When you pick up your prescription, you might be handed a pill that looks completely different from what you’ve taken before. The label says it’s the same medicine, but it’s cheaper-and you’re left wondering: Is this really going to work the same way?
They’re not different drugs. They’re the same drug, just cheaper.
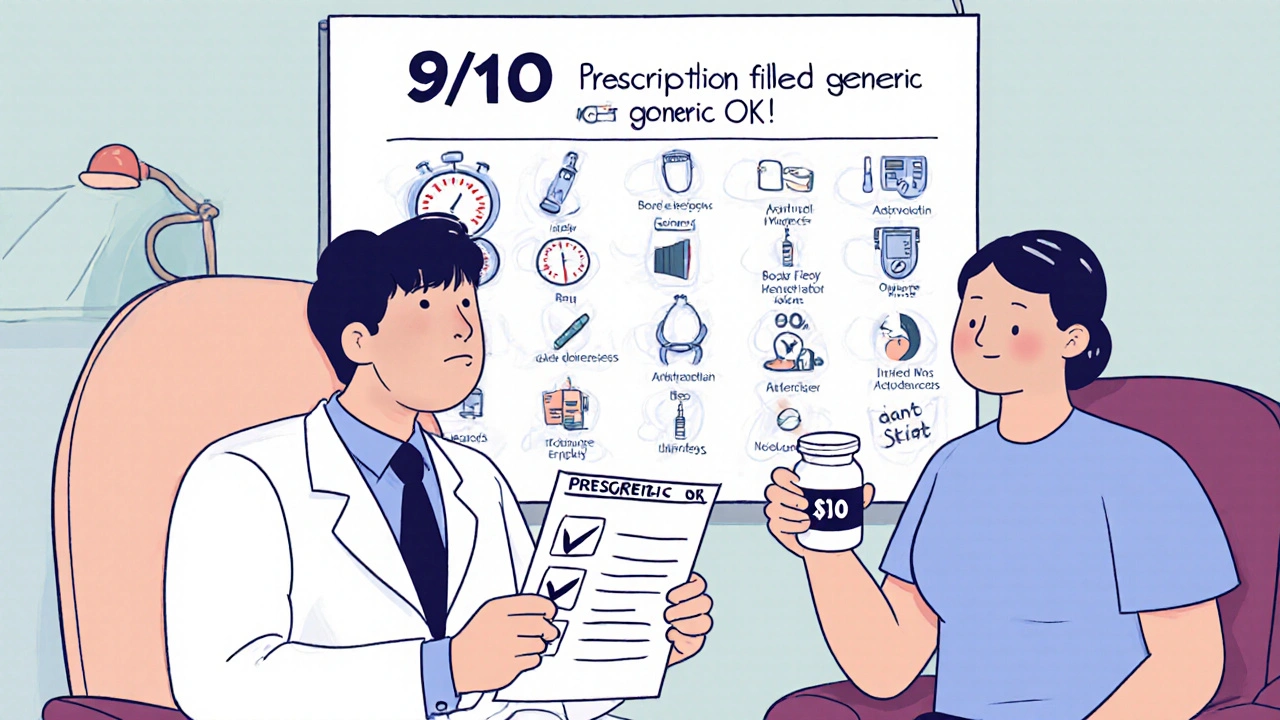
The FDA requires generic medications to contain the exact same active ingredient as the brand-name version. That means if you’re taking metformin for diabetes or lisinopril for high blood pressure, the generic version has the same chemical structure, works the same way in your body, and delivers the same clinical results. The only differences are in the color, shape, size, flavoring, or inactive ingredients like fillers and dyes. These changes are required by U.S. trademark laws so generics can’t look identical to the brand-name drug-but they don’t affect how the medicine works.Here’s the reality: 9 out of 10 prescriptions filled in the U.S. are for generics. And for good reason. Generics cost 80-85% less than brand-name drugs. Between 2007 and 2016, they saved the U.S. healthcare system over $1.67 trillion. On average, patients save $45 per prescription just by switching to generics. That’s not a small difference-it’s life-changing for people on fixed incomes or juggling multiple medications.
Why do some people say generics don’t work as well?
You’ve probably heard stories. Someone switched from brand-name Lamictal to the generic version and had a seizure. Or their cholesterol jumped after switching from Lipitor. These cases get talked about. But they’re rare-and often misunderstood.The FDA allows generics to vary by up to 20% in how quickly they’re absorbed into the bloodstream. In practice, the average difference is just 3.5%. That’s well within the safe range. For 99% of medications, this tiny variation makes no clinical difference.
There are exceptions. Some drugs have a narrow therapeutic index-meaning even a small change in blood levels can cause problems. These include warfarin (blood thinner), levothyroxine (thyroid hormone), and certain seizure medications like phenytoin. Even here, the FDA says approved generics are safe and effective. But some doctors, out of caution, may still prescribe the brand-name version.
More often than not, what people feel isn’t a pharmacological difference-it’s the nocebo effect. If you believe the cheaper version won’t work, your brain can convince you it doesn’t. A Kaiser Permanente study found that 17% of patients worried when they got a generic, but 92% were satisfied after a pharmacist explained what changed.
State laws force pharmacies to switch you-unless your doctor says no.
In most states, pharmacies are required by law to substitute a generic drug if one exists, unless your doctor writes “dispense as written” or “do not substitute” on the prescription. That means you might get a different pill without ever asking. You might not even notice until you see the price drop-or the pill looks different.That’s why it’s critical to talk to your doctor before you get to the pharmacy. Don’t wait for a surprise. Ask: “Is there a generic version of this?” and “Is it safe for me to use?”
If you’ve had a bad reaction to a generic in the past, say so. If you’re on a tight budget and can’t afford the brand-name drug, say that too. Your doctor isn’t just prescribing medicine-they’re helping you manage your health within real-world constraints.
What to ask your doctor before your next appointment.
You don’t need to be a medical expert to have this conversation. Here are three simple questions to ask:- Is there a generic version of this medication?
- Will it work just as well for my condition?
- Are there any reasons I should avoid the generic?
For most conditions-high blood pressure, depression, cholesterol, acid reflux, infections-the answer will be yes. Generics are just as effective. But if you’re on a complex medication like warfarin, your doctor might want to monitor your levels more closely after switching. That’s not because the generic is worse-it’s because your body needs precise control.
Also ask: “Can I try the generic first?” Many doctors will agree, especially if cost is a barrier. If you notice any changes after switching-new side effects, feeling different, symptoms returning-call your doctor. Don’t assume it’s nothing. But don’t assume it’s the generic’s fault either. Document what you’re feeling. That information helps your doctor decide whether to switch you back or adjust the dose.
Pharmacists are your secret weapon.
Your pharmacist knows more about your medications than you think. They see every prescription you fill, track interactions, and know which generics have had issues in the past. If you’re nervous about a switch, ask them: “Is this generic the same as the brand?”A 2022 study by the American Pharmacists Association found that 78% of patient concerns about generics were resolved after a simple conversation with a pharmacist. They can explain why the pill looks different, confirm it’s FDA-approved, and even check if your insurance requires a generic.
Don’t treat the pharmacy counter as a place to just grab your pills. Treat it like a free consultation.
Why do brand-name drugs still cost so much?
Even though generics make up 90% of prescriptions, they only account for about 25% of total drug spending. Why? Because brand-name drugs are priced 5 to 10 times higher. A 30-day supply of brand-name Lipitor might cost $300. The generic, atorvastatin, costs $10.Brand-name companies spend billions on research and marketing. Once the patent expires (usually 20 years after filing), other companies can make copies. But the original company doesn’t lower its price. Instead, they often push “new and improved” versions or bundle drugs together to keep you on the expensive option.
That’s why it’s so important to question why you’re being prescribed a brand-name drug. Is it because it’s better? Or because it’s what the rep pushed, or what the insurance plan favors?

What about biologics and biosimilars?
Not all drugs have generics. Biologics-like Humira, Enbrel, or insulin-are made from living cells, not chemicals. They’re complex, expensive, and can’t be copied exactly. Instead, there are biosimilars: highly similar versions that are cheaper but not identical.Biosimilars are not the same as generics. They’re a different category. Right now, only about 28% of biologic prescriptions use biosimilars, but that’s changing fast. As more biologics lose patent protection, biosimilars will become more common. Your doctor should be able to tell you if your drug is a biologic and whether a biosimilar is available.
When should you stick with the brand-name?
There are three real reasons to choose brand-name over generic:- You had a clear, documented reaction to a generic version in the past.
- Your doctor has a specific reason-like managing a narrow therapeutic index drug-and wants to avoid switching.
- You’re on a medication with no approved generic yet (like some newer cancer drugs).
That’s it. For everything else-diabetes, asthma, high cholesterol, anxiety, arthritis-generics are the smart, safe, proven choice.
What’s changing in 2025?
The FDA is approving more generics faster than ever. Thanks to the Generic Drug User Fee Amendments (GDUFA), approval times dropped from 36 months to just 10 months. In 2022 alone, the FDA approved 745 new generics-a 12% increase from 2021.More drugs are coming off patent. By 2027, generics could save the U.S. healthcare system another $1.48 trillion. But there’s a risk: supply chain issues. Nearly half of all generic shortages in recent years came from single manufacturing sites overseas. That’s why your doctor might occasionally switch you between generic brands-it’s not because one is better. It’s because the other one ran out.
Bottom line: Generics aren’t second-rate. They’re the standard.
You’re not saving money by choosing a brand-name drug. You’re paying extra for packaging, advertising, and brand recognition. The medicine inside? Identical.
Next time you get a prescription, ask: “Is there a generic?” If the answer is yes, and your doctor says it’s safe, take it. You’re not compromising your health. You’re making a smarter choice.






Russ Bergeman
November 20, 2025 AT 04:10 AMI switched to generic lisinopril and got a headache for three days. Coincidence? Maybe. But I'm not risking it again. 🤷♂️
Dana Oralkhan
November 20, 2025 AT 06:55 AMI used to be scared of generics too-until my pharmacist sat me down and showed me the FDA data. Turns out, my blood pressure didn’t care if the pill was blue or white. I’ve saved $200/month since. 🙌
Jeremy Samuel
November 20, 2025 AT 18:41 PMgenericz r cool n all but what if the filler has gluten? i got celiac and once got a pill that made me feel like i was run over by a truck. no one cares.
Destiny Annamaria
November 22, 2025 AT 04:58 AMMy grandma took generic metformin for 8 years and never missed a beat. She said, 'If it keeps my sugar down and doesn't cost me my groceries, why fight it?' 💪❤️
Ron and Gill Day
November 23, 2025 AT 03:45 AMLet’s be real-this whole 'generics are fine' narrative is corporate propaganda. Big Pharma doesn’t want you to know they’re just repackaging the same chemistry. And the FDA? They’re bought and paid for.
Aruna Urban Planner
November 24, 2025 AT 11:35 AMThe pharmacokinetic variance in generics is statistically negligible for most agents, but in populations with polypharmacy or renal impairment, even minor deviations can cascade into clinical instability. Monitoring is not paranoia-it’s precision medicine.
Nicole Ziegler
November 24, 2025 AT 21:39 PMI switched to generic Adderall and felt like a zombie for a week 😵💫… then realized I’d been sleeping 4 hours a night. The pill didn’t change. My life did. 🤓
Bharat Alasandi
November 26, 2025 AT 10:50 AMBro, I took generic simvastatin for 2 years, my LDL dropped, no side effects, and I paid $5 instead of $300. Why would anyone pay extra unless they’re rich or brainwashed? 🤔
Kristi Bennardo
November 26, 2025 AT 17:00 PMThis article is dangerously misleading. People have died from generic substitutions. The FDA doesn’t test long-term effects. This isn’t science-it’s a marketing pamphlet for insurance companies.
Ravi boy
November 27, 2025 AT 21:55 PMi got generic warfarin last year and my inr went nuts. doc said its fine but i switched back to brand. now im stable. dont trust the system
Matthew Karrs
November 29, 2025 AT 14:21 PMYou know who benefits from generics? The Chinese and Indian manufacturers. The FDA doesn’t inspect most of those factories. Your ‘safe’ pill could be made in a basement with no quality control.
Matthew Peters
November 30, 2025 AT 09:26 AMI’ve been on 7 different generics for my antidepressants. Some worked fine. One made me cry in the shower for no reason. Another made me feel like a robot. The difference? Not chemistry. It’s your brain believing it should feel different. I stopped fighting it. Now I just track how I feel-not the pill’s color.