When you start taking an antidepressant, you expect your mood to improve. But for many people, the first thing that changes is their sleep-and not always for the better. Insomnia, vivid dreams, waking up in the middle of the night, or feeling groggy all day aren’t just side effects. They’re direct results of how these medications interact with your brain’s sleep-wake system. And if you’re already struggling with sleep because of depression, this can make things feel worse before they get better.
Why Antidepressants Disrupt Sleep
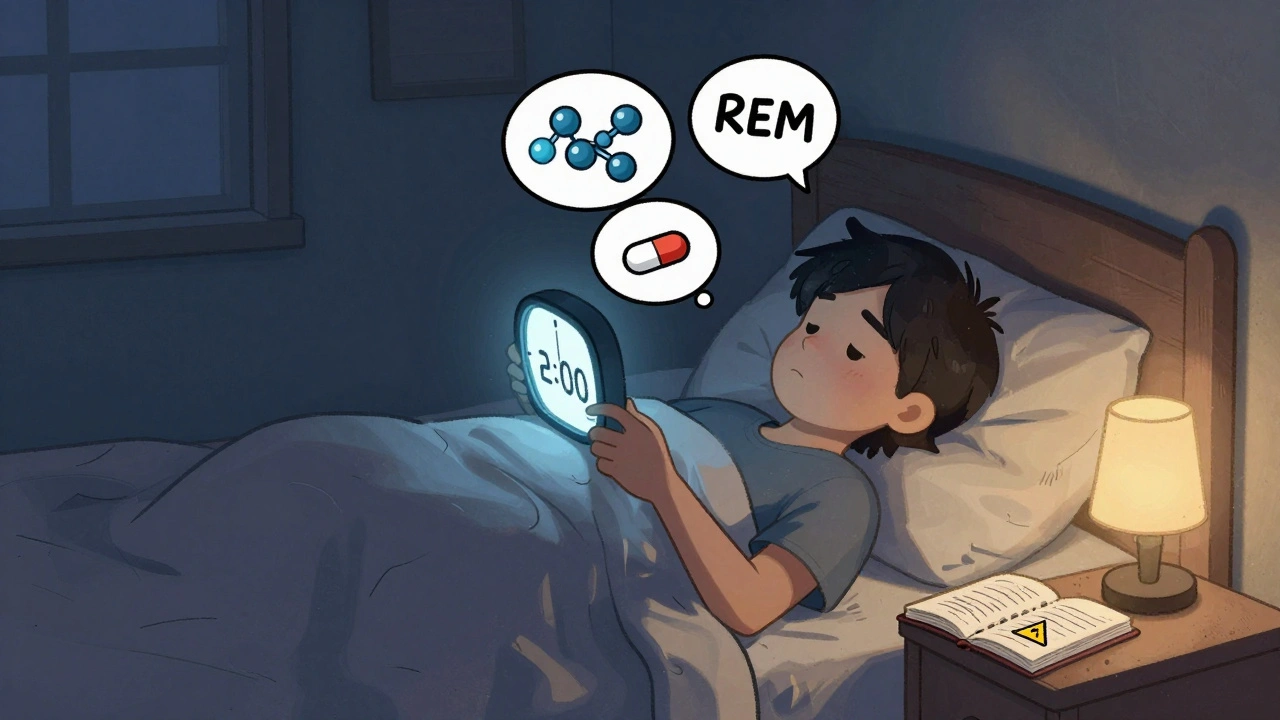
Antidepressants don’t just lift your mood-they tweak the chemicals in your brain that control sleep. Serotonin, norepinephrine, and dopamine are the big players here. These neurotransmitters aren’t just about feeling happy or focused. They also tell your body when to sleep, when to wake up, and how deeply you rest.For example, SSRIs like fluoxetine and sertraline boost serotonin. That’s good for depression, but too much serotonin too soon can shut down REM sleep-the stage where dreaming happens. Studies show SSRIs can reduce REM sleep by up to 29% in the first week. That might sound harmless, but REM suppression is linked to how well the drug works for depression. The catch? When REM sleep gets blocked, many people report trouble falling asleep, restless nights, or even nightmares.
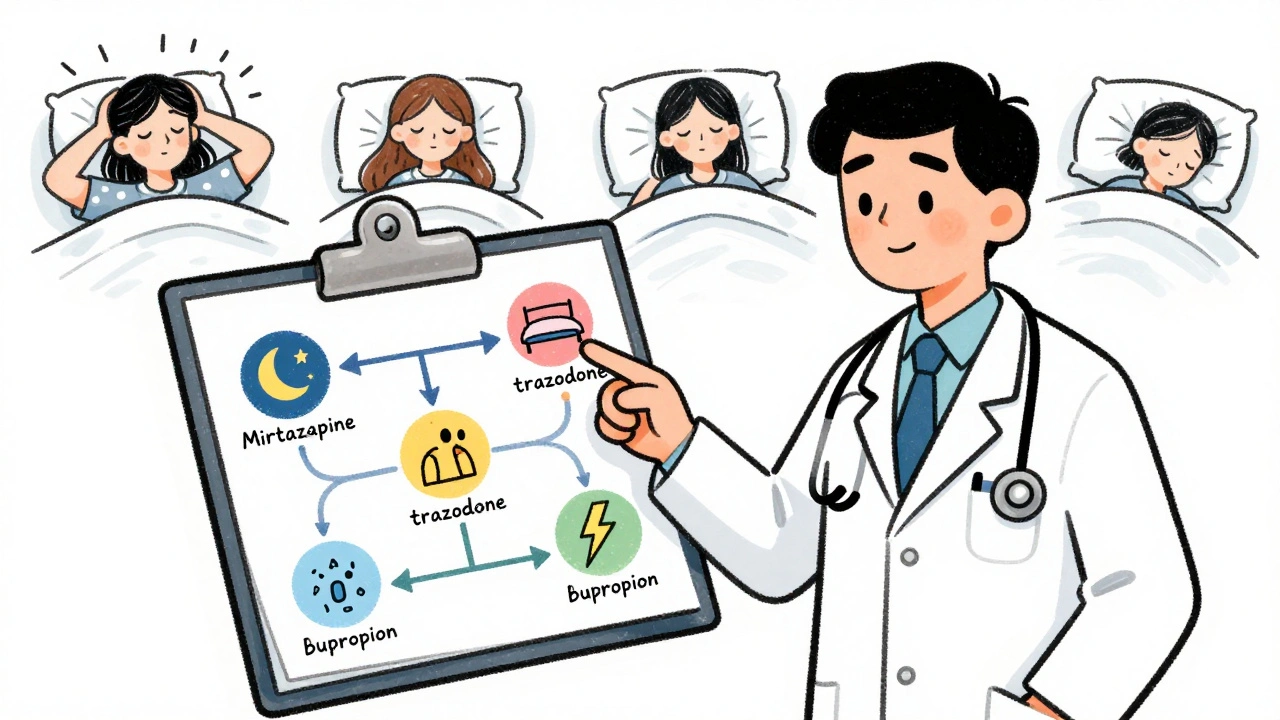
Tricyclics like amitriptyline do the opposite. They increase deep sleep and reduce REM, which can help you feel more rested. But they come with their own trade-offs: dry mouth, weight gain, and next-day drowsiness. Then there’s mirtazapine, which blocks certain serotonin receptors and actually increases total sleep time by nearly an hour on average. It’s one of the few antidepressants that doctors sometimes prescribe specifically for sleep.
Which Antidepressants Cause Insomnia?
Not all antidepressants affect sleep the same way. Some are more likely to keep you awake, others make you sleepy. Here’s what the data shows:- Fluoxetine (Prozac): The most common offender. Up to 78% of users report insomnia in the first two weeks. It’s also the most activating SSRI-some people feel jittery or wired, even at low doses.
- Sertraline (Zoloft): Still causes insomnia in about 65% of users, but less than fluoxetine. Many find it tolerable after the first month.
- Paroxetine (Paxil): Less likely to cause insomnia than other SSRIs, but it can make you feel drowsy during the day. It’s a mixed bag.
- Bupropion (Wellbutrin): This one doesn’t touch serotonin. Instead, it boosts dopamine and norepinephrine. That’s why it’s often used for fatigue and low energy-but it’s also one of the worst for sleep. Over half of users report trouble falling asleep.
- Venlafaxine (Effexor): At low doses, it’s more serotonin-focused and can cause insomnia. At higher doses, it hits norepinephrine harder, which can sometimes make sleep worse.
On the flip side:
- Mirtazapine (Remeron): Works like a sleep aid. It helps people fall asleep faster and stay asleep longer. In one study, users gained 53 extra minutes of sleep per night. But at doses above 30 mg, daytime sleepiness becomes a real problem.
- Trazodone: Originally an antidepressant, now mostly used as a sleep aid. At 25-50 mg, it helps people fall asleep without the grogginess of stronger sedatives. But at higher doses, it can cause dizziness, dry mouth, and next-day fog.
- Agomelatine: Not available in the U.S., but widely used elsewhere. It works on melatonin receptors to reset your body clock. In trials, it improved sleep quality without suppressing REM sleep-unlike SSRIs.
Timing Matters More Than You Think
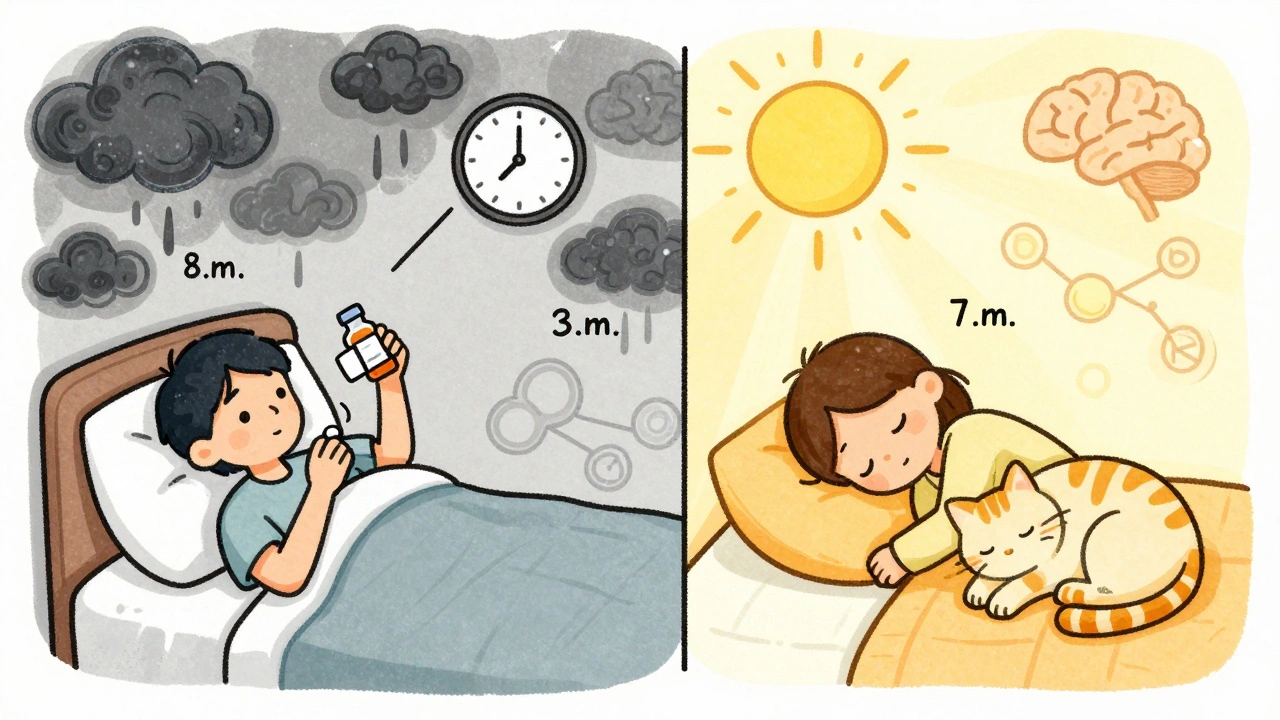
It’s not just about which drug you take-it’s when you take it.Take an SSRI in the evening? You’re asking for trouble. A 2020 study found that taking SSRIs before 9 a.m. reduced insomnia risk by 41%. That’s because these drugs stimulate the brain. If you take them later in the day, your nervous system doesn’t have time to wind down.
On the other hand, sedating antidepressants like trazodone or mirtazapine should be taken 2-3 hours before bed. Taking them too close to bedtime can make you feel groggy or disoriented when you wake up. Some people find that taking trazodone at 8 p.m. instead of 10 p.m. cuts down on morning fog.
And here’s something most people don’t know: some users report better sleep by splitting their SSRI dose. Half in the morning, half in the early afternoon. It’s not officially recommended yet, but a clinical trial at the University of Michigan is testing this exact approach. Early reports from Reddit users suggest it helps reduce nighttime wakefulness without losing the antidepressant effect.
What to Do If You’re Losing Sleep
If you started an antidepressant and now you’re lying awake at 2 a.m., here’s what actually works:- Wait it out (sometimes). For many, sleep problems peak around days 3-7 and improve by week 3. The 2005 Riemann review showed this pattern clearly. If your insomnia is mild, give it a few weeks before deciding the drug isn’t right.
- Change the timing. Move your SSRI to the morning. If you’re on a sedating drug, take it earlier in the evening.
- Track your sleep. Keep a simple sleep diary for two weeks. Note when you go to bed, when you wake up, how long it took to fall asleep, and if you woke up during the night. This helps your doctor spot patterns.
- Don’t combine bupropion with SSRIs. Over 120 Reddit users reported severe insomnia when mixing these two. The FDA issued a warning in 2022-this combo increases insomnia risk by 2.4 times.
- Ask about switching. If you have insomnia-predominant depression (which affects 70-75% of people with depression), mirtazapine or trazodone might be better first-line choices than an SSRI.
When to Worry About More Serious Sleep Problems
Most sleep changes are temporary. But some signals mean you need to talk to your doctor right away:- Acting out dreams-kicking, yelling, punching while asleep. This could be REM sleep behavior disorder (RBD), which is more common in people on SSRIs. The Cleveland Clinic found 68% of SSRI users showed signs of RBD on sleep studies.
- Uncontrollable leg movements at night. Restless legs syndrome (RLS) can be triggered or worsened by SSRIs. The International Restless Legs Syndrome Study Group says 65% of SSRIs can make it worse.
- Extreme daytime sleepiness that doesn’t improve after 4-6 weeks. If you’re nodding off at work or driving, your dose may be too high-or the drug isn’t right for you.
If any of these happen, ask for a sleep study. Polysomnography isn’t routine, but it’s worth it if your sleep is truly broken.
The New Way Forward: Matching Sleep Profile to Medication
The old approach was: pick an antidepressant, deal with side effects, hope things get better. The new approach is smarter.Doctors are starting to match antidepressants to your sleep pattern. If you sleep too much and feel heavy, an SSRI might help. If you can’t fall asleep and your mind races, start with mirtazapine or trazodone.
The 2023 Canadian guidelines now recommend mirtazapine 7.5-15 mg at bedtime for depression with insomnia. Why? Because it improves sleep efficiency by 32% and has a bigger effect on sleep than SSRIs do. In one study, mirtazapine had a 0.8 effect size for sleep improvement-SSRIs were only 0.3.
And it’s not just doctors. The FDA now requires all new antidepressants to include REM sleep data in their applications. The $18.7 billion antidepressant market is shifting. Companies like Organon are launching drugs like zuranolone (Zurzuvae), approved in 2023 specifically for rapid sleep improvement.
Even genetic testing is entering the picture. Genomind’s 2025 test analyzes 17 genes linked to sleep regulation and predicts how you’ll respond to 24 antidepressants. It’s not perfect-but it’s a step toward personalization.
What Works Best Right Now?
Here’s a simple guide based on your sleep problem:| Sleep Problem | Best First Choice | Why |
|---|---|---|
| Can’t fall asleep, racing thoughts | Mirtazapine 7.5-15 mg at bedtime | Increases total sleep time, improves sleep efficiency |
| Wake up often, can’t stay asleep | Trazodone 25-50 mg at bedtime | Reduces nighttime wakefulness, minimal next-day grogginess |
| Sleep too much, feel sluggish | SSRI (sertraline or escitalopram) in the morning | Helps with hypersomnia, less likely to cause insomnia than fluoxetine |
| Depression + vivid dreams or acting out dreams | Agomelatine (if available) or avoid SSRIs | Preserves REM sleep, lowers RBD risk |
| Need energy, not sedation | Bupropion alone (not with SSRIs) | Boosts alertness, no sedation-but avoid if insomnia is already a problem |
Remember: no single drug is perfect. But knowing how each one affects sleep lets you make smarter choices-and avoid months of sleepless nights.
What’s Coming Next
The future of antidepressant treatment isn’t just about mood. It’s about sleep. Researchers at MIT are building AI models that analyze over 2,000 sleep parameters to predict which antidepressant will work best for you-based on your sleep patterns, not just your symptoms. The National Institute of Mental Health is funding $14.3 million for this kind of research through 2026.One thing’s clear: if you’re struggling with sleep on antidepressants, you’re not alone. And you don’t have to just endure it. There are better ways to choose, time, and adjust these medications so they help you sleep-not hurt you.
Do all antidepressants cause insomnia?
No. While SSRIs like fluoxetine and sertraline commonly cause insomnia-especially in the first few weeks-other antidepressants like mirtazapine and trazodone are actually prescribed to improve sleep. The effect depends on the drug’s chemical profile. Mirtazapine increases total sleep time by nearly an hour on average, while fluoxetine can reduce REM sleep by up to 29% and make falling asleep harder.
How long does antidepressant-induced insomnia last?
For most people, insomnia from SSRIs peaks between days 3 and 7 and starts improving after 2-3 weeks. A 2005 study found that sleep disturbances typically resolve by week 4. But if it hasn’t improved by 6 weeks, it’s unlikely to get better on its own-and you should talk to your doctor about switching or adjusting your medication.
Can I take a sleep aid with my antidepressant?
Yes, but carefully. Trazodone is often used at low doses (25-50 mg) as a sleep aid alongside SSRIs. Melatonin or magnesium may help with sleep onset. But avoid combining sedating sleep aids like benzodiazepines or diphenhydramine with antidepressants unless your doctor approves it. Some combinations can increase dizziness, confusion, or next-day grogginess.
Why does my doctor say to take my SSRI in the morning?
SSRIs increase serotonin and norepinephrine, which are wakefulness-promoting chemicals. Taking them in the evening can delay sleep onset and cause nighttime wakefulness. A 2020 study found that taking SSRIs before 9 a.m. reduced insomnia risk by 41%. Morning dosing gives your body time to process the stimulation before bedtime.
Is mirtazapine better than an SSRI for sleep?
For people with insomnia-predominant depression, yes. Mirtazapine improves sleep efficiency by 32% and adds 47-53 minutes of sleep per night. In head-to-head trials, its effect on sleep is nearly three times stronger than SSRIs. But it can cause daytime drowsiness, especially at doses above 30 mg. If you need to stay alert during the day, your doctor might choose a different option.
Can antidepressants cause sleepwalking or acting out dreams?
Yes. SSRIs are linked to REM sleep behavior disorder (RBD), where people physically act out their dreams. The Cleveland Clinic found that 68% of SSRI users showed signs of RBD on sleep studies, compared to 22% of non-users. If you or your partner notice kicking, yelling, or punching during sleep, tell your doctor. This isn’t normal-it may require switching medications or a sleep study.
What should I do if my antidepressant makes me too sleepy?
If you’re excessively drowsy during the day, your dose may be too high-or the drug isn’t right for you. For mirtazapine, reducing the dose from 30 mg to 15 mg often cuts daytime sleepiness without losing sleep benefits. For trazodone, lowering the dose from 100 mg to 50 mg can help. Never stop abruptly. Talk to your doctor about adjusting timing or switching to a less sedating option like sertraline or bupropion.





Ruth Witte
December 8, 2025 AT 21:11 PMOMG YES. I was on sertraline and thought I was going crazy at 3 a.m. every night 😵💫 Then I switched to morning doses and my brain finally stopped throwing rave parties. Thank you for this guide!
Noah Raines
December 10, 2025 AT 19:56 PMBupropion + SSRI = sleep apocalypse. I learned that the hard way. Now I just take Wellbutrin alone and sleep like a log... if you ignore the 2 a.m. anxiety spikes. Still better than tossing and turning from Prozac.
Gilbert Lacasandile
December 12, 2025 AT 09:53 AMThis is actually super helpful. I've been on mirtazapine for 6 weeks now and I didn't realize how much better my sleep was until I read this. I used to count sheep, now I just... fall asleep. Weird how that works.
Lola Bchoudi
December 12, 2025 AT 21:24 PMFrom a clinical psych standpoint, the REM suppression metric is critical for treatment adherence. SSRIs induce a dose-dependent REM latency shift, which correlates with HAM-D reduction-but at the cost of sleep architecture fragmentation. For patients with comorbid insomnia-predominant MDD, mirtazapine’s 5-HT2A/2C antagonism and H1 histaminergic blockade provide superior sleep efficiency (SEI >85%) without pharmacodynamic antagonism. Don't just titrate-match the pharmacophore to the phenotype.
Morgan Tait
December 13, 2025 AT 13:24 PMYou know what they’re not telling you? Big Pharma knows SSRIs make people sleepless so they sell you melatonin supplements and sleep apps. It’s a cash grab. They don’t want you switching to agomelatine because it’s cheap and not patented. The FDA’s ‘REM data requirement’? Just PR spin. Wake up.
Christian Landry
December 14, 2025 AT 19:46 PMi took trazodone for like 2 weeks and woke up like a zombie. like... i couldnt even make coffee. switched to 25mg and now im fine. also why is everyone on here saying "morning ssri" like its magic? mine still kept me up at 8am lol
Katie Harrison
December 15, 2025 AT 00:56 AMI appreciate the detailed breakdown. But I have to say: the fact that we’re now relying on genetic tests to choose antidepressants... it’s a little overwhelming. I just want to feel normal. Not be a data point in a $18.7 billion algorithm.
Michael Robinson
December 16, 2025 AT 05:38 AMSleep is the foundation. If your brain can’t rest, nothing else matters. Medication helps the mind, but rest heals the body. Sometimes the simplest thing is the hardest to do: go to bed, turn off the screen, let go.