When your body can’t make enough of the hormones that keep you alive, everyday life becomes a balancing act. For people with Addison’s disease, this isn’t theoretical-it’s daily reality. Addison’s disease, or primary adrenal insufficiency, happens when the adrenal glands are damaged and can’t produce enough cortisol and aldosterone. These aren’t optional hormones. Cortisol manages stress, blood sugar, and inflammation. Aldosterone controls salt and water balance. Without them, your body starts shutting down. And if you don’t know what’s wrong, it can kill you.
What Actually Causes Addison’s Disease?
Most cases-80 to 90% in the UK and other developed countries-are caused by the immune system attacking the adrenal glands. It’s an autoimmune mistake: your body turns on itself. This usually shows up as antibodies against 21-hydroxylase, a key enzyme in hormone production. The damage builds slowly. You lose function until 90% of the adrenal cortex is gone before symptoms appear. That’s why most people are diagnosed only after they’re already in crisis. Decades ago, tuberculosis was the main cause. Today, it’s rare in places like the UK. But in parts of Africa and Asia, TB still accounts for over half of cases. Other rare causes include infections, cancer spreading to the adrenals, or genetic conditions. But if you’re in the UK, US, or Europe and you have adrenal insufficiency, it’s almost certainly autoimmune.How Do You Know You Have It?
Symptoms creep in quietly. Fatigue. Weight loss. Low blood pressure. Nausea. Cravings for salt. These get written off as stress, depression, or the flu. The average person waits over three years before getting the right diagnosis. Gastroenterologists and GPs are often the first to see them-because the symptoms look like digestive problems. But there are clues that point to Addison’s. Dark patches of skin, especially on knuckles, elbows, knees, and inside the mouth, are classic. That’s from high ACTH levels stimulating pigment cells. You might also have low sodium, high potassium, low blood sugar, and dizziness when standing up. These aren’t random. They’re the body screaming that it’s out of balance. The test that confirms it is the ACTH stimulation test. You get a shot of synthetic ACTH, then your cortisol is checked 30 to 60 minutes later. If your cortisol doesn’t jump above 18 mcg/dL, your adrenals aren’t responding. Blood tests will also show high ACTH and low aldosterone. If your ACTH is high but aldosterone is normal, it’s probably not Addison’s-it’s secondary insufficiency, which comes from the pituitary, not the adrenals.Steroid Replacement: The Lifesaving Routine
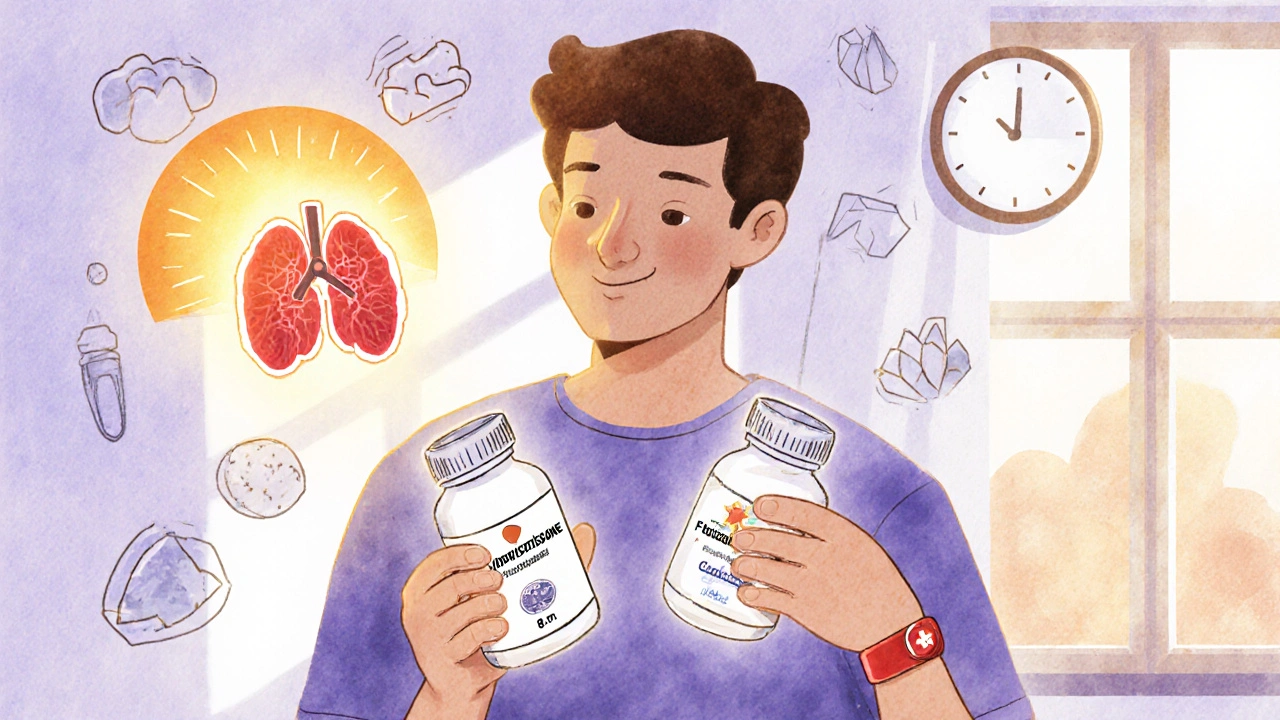
There’s no cure. But there is treatment: lifelong steroid replacement. You need two types. First, glucocorticoids-usually hydrocortisone. This replaces cortisol. Most people take 15 to 25 mg a day, split into two or three doses. The first dose is higher in the morning to mimic your body’s natural rhythm. You might take 10 mg at 8 a.m., 5 mg at noon, and 5 mg at 5 p.m. Some newer options, like Chronocort, are designed to release slowly and mimic natural patterns better, reducing spikes and crashes. Second, mineralocorticoids-fludrocortisone. This replaces aldosterone. You take 50 to 300 micrograms daily. It helps your kidneys hold onto salt and water. Without it, you get dangerously low blood pressure and high potassium. Your doctor will monitor your sodium, potassium, and blood pressure to adjust the dose. It’s not just about taking pills. It’s about knowing when to change them.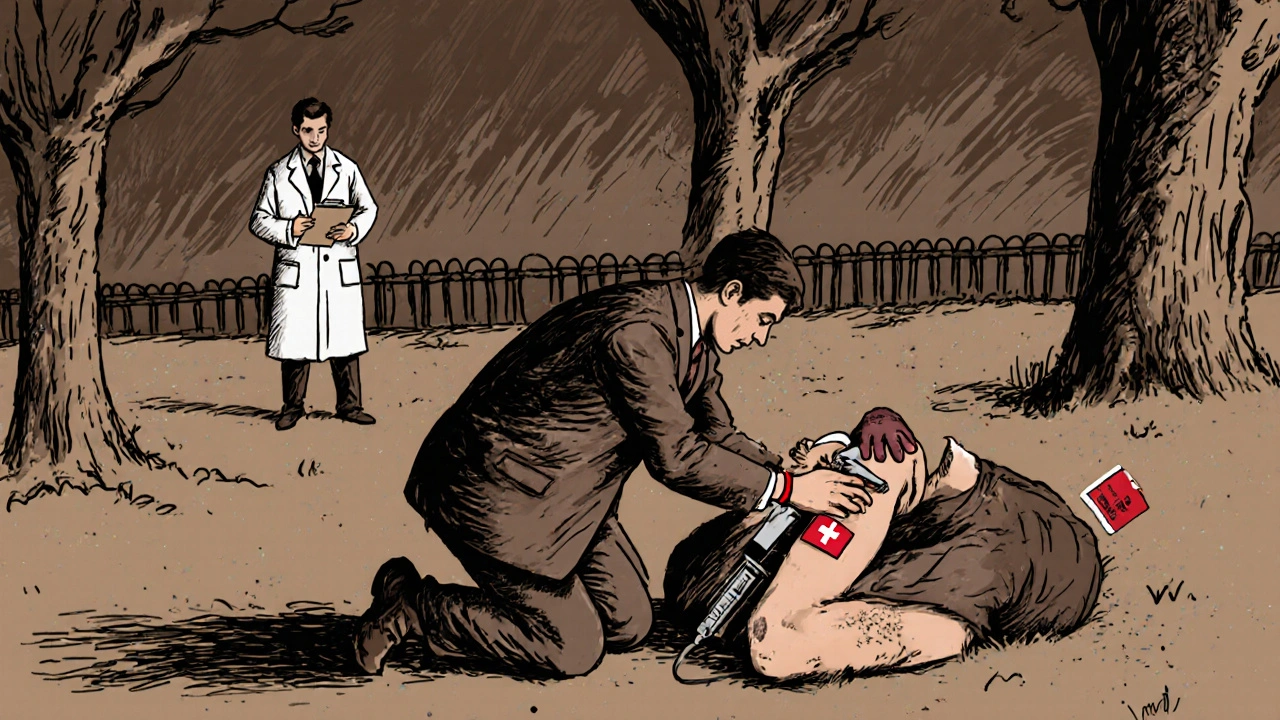
The Sick Day Rules: When Illness Becomes a Crisis
The biggest danger isn’t missing a dose on a normal day. It’s missing it when you’re sick. Infection, vomiting, surgery, even a bad cold-these can trigger adrenal crisis. Your body needs up to three times more cortisol just to cope. If you don’t increase your dose, your blood pressure can crash, your blood sugar can drop, and you can go into shock. The Addison’s Disease Self Help Group has clear rules:- At the first sign of illness-fever, cough, diarrhea-double or triple your hydrocortisone dose.
- If you can’t keep pills down because of vomiting, you need an injection.
- Always carry an emergency hydrocortisone injection kit. Know how to use it.
- If you’re vomiting, unconscious, or too weak to swallow, give yourself a 100 mg intramuscular shot immediately.
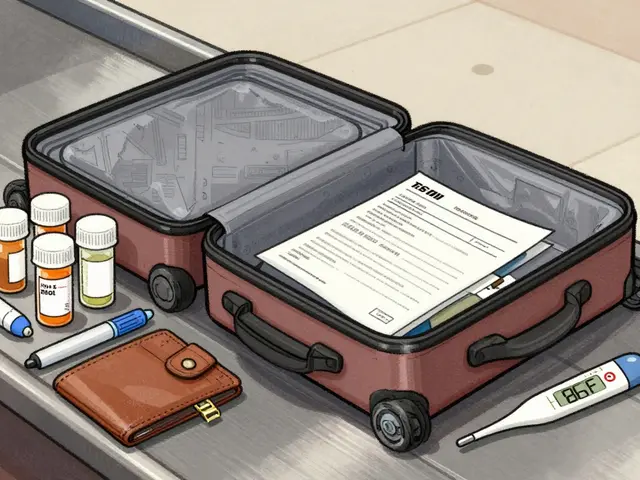
Medical Alert and Emergency Preparedness
Wearing a medical alert bracelet isn’t optional. It’s mandatory. If you collapse in public, paramedics won’t know you have Addison’s unless you tell them. And if they don’t know, they won’t give you the steroids you need. In the UK, 92% of patients who wore medical ID and carried emergency kits had 50% lower death rates from crisis. That’s not a small difference. That’s life or death. You should also carry a steroid card or letter from your endocrinologist. It tells emergency staff exactly what to do. If you’re in hospital for surgery, your dose needs to be adjusted-often to 100 mg IV on the day of the procedure. Dentists need to know too. A simple filling might require an extra 25 mg of hydrocortisone.The Hidden Costs and the Struggle to Get Care
Hydrocortisone isn’t expensive in theory. But in the US, without insurance, a month’s supply can cost $350 to $500. Even in the UK, some patients ration pills because of prescription charges or delays in renewals. One in four patients admit to cutting doses to make them last. Finding doctors who understand is another hurdle. Many GPs haven’t seen a case in years. Patients on Reddit say things like, “Finding someone who gets that I need to take extra hydrocortisone at 3 a.m. during a fever is nearly impossible.” The good news? Patients who complete the Addison’s Self Help Group’s “Sick Day Rules” training cut their crisis frequency by 85%. Education saves lives.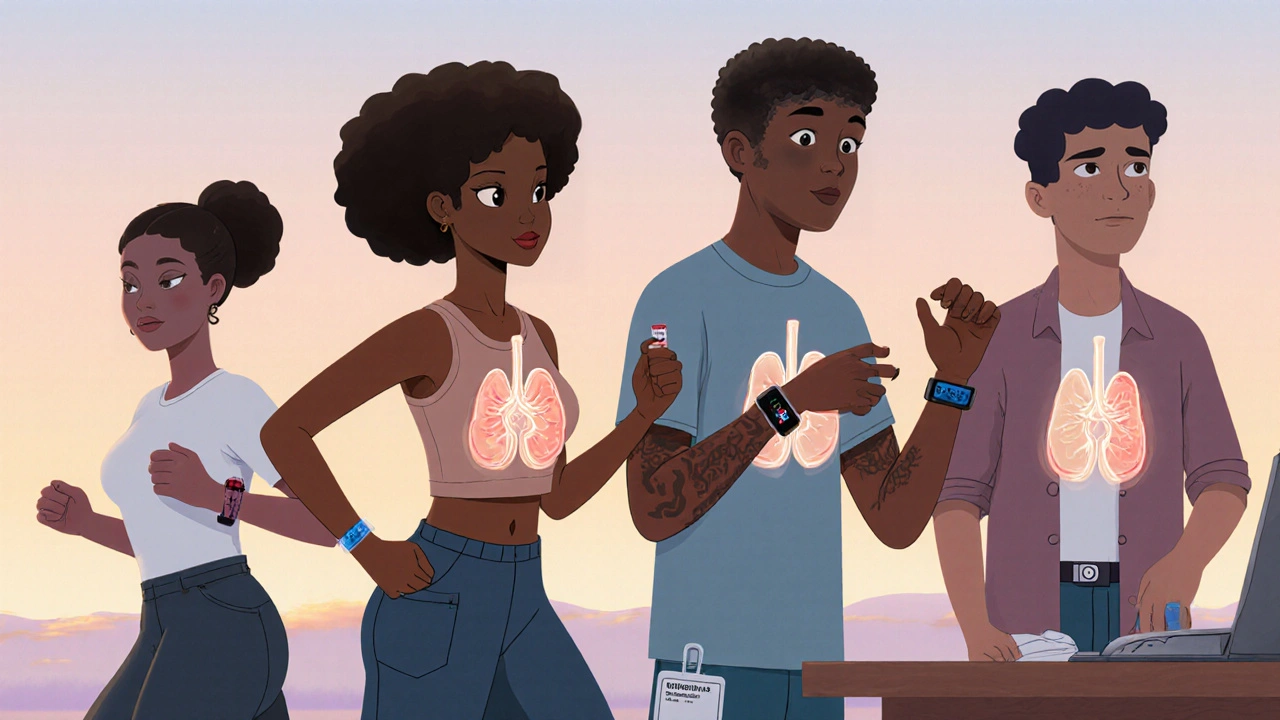
What’s Next for Treatment?
The field is moving. Chronocort, a modified-release hydrocortisone approved in 2023, gives more stable levels with once-daily dosing. Early data shows 37% fewer cortisol spikes and dips than standard tablets. That means fewer mood swings, less fatigue, and better sleep. Researchers are testing wearable devices that monitor cortisol levels in real time. If they work, they could alert you before a crisis hits-like a glucose monitor for diabetics. One expert predicts these could reduce crisis rates by 60% within five years. But even with better drugs, the biggest problem remains: awareness. The global prevalence of Addison’s is rising-10 to 14 cases per 100,000 people-and it’s increasing by 15% each year. Why? Because we’re testing for antibodies more often. We’re diagnosing earlier.Living with Addison’s: A Life of Precision
Addison’s disease isn’t a death sentence. It’s a chronic condition that demands discipline. You can work, travel, raise kids, run marathons. But you have to be the expert on your own body. You learn to track your symptoms. You know when your sodium is low because you feel weak and dizzy. You know when your fludrocortisone is too high because your ankles swell. You learn to say no to parties when you’re tired. You carry your injection kit everywhere-even to the beach. The life expectancy gap is real. Studies show people with Addison’s live 3 to 11 years less than average, mostly from heart problems caused by long-term steroid use or sudden crisis. But those who stick to their regimen, know their sick day rules, and get regular monitoring can live full, active lives. It’s not about being perfect. It’s about being prepared. One missed dose on a normal day? You’ll probably be fine. One missed dose during a fever? That’s when you risk dying.Frequently Asked Questions
Can Addison’s disease be cured?
No, Addison’s disease cannot be cured. The damage to the adrenal glands is permanent. But it can be effectively managed with lifelong steroid replacement therapy. With proper dosing and emergency preparedness, most people live normal lifespans and maintain good quality of life.
What happens if I miss a dose of hydrocortisone?
Missing one dose occasionally may cause fatigue, dizziness, or nausea, but it’s rarely dangerous if you’re otherwise healthy. However, if you miss doses during illness, stress, or injury, your risk of adrenal crisis increases dramatically. Always double or triple your dose when sick, and never skip doses during physical stress.
Do I need to take fludrocortisone forever?
Yes, if you have primary adrenal insufficiency (Addison’s disease), you need fludrocortisone for life. It replaces aldosterone, which your body can no longer make. Without it, you’ll develop dangerous electrolyte imbalances-low sodium and high potassium-which can lead to heart rhythm problems and shock. Secondary adrenal insufficiency doesn’t require fludrocortisone because the adrenal glands still produce aldosterone.
Why do people with Addison’s get dark skin?
High levels of ACTH, the hormone your pituitary releases to try to stimulate the adrenal glands, also bind to melanocyte receptors in the skin. This triggers increased melanin production, leading to hyperpigmentation. It’s most noticeable on sun-exposed areas, knuckles, gums, and skin folds. This is a key sign that differentiates Addison’s from secondary adrenal insufficiency, where ACTH is low and skin color remains normal.
Can I still exercise or play sports with Addison’s disease?
Absolutely. Many people with Addison’s compete in endurance sports, lift weights, and stay active. But you need to adjust your steroid dose around intense activity. For prolonged or high-intensity exercise, increase your hydrocortisone by 5-10 mg on the day of activity. Stay hydrated, monitor for fatigue, and carry your emergency injection. Always inform coaches or trainers about your condition.
How often should I see my endocrinologist?
At least once a year, but more often if you’ve had recent crises or dose changes. Your doctor will check your blood pressure, electrolytes (sodium, potassium), kidney function, and blood sugar. They’ll also screen for other autoimmune conditions like thyroid disease, type 1 diabetes, or vitamin B12 deficiency, which are common in people with Addison’s. Annual testing helps prevent long-term complications.
Is Addison’s disease hereditary?
It’s not directly inherited like a genetic disease, but there is a strong genetic link. People with certain HLA gene types are more likely to develop autoimmune Addison’s. If you have a close relative with an autoimmune condition-like type 1 diabetes, Hashimoto’s thyroiditis, or vitiligo-your risk is higher. Testing for 21-hydroxylase antibodies is recommended for family members if someone in the family has Addison’s.
Can stress cause an adrenal crisis?
Yes. Emotional stress, major life events, or even sleep deprivation can trigger a crisis because your body needs more cortisol to cope. While physical illness is the most common trigger, psychological stress is just as real. If you’re going through a divorce, losing a job, or caring for a sick relative, increase your hydrocortisone dose as you would during physical illness. Don’t wait until you feel sick-stress counts.




Suresh Ramaiyan
November 23, 2025 AT 00:49 AMBeen living with this for 12 years now. The salt cravings? Real. The 3 a.m. panic when you feel like you’re drowning in fatigue? Real. I keep a bottle of electrolytes by my bed. No one tells you how much your body becomes a machine you have to manually wind up every day. But you learn. And you get quiet about it. Because most people think you’re just lazy.
Still run 5Ks. Still cook for my kids. Still laugh. Just with a little more planning.
Vivian C Martinez
November 23, 2025 AT 07:21 AMThis is one of the most thorough, compassionate explanations of Addison’s I’ve ever read. Thank you for writing this. I’m a nurse in rural Oregon, and I’ve seen too many patients dismissed as ‘anxious’ or ‘depressed’ when they were slipping into crisis. Your breakdown of the ACTH test and sick day rules should be required reading for all primary care providers. I’m printing this out for our clinic.
Ross Ruprecht
November 23, 2025 AT 15:43 PMWhy do people even write long posts like this? It’s just cortisol. Take a pill. Done. Why make it sound like some epic survival saga? I mean, come on. It’s not even rare. Like 1 in 100k. You’re gonna die if you miss a dose? So? People die from forgetting insulin too. Chill.
Bryson Carroll
November 24, 2025 AT 09:53 AMLook I get the drama but this whole thing is just a glorified hormone replacement therapy. You’re not special. You’re not a warrior. You’re just a guy who needs to take a drug that costs less than a latte in most places. The fact that you’re posting this like it’s a TED Talk just proves how much of this is performative suffering. Also Chronocort? That’s a brand name. You’re being marketed to.
And why do you keep saying ‘you can live a full life’? That’s not a fact. That’s a pep talk. You’re still gonna die 10 years early. Get real.
Suzan Wanjiru
November 25, 2025 AT 16:11 PMAs someone who’s been on fludrocortisone since I was 17 I can confirm the ankle swelling thing is real. Also the sodium thing - if you’re dizzy after standing up and you’ve been drinking water like crazy, it’s not dehydration. It’s your aldosterone tanking. I keep a salt shaker in my purse. Always.
And if you’re thinking about skipping your dose because you’re ‘feeling fine’ - don’t. Your body doesn’t know you feel fine. It only knows you didn’t give it what it needs. Trust the science. Not the vibes.
Also - if you’re in the US and your pharmacy says ‘we don’t carry hydrocortisone’ - call a different one. It’s not rare. They’re just lazy. I’ve had to call 7 pharmacies before I found one that didn’t treat me like I was asking for cocaine.
Kezia Katherine Lewis
November 26, 2025 AT 19:52 PMThe hyperpigmentation mechanism is fascinating from a neuroendocrine standpoint. ACTH shares a precursor with MSH - melanocyte-stimulating hormone - so when the pituitary goes into overdrive trying to rescue the adrenal axis, you get ectopic melanogenesis. It’s a beautiful, tragic biomarker. Most clinicians miss it because they’re looking for ‘symptoms’ not ‘signs.’
Also, the 21-hydroxylase antibody titers are the gold standard for autoimmune etiology. If you’re testing positive and have low cortisol, you’re not ‘suspected’ - you’re confirmed. No need to wait for crisis. Early diagnosis saves lives.
And yes, the stress response is physiologically identical whether it’s emotional or physical. The HPA axis doesn’t discriminate. Your divorce is as real a trigger as your flu.
Henrik Stacke
November 28, 2025 AT 19:44 PMI’ve been a consultant endocrinologist in London for 27 years. I’ve seen this disease evolve from a death sentence to a manageable condition - but only because patients learned to speak up. I still get patients coming in after three years of being told they have ‘chronic fatigue.’ One woman was diagnosed after her daughter noticed her knuckles were dark - and asked her doctor. That child saved her mother’s life.
And yes - the emergency injection is non-negotiable. I’ve had patients die because they were too embarrassed to inject themselves in public. Don’t be that person. You are not a burden. You are a human being who needs medicine. Carry it. Use it. Live.
And if you’re reading this and you’re scared - you’re not alone. We’ve got you.
Javier Rain
November 30, 2025 AT 07:15 AMJust had my first adrenal crisis last year. Thought I was dying. Turned out I was just being an idiot and didn’t up my dose when I got the flu.
Now I have a little card in my wallet. A bracelet. A syringe in my backpack. Even when I go to the gym. I don’t care what people think. I’m alive because I learned.
Also - if you think you’re too young to need this info - you’re not. I was 24. I thought I was just tired from work.
Don’t be me.
Laurie Sala
December 1, 2025 AT 23:58 PMOkay but why do you keep saying ‘you can live a full life’ like it’s a miracle? Like it’s some kind of reward? It’s not a miracle - it’s a daily grind. You’re not ‘strong.’ You’re just not dead yet. And what about the people who can’t afford the meds? Or the ones whose doctors don’t believe them? Or the ones who get told ‘it’s all in your head’ for years? You’re painting this like it’s a motivational poster. It’s not. It’s survival. And it’s ugly. And it’s lonely. And no one talks about the guilt of being the one who’s ‘fine’ while your partner is in the ER again.
Stop glorifying it.
Lisa Detanna
December 3, 2025 AT 09:06 AMI’m from a family with three autoimmune disorders - Addison’s, Hashimoto’s, and type 1. We call it the ‘trifecta.’ My mom had it, my sister has it, and now I do. I didn’t know until I passed out at work. The doctor said, ‘You’re lucky you’re alive.’
But here’s what no one says: you get really good at hiding it. You smile through the nausea. You fake energy for your kids. You never say no to coffee, even when you’re shaking. You become a master of distraction.
So if you see someone who’s always tired but never complains - maybe they’re not lazy. Maybe they’re just trying not to die.
And if you’re reading this and you think it’s rare - it’s not. It’s just quiet.
Demi-Louise Brown
December 4, 2025 AT 09:29 AMHydrocortisone dosing must be individualized. Standard regimens are guidelines, not rules. Some patients require 30 mg daily. Others do fine on 12 mg. Titrate based on clinical response - not arbitrary numbers. Monitor for signs of over-replacement: weight gain, hypertension, insomnia. Under-replacement: fatigue, hypotension, hyponatremia.
Emergency injection: 100 mg IM. Do not wait. Do not hesitate. Time is cortisol.
Education is the most effective intervention. Period.