
And the physiotherapy schedule? Perfect for anyone who enjoys paying for more appointments.
Let’s not forget the joy of navigating opioid prescriptions without becoming dependent.
Sure, the guide mentions diet, but a protein shake won’t fix a broken cartilage.
If you survive the first six weeks, congratulations-you’ve earned the right to be told to avoid high‑impact sports forever.
All in all, thanks for the optimism, but the reality is a lot less Instagram‑ready. 😊
Edward Morrow
October 17, 2025 AT 11:40 AMLook, the implants are just glorified metal peanuts.
Shayne Tremblay
October 19, 2025 AT 05:20 AMStay motivated during those first weeks; even short walks boost circulation. Remember to celebrate small milestones – each step is progress. And keep that positive attitude; it really influences recovery speed.
Musa Bwanali
October 20, 2025 AT 23:00 PMMike’s point on weight loss is spot‑on; shedding even a few pounds drops the strain on the joint dramatically. Pair that with high‑protein meals and you’ll give the body the resources it needs to heal. Keep the rehab schedule strict and you’ll see results faster.
Allison Sprague
October 22, 2025 AT 16:40 PMWhile brevity is appreciated, the statement oversimplifies a complex dataset; revision rates vary widely based on implant type and patient activity levels. A more nuanced phrasing would better serve readers.
leo calzoni
October 24, 2025 AT 10:20 AMShaun, your exhaustive critique, while thorough, borders on pedantry.
KaCee Weber
October 26, 2025 AT 03:00 AMI get the sarcasm, Aura, but the rehab journey can also be empowering when you see real progress.
Those six weeks of restricted activity often feel endless, yet they lay the foundation for long‑term joint health.
Embracing the prescribed physiotherapy isn’t just about paying for appointments; it’s an investment in mobility.
Balancing pain meds with non‑pharmacologic methods can reduce the risk of dependence while still managing discomfort.
So, keep the humor alive, but also give yourself credit for each milestone you conquer. 😊
Sriram Musk
October 27, 2025 AT 20:40 PMChris makes a good point about keeping workouts enjoyable; motivation is a key determinant of adherence. Mixing in low‑impact activities like swimming can also alleviate joint stress while maintaining fitness.