Imagine your body absorbing way too much iron-so much that it starts eating away at your liver, heart, and pancreas. This isn’t science fiction. It’s hemochromatosis, a silent genetic disorder that affects about 1 in 200 people of Northern European descent. Most don’t know they have it until their organs are already damaged. And the scary part? It’s completely treatable-if caught early.
What Is Hemochromatosis, Really?
How Iron Builds Up Without You Even Knowing
Normally, your body absorbs just enough iron from food to replace what you lose through blood loss, sweat, or shedding skin cells. But in hemochromatosis, a broken gene-usually the HFE C282Y mutation-tells your gut to keep absorbing iron even when you have plenty. Over time, that extra iron piles up like rust in a pipe.
Men are far more likely to show symptoms than women, not because they’re more genetically prone, but because women lose iron naturally through menstruation. By the time women reach menopause, their risk catches up. Symptoms usually appear between ages 30 and 50. Early signs? Fatigue so bad it feels like you’re dragging through mud, joint pain in your knuckles (not your knees, not your back-your fingers), and a sudden loss of interest in sex. These aren’t signs of aging or stress. They’re red flags for iron overload.
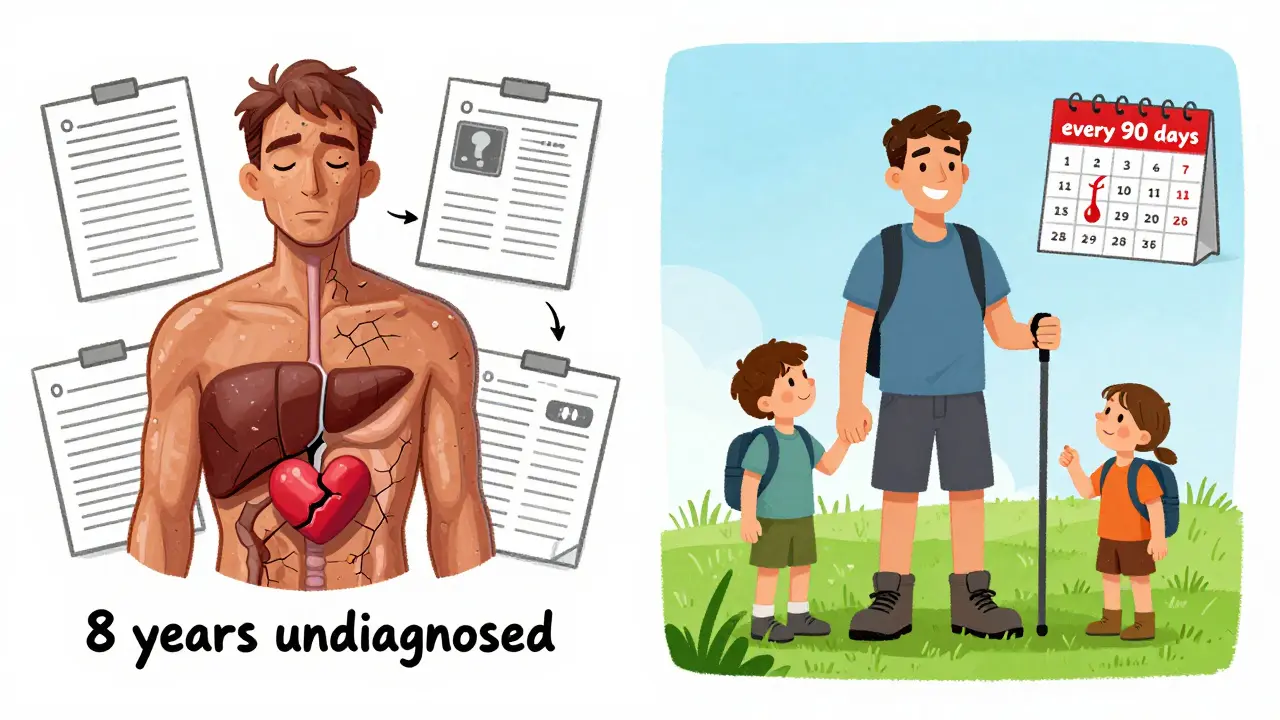
By the time skin turns bronze or gray, diabetes develops, or your liver starts failing, it’s already too late for simple fixes. That’s why so many people go years undiagnosed. One patient on Reddit spent eight years seeing doctors before his ferritin level hit 2,850 ng/mL-over ten times the normal range.
How Doctors Diagnose It
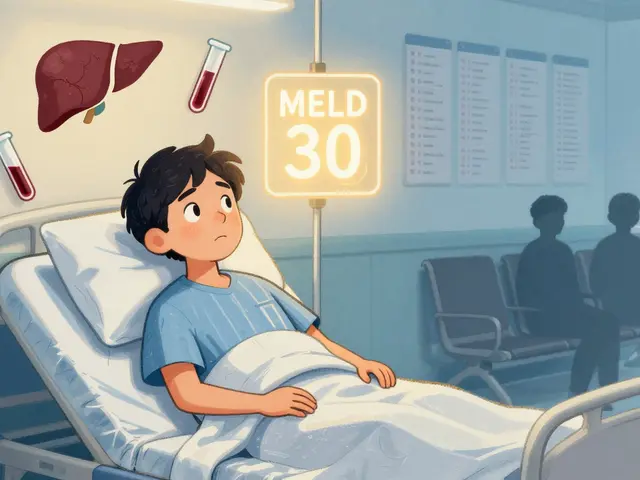
There’s no single test for hemochromatosis. It’s a two-step puzzle. First, blood tests. If your transferrin saturation is above 45% and your serum ferritin is over 300 ng/mL for men or 200 ng/mL for women, that’s a strong signal. Ferritin isn’t just a measure of iron-it’s your body’s iron storage tank. Normal levels are 30-400 ng/mL. But when it climbs past 1,000 ng/mL, your risk of cirrhosis jumps to 50-75%.
The second step is genetic testing. Over 90% of cases come from two copies of the C282Y mutation. Less common are compound mutations like C282Y/H63D, which cause milder iron buildup. Other types of hemochromatosis exist (Types 2, 3, 4), but they’re rare and often hit younger people. If you’re Caucasian and have unexplained fatigue, joint pain, or elevated liver enzymes, ask for these two tests. Most doctors won’t order them unless you push.
And yes, MRI scans now replace liver biopsies. The R2* technique measures iron in the liver without a needle. It’s accurate, safe, and covered by insurance. Biopsies? Only used now if the diagnosis is unclear or if cancer is suspected.

Phlebotomy: The Simple, Free, and Powerful Cure
There’s no pill for hemochromatosis. No magic drug. The treatment is as old as medicine itself: phlebotomy-removing blood.
Each time you donate 500 mL of blood, you lose about 200-250 mg of iron. Your body doesn’t make new red blood cells fast enough to replace the iron you’ve stored, so it starts pulling from your excess deposits. It’s like draining a flooded basement with a bucket.
Phase one: Induction. You get a blood draw every week until your ferritin drops to 50-100 ng/mL. For someone with ferritin over 2,000, that can take 12 to 18 months-sometimes 50+ sessions. It’s exhausting. But here’s the key: once you get there, your symptoms often vanish. Fatigue lifts. Joint pain fades. Libido returns.
Phase two: Maintenance. You don’t stop after the first year. You keep going-every 2 to 4 months-to stay in that 50-100 ng/mL sweet spot. Most people need 4-6 sessions a year. Insurance covers it. Blood centers often allow therapeutic donations (not just for charity). Some patients even get paid for donating because they’re medically required to.
Compared to iron-chelating drugs like deferasirox-which cost $25,000-$35,000 a year-phlebotomy costs $0 to $50 per session. And it’s proven: people who stick with it have near-normal life expectancy. Those who don’t? Their 10-year survival rate drops to 60% if cirrhosis has already set in.
What Happens If You Ignore It
Iron doesn’t just sit there. It oxidizes. It creates free radicals. It scars tissue. The liver takes the biggest hit. By the time cirrhosis develops, the damage is permanent. From there, liver cancer (hepatocellular carcinoma) becomes a real threat. One study showed that 75% of people with hemochromatosis and cirrhosis died within 10 years without treatment.
But it doesn’t stop at the liver. Iron builds up in the pancreas and kills insulin-producing cells-leading to diabetes in 1 in 4 patients. It clogs the heart, causing arrhythmias and heart failure. It shuts down the pituitary gland, leading to low testosterone and infertility. In men, this often shows up as erectile dysfunction or shrinking testicles.
And here’s the cruel twist: once you feel better after a few phlebotomies, you might think you’re cured. You stop. That’s when the iron creeps back. Symptoms return. Organs start failing again. Treatment isn’t a cure-it’s a lifelong maintenance plan.
Who Should Get Tested
You don’t need to wait for symptoms. If you have:
- A parent, sibling, or child with hemochromatosis
- Unexplained fatigue, joint pain, or liver enzyme spikes
- Diabetes with no clear cause (not overweight, no family history)
- Heart problems without high cholesterol or hypertension
- Darkened skin that doesn’t fade with sun exposure
Then get tested. Family screening is the most effective way to catch it early. If one person in a family is diagnosed, all first-degree relatives should be tested. The genetic test costs $150-$300 now-down from over $1,000 in 2000. It’s one of the cheapest, most life-saving tests in medicine.
What Doesn’t Work
Some people try to manage it with diet. Avoid red meat? Cut back on iron supplements? That’s helpful-but not enough. Your body still absorbs too much iron from vegetables, grains, and even water. You can’t diet your way out of a genetic defect.
Antioxidants like vitamin C? They actually increase iron absorption. Avoid them right before meals. And don’t drink alcohol. It speeds up liver damage. Even moderate drinking can push someone with hemochromatosis into cirrhosis faster.
And don’t rely on your doctor to spot it. Only 12% of primary care doctors routinely check transferrin saturation for fatigue or joint pain. You have to ask. Say: ‘I think I might have hemochromatosis. Can you order a ferritin and transferrin saturation test?’
What’s Next for Treatment
Researchers are working on drugs that mimic hepcidin-the hormone your body stops making in hemochromatosis. One experimental drug, PTG-300, showed a 53% drop in transferrin saturation in just 12 weeks. It could one day replace phlebotomy. But it’s still in trials. For now, blood removal is the only proven, safe, and effective method.
Meanwhile, genetic testing is getting smarter. Scientists are now using 27 genetic markers beyond HFE to predict who will develop severe iron overload. This helps identify people who carry the mutation but won’t get sick-saving them from unnecessary treatment.
Living With It
People with hemochromatosis live full, normal lives-if they stick to treatment. One patient I spoke to had his first phlebotomy at age 42. His ferritin was 3,200. He had joint pain so bad he couldn’t hold his grandkids. After 18 months of weekly blood draws, he was back to hiking, gardening, and playing with his grandchildren. He now gets blood drawn every 90 days. He says it’s the best thing he ever did.
The hardest part isn’t the blood draws. It’s the loneliness. Most people don’t understand. Your doctor might shrug. Your friends might think you’re overreacting. But this isn’t a lifestyle choice. It’s a genetic condition that, if ignored, kills. And if treated? It doesn’t touch your life expectancy.
Don’t wait for symptoms. Don’t wait for a crisis. If you’re of Northern European descent and have unexplained fatigue or joint pain-get tested. It takes five minutes. It costs less than a coffee. And it might save your liver, your heart, your life.





Janette Martens
December 29, 2025 AT 00:28 AMi just found out my dad had this and never told anyone... he died of liver failure at 58. why the hell did no one test him? we’re canadian and he never even got a proper diagnosis. so much for our "great" healthcare system. #ripdad
Marie-Pierre Gonzalez
December 29, 2025 AT 11:06 AMThank you for sharing this vital information with such clarity. I am deeply moved by your dedication to raising awareness. This condition is tragically underdiagnosed, and your post may very well save lives. I shall share it with my entire family immediately. 🙏
Louis Paré
December 31, 2025 AT 10:07 AMPhlebotomy is the cure? Wow. So the solution to a genetic disorder is just... bleeding people? That’s not medicine, that’s medieval. And you call this science? The real cure is gene editing. We’re still using buckets when we could be rewriting DNA. Lazy.
Julius Hader
January 2, 2026 AT 07:25 AMI’ve been doing therapeutic donations for 7 years now. Ferritin was 2,900 when I started. Now I’m at 85. I can lift my kids again. No drugs. No side effects. Just blood. It’s wild how simple it is when you know what to ask for.
Vu L
January 3, 2026 AT 08:03 AMLmao so we’re supposed to just bleed ourselves to stay alive? Sounds like a cult. What if your iron’s high because you eat too much steak? Maybe stop eating meat instead of draining your blood like a vampire?
Mimi Bos
January 3, 2026 AT 09:08 AMi had this and didn’t know it. my doc just said "you’re tired because you’re stressed". took me 4 years and a random lab tech asking "why is your ferritin so high?" to figure it out. now i donate every 3 months and feel like a new person. don’t ignore fatigue.
Sydney Lee
January 4, 2026 AT 01:11 AMThe fact that we still rely on 19th-century phlebotomy in the 21st century is a testament to the stagnation of medical innovation. While the treatment is effective, it is fundamentally reactive, not proactive. We are managing symptoms rather than correcting the underlying regulatory failure in hepcidin signaling. This is not medicine-it is palliative caretaking with a side of blood loss.
oluwarotimi w alaka
January 5, 2026 AT 18:53 PMthis is a western scam. in africa we don’t get this because we don’t eat processed iron. they made this up so you’ll pay for blood draws and tests. they want you weak so you’ll take their pills. the real cause is GMO food and fluoride in the water. trust no one.
Debra Cagwin
January 7, 2026 AT 03:10 AMTo anyone reading this who’s been dismissed by their doctor: you are not overreacting. Your symptoms are real. Ask for ferritin and transferrin saturation. Bring this post with you. You deserve to be heard. I’ve walked this path with patients-your life doesn’t have to be defined by fatigue. You can thrive. I believe in you.
Hakim Bachiri
January 8, 2026 AT 14:49 PMI’ve been doing this for 12 years. 58 phlebotomies. My liver’s fine. My pancreas? Still working. My wife says I’m "less of a grump" now. But here’s the thing: they don’t tell you that after 5 years, your veins turn to Swiss cheese. You need a specialist. Not your GP. Not the blood bank guy. A hematologist. And don’t let them "schedule" you every 4 months-do it when you feel the fog coming back.
Celia McTighe
January 8, 2026 AT 20:06 PMI just got diagnosed after 8 years of being told "it’s just anxiety." I cried for 2 hours. Then I booked my first donation. I’m so grateful for people like you who put this out there. I’m not alone anymore 💕
Ryan Touhill
January 10, 2026 AT 12:39 PMThe irony is that this condition is most prevalent in populations that were once considered "superior" by eugenicists. Iron overload was an evolutionary advantage in times of famine. Now, in our overfed, overprocessed world, it’s a death sentence. The same genes that once ensured survival now doom us. It’s poetic. And tragic.
Teresa Marzo Lostalé
January 11, 2026 AT 12:59 PMMy mom got diagnosed after her second heart attack. She’s 67 now. Gets blood drawn every 90 days. Still gardens. Still dances. Still makes her famous chili. I used to think she was just "old." Turns out she was just full of rust. Now I get tested every year. No excuses.