When a patient is stable on a brand-name NTI drug like warfarin, levothyroxine, or phenytoin, switching to a generic version isn’t just a paperwork change-it’s a clinical moment. These aren’t ordinary medications. A tiny shift in blood levels can mean the difference between control and crisis. That’s why patient communication when switching NTI generics isn’t optional. It’s essential.
Why NTI Drugs Are Different
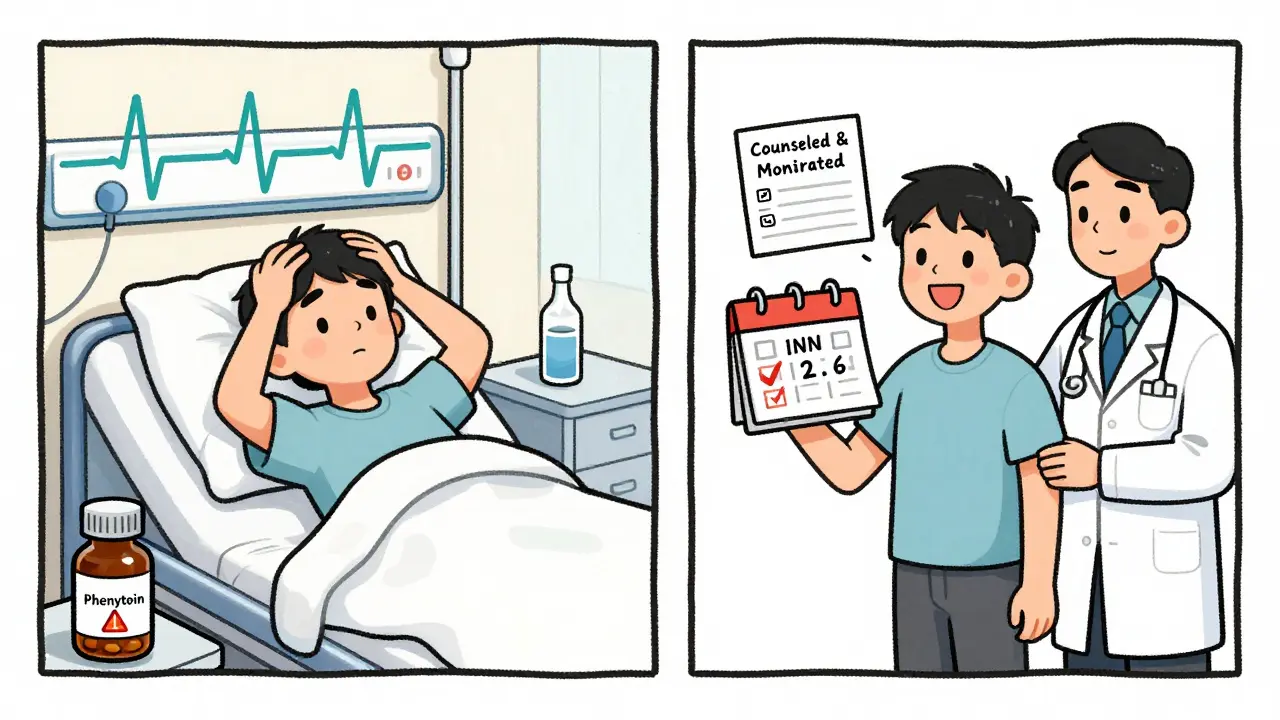
Narrow Therapeutic Index (NTI) drugs have almost no room for error. Their effective dose is barely below the toxic dose. For example, warfarin’s target INR range is 2-3. Go above 3, and you risk bleeding. Drop below 2, and you risk a stroke. Levothyroxine? A 10% change in absorption can throw a thyroid patient into hypothyroidism or hyperthyroidism. Digoxin? Too little won’t control heart rhythm. Too much can cause fatal arrhythmias. The FDA treats these drugs differently. While most generics just need to match the brand within 80-125% of blood concentration, NTI generics must stay within 90-111.11%. That’s tighter. And for some, like levothyroxine, the standard is even stricter: 95-105% for overall exposure (AUC). These aren’t arbitrary numbers. They’re based on real patient data showing what’s safe.Patients Are Confused-And That’s Not Their Fault
A 2017 survey found that 94% of pharmacists believed generic NTI drugs were safe. But only 60% consistently substituted them. Why? Because patients were asking questions. And many providers didn’t have clear answers. Patients hear things like: “This is cheaper,” “It’s the same,” or worse, “The brand didn’t work for me, so try this.” They don’t know what NTI means. They don’t know that switching from one generic to another can also cause problems. And if they’ve had a bad experience-maybe a seizure returned or their INR spiked-they’re not going to trust the next switch. The truth? Most generic NTI drugs are bioequivalent. But “most” isn’t enough when lives are on the line. That’s why communication has to be clear, consistent, and patient-centered.What to Say-And What Not to Say
Avoid: “It’s just a generic.” That sounds dismissive. It implies the drug is second-rate. Instead, say: “This generic version has been tested to deliver the same amount of medicine into your bloodstream as the brand version. For your specific medication, we’ll check your blood levels in one week to make sure everything is working correctly.” This works because it’s factual, specific, and proactive. You’re not just telling them it’s safe-you’re showing them you’re watching out for them. Another effective phrase: “I recommend this generic for you. It contains the exact same medicine, it has been proven to work just as well, and I prescribe it for my own family.” That personal touch builds trust. People don’t just believe facts-they believe people they trust.Monitoring Isn’t Optional-It’s the Standard
Switching NTI drugs isn’t a one-time conversation. It’s the start of a monitoring plan. For warfarin: Check INR within 3-5 days after the switch. The American Heart Association says so. For antiepileptics like phenytoin or carbamazepine: Get a serum level within 7-10 days. The American Epilepsy Society recommends it. Don’t assume the patient will show up. Schedule the test. Call them. Send a reminder. Use your EHR to flag the follow-up. A 2020 study showed patients who got personalized counseling had 28% fewer medication-related problems. That’s not just good care-it’s preventable harm avoided.State Laws Vary-And They Matter
In 27 states, there are special rules for NTI drug substitution. Fourteen of them require written patient consent before switching. That means you can’t just swap the pill bottle. You need a signed form. Some states allow substitution only if the prescriber checks “dispense as written.” Others require the pharmacist to notify the prescriber. You can’t rely on federal rules alone. Check your state’s pharmacy board website. Keep a printed copy in your office. If you’re unsure, ask the pharmacist before dispensing.Who Needs Extra Care?
Not all patients are the same. Certain groups are more vulnerable:- Patients over 65-slower metabolism, more drug interactions
- Those with kidney or liver problems-can’t clear the drug the same way
- People on five or more medications-higher risk of interactions
- Patients with poor health literacy-may not understand instructions
What About the Pharmacist?
You’re not alone in this. Pharmacists are on the front lines. They’re the ones handing over the new bottle. The American Pharmacists Association now recommends a minimum 10-minute counseling session for any NTI drug switch. That includes:- Verifying the patient understands the change
- Demonstrating how to take the medication (e.g., levothyroxine on empty stomach)
- Using teach-back: “Can you tell me what you’ll do differently now?”
What If Something Goes Wrong?
Even with perfect communication, things can happen. Between 2019 and 2023, the FDA received 1,247 reports of possible adverse events linked to NTI drug switches. Most involved antiepileptics or blood thinners. But in only 17% of cases was the switch confirmed as the cause. That doesn’t mean you ignore the reports. It means you document everything. If a patient reports a change in symptoms after a switch:- Check the drug name and manufacturer on the bottle
- Order the relevant lab test immediately
- Document the conversation: “Patient switched from brand to generic [drug] on [date]. Reported [symptom]. INR increased from 2.4 to 3.8.”
- Report to MedWatch if you suspect the switch contributed to harm
The Bigger Picture
Generic NTI drugs make up only 3.2% of all generic approvals-but they cause 11.7% of patient questions. Why? Because people are scared. And fear doesn’t go away with a label that says “generic.” The FDA’s 2024 NTI Drug Communication Initiative now offers patient materials in 12 languages. They’ve created counseling checklists for 15 high-priority drugs. They’re even planning to use real-world data from 12 million patients to track outcomes after switches. But none of that matters if you don’t talk to your patients. No database replaces a human conversation. No algorithm replaces trust. The goal isn’t just to switch the drug. It’s to keep the patient safe, informed, and confident. That’s how you turn a routine refill into a meaningful moment of care.Can I switch my patient from one generic NTI drug to another?
Yes, but only with caution. Even two different generic versions of the same NTI drug can have slightly different absorption rates. If a patient is stable on one generic, switching to another should be treated like switching from brand to generic. Monitor closely-check blood levels within 7-10 days and watch for any change in symptoms. Always document the change and the reason for it.
Do I need to get patient consent before switching an NTI drug?
It depends on your state. Fourteen states require written patient consent before substituting an NTI drug. In others, verbal counseling is enough-but you still need to document it. Check your state’s pharmacy board website or ask your pharmacist. Never assume federal rules override state law. When in doubt, get consent.
What if my patient refuses the generic?
Respect their choice. Some patients have had bad experiences, or simply don’t trust generics. You can explain the evidence, but forcing a switch can damage trust. Instead, ask: “What are your concerns?” Then address them directly. If they still refuse, write “dispense as written” on the prescription. You can revisit the conversation later, especially if cost becomes a barrier.
Which NTI drugs are most commonly switched?
The top five are warfarin, levothyroxine, phenytoin, carbamazepine, and digoxin. These are the drugs with the most documented cases of adverse events after substitution. The FDA has specific bioequivalence guidelines for each. Always check the product-specific guidance before switching.
How do I know if a generic is approved for an NTI drug?
Look up the drug in the FDA’s Orange Book. It lists all approved generics and their therapeutic equivalence codes. For NTI drugs, you’ll see an “A” code followed by “B” or “C.” An “AB1” code means it’s therapeutically equivalent and meets NTI standards. Avoid generics with “BX” codes-they haven’t been fully evaluated for NTI drugs.
Is it safe to switch elderly patients to generic NTI drugs?
Yes, but extra care is needed. Older adults metabolize drugs slower and often take multiple medications, increasing interaction risks. Always start with the lowest dose, monitor closely, and involve the pharmacist. Use visual aids and teach-back to confirm understanding. If the patient is stable on brand, consider keeping them on it unless cost or access forces a change.
What’s the best way to document an NTI drug switch?
Use this template: “Patient counseled on therapeutic equivalence of generic [drug name] to brand version. Advised of need for [specific test] within [timeframe]. Provided written materials. Patient verbalized understanding.” Include the date, the pharmacist’s name, and any follow-up scheduled. This protects you and ensures continuity of care.
Next Steps for Providers
Start today. Don’t wait for a patient to ask. Build a simple protocol:- Identify all patients on NTI drugs in your practice.
- Review their current medication-brand or generic?
- Check your state’s substitution laws.
- Create a one-page handout for patients explaining NTI drugs and what to expect after a switch.
- Set up automated alerts in your EHR for post-switch lab checks.
- Ask your pharmacy partner if they use visual aids and teach-back.







Kacey Yates
January 29, 2026 AT 01:47 AMGeneric NTI drugs are fine if you actually monitor patients like the article says but everyone skips the monitoring because it's a hassle and insurance won't pay for it so patients get screwed and then we wonder why med errors go up
ryan Sifontes
January 30, 2026 AT 23:11 PMlol at the 10-minute pharmacist counseling. good luck with that when they're doing 60 scripts an hour and the line is out the door
Laura Arnal
February 1, 2026 AT 00:59 AMThis is so important!! 🙌 I've seen patients panic when their pill changes color and it's not their fault - we just don't explain it right. Visuals + teach-back = game changer. 💊❤️
Jasneet Minhas
February 1, 2026 AT 02:17 AMHow ironic that in India we pay 10x more for brand-name levothyroxine while Americans argue about generics. Capitalism is a beautiful thing 😏
Eli In
February 1, 2026 AT 23:38 PMI love how this article treats patients like humans instead of compliance metrics. We need more of this. 🌍✨
Megan Brooks
February 2, 2026 AT 05:58 AMThe ethical imperative here transcends clinical guidelines. When we reduce patient autonomy in the name of cost-efficiency, we erode the foundational trust of the healer-patient relationship. Documentation is not merely administrative-it is moral witness.
Sheryl Dhlamini
February 3, 2026 AT 05:53 AMI've been on the same generic warfarin for 5 years. Never had an issue. But I know someone who had a bleed after switching. So I guess we just... keep doing the same thing and hope?
Doug Gray
February 4, 2026 AT 14:17 PMIt's not the bioequivalence that's the issue-it's the ontological insecurity of the pharmaceutical-industrial complex. We're projecting epistemic anxiety onto pill formulations because we've outsourced meaning to patent law.
Pawan Kumar
February 6, 2026 AT 07:15 AMOne must question the scientific rigor behind these so-called "NTI" thresholds. The FDA's 90-111.11% range is statistically arbitrary, derived from cherry-picked cohorts with inadequate power. Real-world pharmacokinetic variability in diverse populations is systematically ignored. This is not medicine-it is regulatory theater dressed in pseudoscientific garb.
Furthermore, the insistence on patient consent reflects a profound misunderstanding of medical paternalism. If a physician deems a substitution clinically appropriate, the patient's emotional resistance is irrelevant. Their fear is not data. Their anecdotal "bad experience" is not evidence. We are not here to coddle ignorance-we are here to correct it.
And yet, the article recommends visual aids and teach-back? How quaint. In my practice, we use standardized lab protocols and automated EHR alerts. The patient's comprehension is irrelevant if the system is robust. If they can't follow instructions, perhaps they shouldn't be managing their own anticoagulation.
The notion that "trust" is the outcome of a 10-minute pharmacist conversation is delusional. Trust is earned through consistency, not scripted phrases. And let us not forget: the brand-name manufacturers spent billions lobbying to create this myth of superiority. The real villain is not the pharmacist-it is the pharmaceutical marketing machine.
Why are we still debating this in 2025? We have real-time therapeutic drug monitoring. We have AI-driven predictive analytics for INR fluctuations. We have blockchain-enabled supply chains. Yet we cling to paper consent forms and printed handouts like relics of a pre-digital age.
And don't get me started on the "12 languages" initiative. Translation is not cultural competence. You cannot translate epistemology. A Gujarati-speaking patient in rural Rajasthan does not need a pamphlet-he needs a functional healthcare system.
The entire discourse is performative. We are not solving a clinical problem. We are performing virtue signaling to appease liability insurers and regulatory bodies. The real solution? Ban generic substitution for NTI drugs entirely. Let the market decide. If patients want the brand, they pay for it. If they want the generic, they accept the risk. No counseling. No forms. No hand-holding. Just medicine.
And if someone has a bleed? Well, that's what malpractice insurance is for.
LOUIS YOUANES
February 7, 2026 AT 12:55 PMThey're just trying to sell you cheaper pills. Same as always. You think they care if you have a stroke? Nah. They care about their quarterly earnings.
Laia Freeman
February 7, 2026 AT 18:04 PMOMG YES!!! I just switched my mom to generic levothyroxine and she was FREAKING OUT because the pill looked different-so I printed out a chart with the pill pics and we did the teach-back thing and now she’s chill 😌💕 #PatientEmpowerment
rajaneesh s rajan
February 8, 2026 AT 18:08 PMSo we're supposed to trust a system that lets one generic be made in China and another in India, both labeled the same, but who knows what's really inside? Meanwhile, the FDA just smiles and says "AB1" like it's a magic spell. 🤷♂️