When your kidneys aren’t working right, it’s not just about urinating less or feeling tired—it changes how every medication in your body behaves. Renal impairment, a condition where kidney function drops below normal, often due to diabetes, high blood pressure, or aging. Also known as chronic kidney disease, it means drugs that used to be safe might now build up to dangerous levels. Your kidneys filter waste and help control drug clearance. When they slow down, even normal doses of common meds can turn toxic. This isn’t theoretical—it’s why people with kidney issues end up in the hospital from drugs like ibuprofen, metformin, or even antibiotics.
That’s why medication dosing, the careful adjustment of drug amounts based on kidney function becomes critical. Doctors don’t just guess—they use blood tests like eGFR to measure how well your kidneys are filtering. If your eGFR is below 60, many drugs need lower doses or longer gaps between doses. For example, drug toxicity, when a substance builds up to harmful levels because the body can’t clear it is a real risk with digoxin, lithium, and certain painkillers. Even supplements like potassium or vitamin D can become dangerous if your kidneys can’t flush out the excess. And it’s not just about pills—some IV meds, contrast dyes for scans, and herbal products need special caution too.
You might not feel symptoms until your kidney function is already significantly reduced. That’s why regular check-ups matter, especially if you’re on long-term meds. If you’ve been told you have renal impairment, don’t assume your old prescriptions are still safe. Talk to your pharmacist about every pill you take—even over-the-counter ones. They can flag hidden risks and help you avoid interactions. The good news? Many meds can still be used safely if dosed right. It’s not about stopping treatment—it’s about adjusting it.
Below, you’ll find real, practical guides on how to manage your meds when your kidneys aren’t working at full speed. From understanding why certain drugs need monitoring to knowing what to ask your doctor about dose changes, these posts cut through the noise. You’ll learn how to spot early signs of trouble, what to bring to your next appointment, and how to avoid common mistakes that lead to hospital visits. This isn’t theory—it’s what works for people living with kidney issues every day.
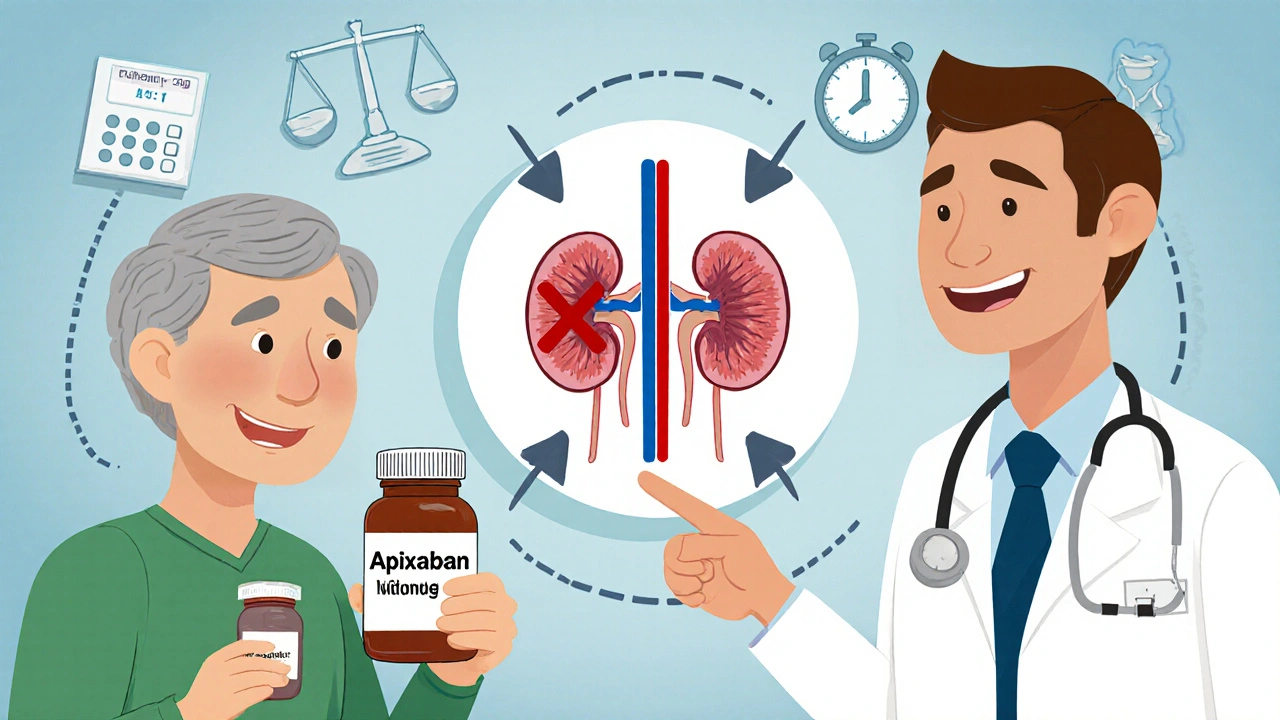
DOACs like apixaban and rivaroxaban require precise dosing in kidney disease to avoid bleeding or clots. Learn how to adjust doses using creatinine clearance and the ABCs rule, and why apixaban is often the safest choice.
read more