DOAC Dosing Calculator for Kidney Impairment
Calculate Your Creatinine Clearance
The Cockcroft-Gault formula is the only validated method for determining DOAC dosing. Enter your details below to get an accurate creatinine clearance (CrCl) calculation.
Your Creatinine Clearance
Recommended DOAC Dose
Important: This calculator is for educational purposes only. Always consult with your healthcare provider before making any medication adjustments.
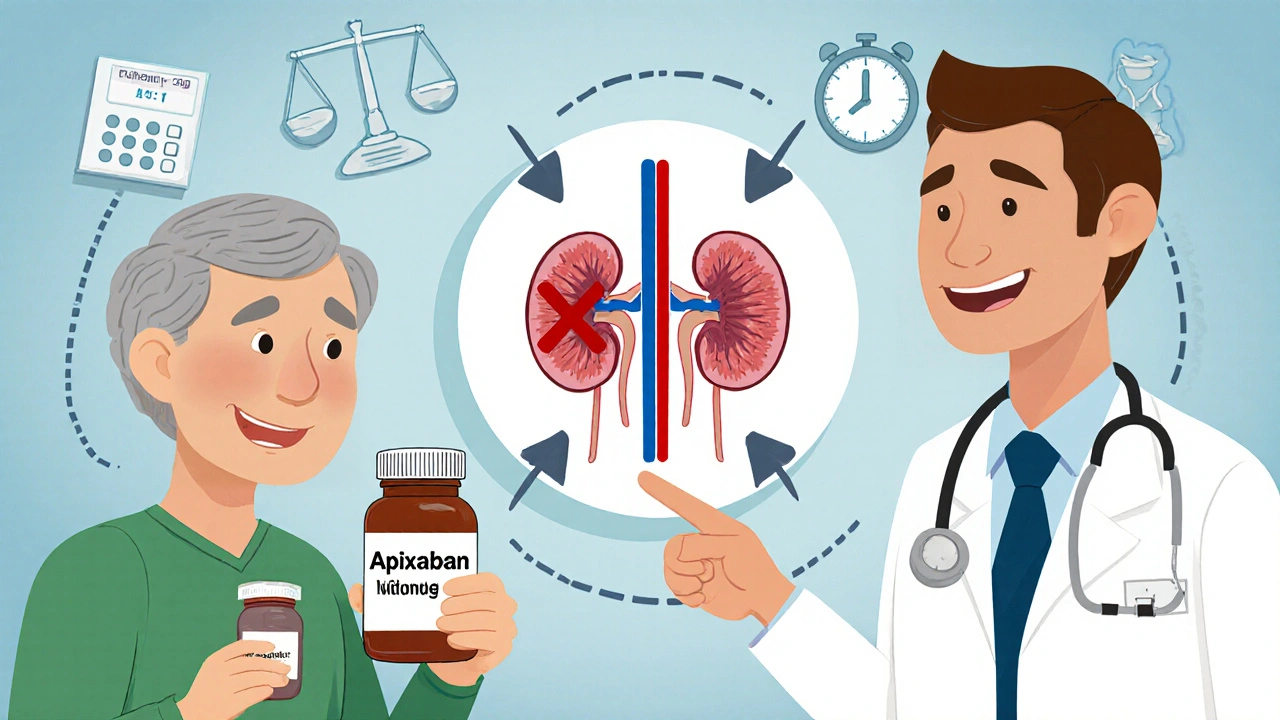
Why DOACs in Kidney Problems Need Special Care
Direct Oral Anticoagulants - or DOACs - are now the go-to blood thinners for millions of people with atrial fibrillation. But if your kidneys aren’t working well, taking the standard dose can be dangerous. Too much drug builds up in your body and raises your risk of serious bleeding. Too little, and you’re unprotected against strokes or clots. The problem isn’t the drugs themselves - it’s that your kidneys help clear them out. When kidney function drops, the balance shifts. And getting it wrong can land you in the hospital.
Unlike warfarin, which needs regular blood tests and dietary tweaks, DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban were designed to be simple. But that simplicity falls apart in people with chronic kidney disease. About 1 in 3 patients with atrial fibrillation also have moderate to severe kidney impairment. And yet, studies show nearly 4 out of 10 of these patients get the wrong DOAC dose. That’s not just a mistake - it’s a preventable risk.
Which DOACs Are Safe - and Which Aren’t
Not all DOACs behave the same in people with kidney problems. Apixaban stands out. It’s the only one with data showing it’s safe even in end-stage kidney disease, including patients on dialysis. In fact, in real-world use, apixaban has been linked to lower bleeding rates than warfarin in this group. That’s why many nephrologists now consider it the best option when kidneys are failing.
Rivaroxaban? Not so much. Guidelines say don’t use it if your creatinine clearance is below 15 mL/min. It’s cleared mostly by the kidneys, and in advanced kidney disease, it builds up fast. Dabigatran and edoxaban also need strict dose reductions in moderate to severe kidney impairment. Dabigatran should be cut to 75 mg twice daily if your CrCl is between 15 and 30 mL/min - and avoided completely below that. Edoxaban drops to 30 mg once daily in the same range. Both are off-limits if CrCl is under 15.
Here’s the reality: if you have stage 4 or 5 chronic kidney disease, your doctor should be thinking about apixaban first. The others? They’re risky unless your kidney function is still above 30 mL/min.
The One Number That Matters: Creatinine Clearance (CrCl)
Don’t rely on your eGFR number. That’s what most labs report, and it’s what many doctors see first. But for DOAC dosing, eGFR is misleading. The only number that counts is creatinine clearance - calculated using the Cockcroft-Gault formula. This isn’t a suggestion. It’s a requirement from the FDA and every major guideline. Using eGFR instead can lead to over- or under-dosing by up to 40%.
The Cockcroft-Gault formula looks at your age, weight, sex, and serum creatinine. It’s not perfect - especially in elderly or very thin people - but it’s the only one validated for DOAC dosing. Many pharmacies now have built-in calculators. If yours doesn’t, ask for it. If your doctor skips this step, push back. You’re not being difficult - you’re protecting yourself.
Example: A 78-year-old woman, weighing 55 kg, with a creatinine of 1.4 mg/dL. Her eGFR might say 40 mL/min. But her CrCl? Around 28 mL/min. That changes everything. Apixaban would drop from 5 mg twice daily to 2.5 mg twice daily. Rivaroxaban would be stopped entirely.
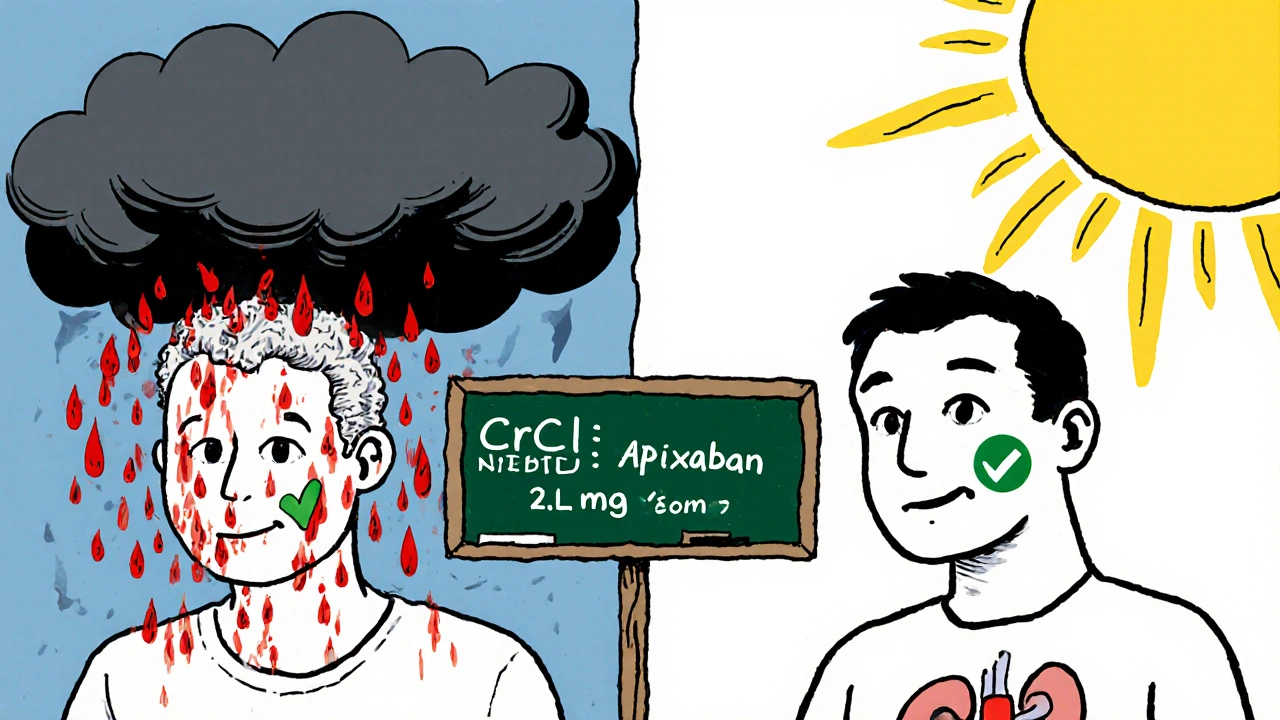
Apixaban’s Dose Reduction Rules - The ABCs
If you’re on apixaban and have kidney issues, you need to know the ABCs:
- Age 80 or older
- Body weight 60 kg or less (about 132 lbs)
- Creatinine 133 μmol/L or higher (1.5 mg/dL)
If you meet two or more of these, your dose drops to 2.5 mg twice daily - no matter what your CrCl says. This isn’t just a guideline. It’s FDA-approved. And it’s based on real data showing lower bleeding rates with this lower dose in older, smaller, or higher-creatinine patients.
But here’s the catch: some doctors forget the weight and age criteria and only look at creatinine. That’s dangerous. A 75-year-old woman weighing 52 kg with normal creatinine still needs the lower dose. Don’t assume your doctor knows this. Ask: “Do I meet two of the ABCs?”
What Happens When Dosing Goes Wrong
Getting the dose wrong has real consequences. Too high? You could bleed into your stomach, brain, or joints. A 2022 study in JAMA Internal Medicine found that 37% of DOAC prescriptions in kidney patients had dosing errors - and nearly half of those led to major bleeding or hospitalization.
Too low? You’re not protected. A patient with atrial fibrillation and poor kidney function who gets an underdosed DOAC has the same stroke risk as someone not taking any blood thinner. And strokes from AF aren’t minor - they’re often disabling or deadly.
One case from a UK hospital: a 79-year-old man on standard-dose apixaban (5 mg twice daily) had a GI bleed that required emergency surgery. He weighed 58 kg, was 81, and had creatinine of 1.4. He met two ABCs. He should’ve been on 2.5 mg. He wasn’t. He survived - but barely.
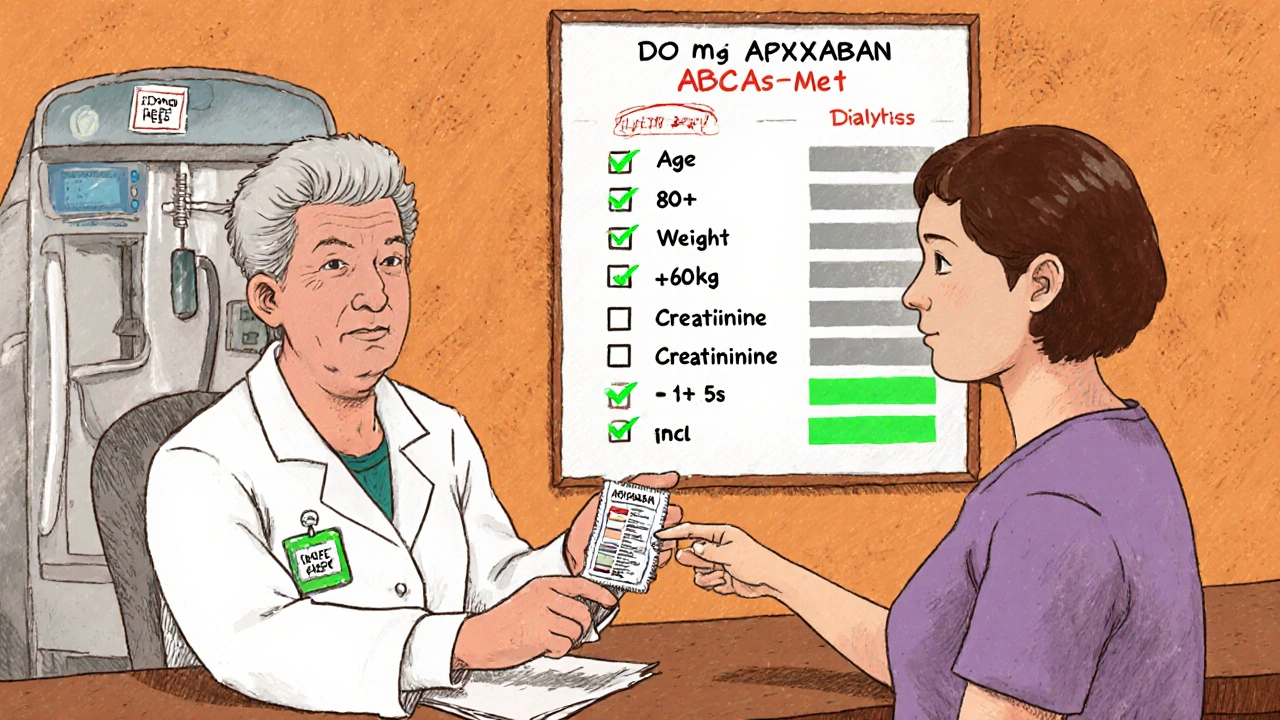
Special Cases: Dialysis and Extreme Weight Loss
People on hemodialysis were once left out of DOAC studies. That’s changing. Apixaban is now used in over 10,000 dialysis patients worldwide, with data showing it’s safer than warfarin. The dose? Usually 2.5 mg twice daily. But don’t assume this is automatic. Some nephrologists still avoid DOACs here - even though guidelines now support apixaban.
What about someone who’s lost a lot of weight? A cancer patient who dropped from 90 kg to 50 kg? Their dose needs rechecking. The same goes for frail elderly people with low muscle mass. Their creatinine might look normal, but their actual kidney clearance is lower. That’s where the Cockcroft-Gault formula and the ABCs come in - they catch what lab numbers miss.
What to Do Right Now
If you’re on a DOAC and have kidney disease, here’s your action plan:
- Ask for your creatinine clearance (CrCl), not eGFR. Get it in mL/min.
- Check if you meet two of the ABCs for apixaban.
- Confirm your DOAC dose matches your CrCl and your personal factors.
- Ask if your doctor uses the Cockcroft-Gault formula - if not, insist.
- Get your kidney function checked every 3 to 6 months - more often if you’re sick, losing weight, or on dialysis.
Don’t wait for your next routine visit. If you’re unsure, call your pharmacist. They’re trained to catch these errors. Many have apps that auto-calculate CrCl and flag wrong doses.
What’s Coming Next
More data is on the way. The RENAL-AF trial, expected to finish in 2025, will compare apixaban to adjusted warfarin in patients with severe kidney disease. That could finally give us clear answers for the hardest cases.
Right now, the message is simple: DOACs are powerful tools - but only when used correctly. In kidney disease, precision isn’t optional. It’s life-saving.
Can I still take apixaban if I’m on dialysis?
Yes, apixaban is the only DOAC recommended for patients on dialysis. The standard dose is 2.5 mg twice daily, especially if you meet two of the ABCs (age ≥80, weight ≤60 kg, creatinine ≥1.5 mg/dL). Studies show it’s safer than warfarin in this group, with lower bleeding rates. Always confirm your dose with your nephrologist or pharmacist.
Why can’t I just use eGFR instead of CrCl for DOAC dosing?
eGFR overestimates kidney function in older, frail, or low-weight patients. DOACs are cleared by the kidneys, and using eGFR can lead to dangerously high doses. The FDA and all major guidelines require the Cockcroft-Gault formula for dosing decisions. It’s the only method validated for this purpose. Don’t trust your lab’s eGFR number for DOACs - ask for CrCl.
What if my doctor refuses to change my DOAC dose?
If your kidney function has changed or you meet the ABCs for apixaban, you have the right to ask for a dose review. Bring printed guidelines from the American Heart Association or KDIGO. Ask to speak with a clinical pharmacist - they specialize in these interactions. If your doctor still refuses, seek a second opinion from a cardiologist or nephrologist who specializes in anticoagulation. Your safety matters more than protocol.
Is warfarin better than DOACs for advanced kidney disease?
Not necessarily. Warfarin carries a higher risk of bleeding, especially brain bleeds, in patients with advanced kidney disease. It also requires frequent blood tests and is affected by diet and other drugs. Apixaban has proven safer in multiple studies. While warfarin is still used in some cases, apixaban is now the preferred option for most patients with CKD or on dialysis - unless there’s a mechanical heart valve or another specific reason.
Can I take a lower dose of rivaroxaban if my kidneys are weak?
No. Rivaroxaban is not approved for use when creatinine clearance is below 15 mL/min, and even at higher levels, it’s riskier than apixaban in kidney disease. There’s no safe reduced dose for advanced CKD. If your kidneys are impaired, switching to apixaban is the recommended move. Don’t try to adjust rivaroxaban yourself - it’s not safe.
Final Thought: Don’t Assume - Ask
DOACs are not one-size-fits-all. Especially with kidney problems, the difference between 2.5 mg and 5 mg could mean the difference between safety and disaster. Your kidneys change. Your weight changes. Your health changes. Your dose should change too. Make sure you’re not just getting a prescription - you’re getting the right one.





Craig Hartel
November 28, 2025 AT 19:06 PMJust had my dad’s DOAC dose reviewed last week thanks to this post - he’s 82, weighs 56kg, and his CrCl was 27. Docs were about to keep him on 5mg apixaban. We asked for Cockcroft-Gault, they were surprised we knew to ask. Now he’s on 2.5mg. No more scary GI bleed scares. Thanks for the clarity!
Chris Kahanic
November 30, 2025 AT 01:17 AMThe discrepancy between eGFR and CrCl is a systemic failure in clinical practice. It is not merely an oversight; it is a structural blind spot that endangers vulnerable populations. The reliance on automated lab values without clinical validation is indefensible.
Geethu E
December 1, 2025 AT 04:55 AMAs a nurse in Mumbai, I see this ALL the time. Doctors copy-paste prescriptions. One guy on rivaroxaban 20mg with CrCl 12? Bro, that’s a death sentence. I printed the KDIGO guidelines and handed them to the doc. He rolled his eyes but changed it to apixaban 2.5mg. Saved his life. You gotta be the patient’s advocate - no one else will.
anant ram
December 2, 2025 AT 00:33 AMListen. Listen. Listen. If you’re on a DOAC and have kidney issues - check your CrCl. Check your weight. Check your age. Check the ABCs. If two of them apply - you need the lower dose. No exceptions. No guesses. No ‘I think it’s fine.’ Your kidneys aren’t guessing. Your blood isn’t guessing. Don’t you dare guess either.
king tekken 6
December 3, 2025 AT 16:06 PMso like... is this all just a big pharma scam? like, why did they make these drugs so dependent on kidneys? why not make them liver-metabolized? maybe the FDA is in bed with the labs that charge for cockcroft-gault calculators. also i think eGFR is just a capitalist plot to make us pay more for blood tests. i mean, think about it.
DIVYA YADAV
December 4, 2025 AT 03:36 AMAnd let’s not forget who benefits from this confusion - Western pharmaceutical giants pushing DOACs as ‘simple’ while ignoring how Indian and African bodies metabolize drugs differently. They test these drugs on white, middle-aged men in the US and then sell them globally. My cousin in Delhi got a 5mg dose of apixaban and nearly bled out - her CrCl was 24, she weighed 48kg, she’s 74 - but the doctor trusted the eGFR. This isn’t medicine - it’s medical colonialism.
Kim Clapper
December 4, 2025 AT 23:47 PMWhile I appreciate the technical detail, I must express my profound concern regarding the normalization of patient self-advocacy in clinical decision-making. The physician-patient relationship is a sacred trust, not a marketplace of competing interpretations of pharmacokinetics. To demand the Cockcroft-Gault formula is to undermine the authority of medical expertise - which, I remind you, requires a decade of training and licensing.
Bruce Hennen
December 6, 2025 AT 14:26 PMApixaban is not 'the only safe DOAC' in renal impairment. It is the least dangerous among four flawed options. The real issue is that anticoagulation in CKD is inherently high-risk. No drug is safe. The fact that guidelines even permit DOACs in CrCl 15-30 is a compromise born of desperation, not evidence. Warfarin remains the gold standard for true clinical caution.
Jake Ruhl
December 7, 2025 AT 04:00 AMok but what if your doctor is just lazy and your eGFR says 40 so they just give you the regular dose and you dont even know? like i had a friend who was on rivaroxaban and his creatinine was 1.6 but he was 80 and 55kg and he had a brain bleed and now he cant talk and his wife says the doctor never even checked his weight or age and just looked at the eGFR and was like 'eh its fine' and now hes in a nursing home and i just wanna scream because this couldve been prevented with like 2 minutes of math
Chuckie Parker
December 8, 2025 AT 22:02 PMWhy are we letting bureaucrats and guidelines dictate medicine? In my clinic, we use clinical judgment. If the patient looks good, the dose is fine. CrCl? eGFR? Who cares. We’ve been doing this for decades without calculators. This post is overcomplicating what should be simple. Trust your doctor, not some algorithm.
Michael Segbawu
December 9, 2025 AT 13:49 PMThey’re all lying. DOACs are just a cover. The real reason they push apixaban in dialysis patients is because the government pays hospitals more for using 'newer' drugs. I’ve seen the invoices. It’s all about reimbursement codes. Your kidney isn’t failing - your bank account is being drained. Ask your pharmacist if they get kickbacks for prescribing apixaban. I bet they won’t answer.