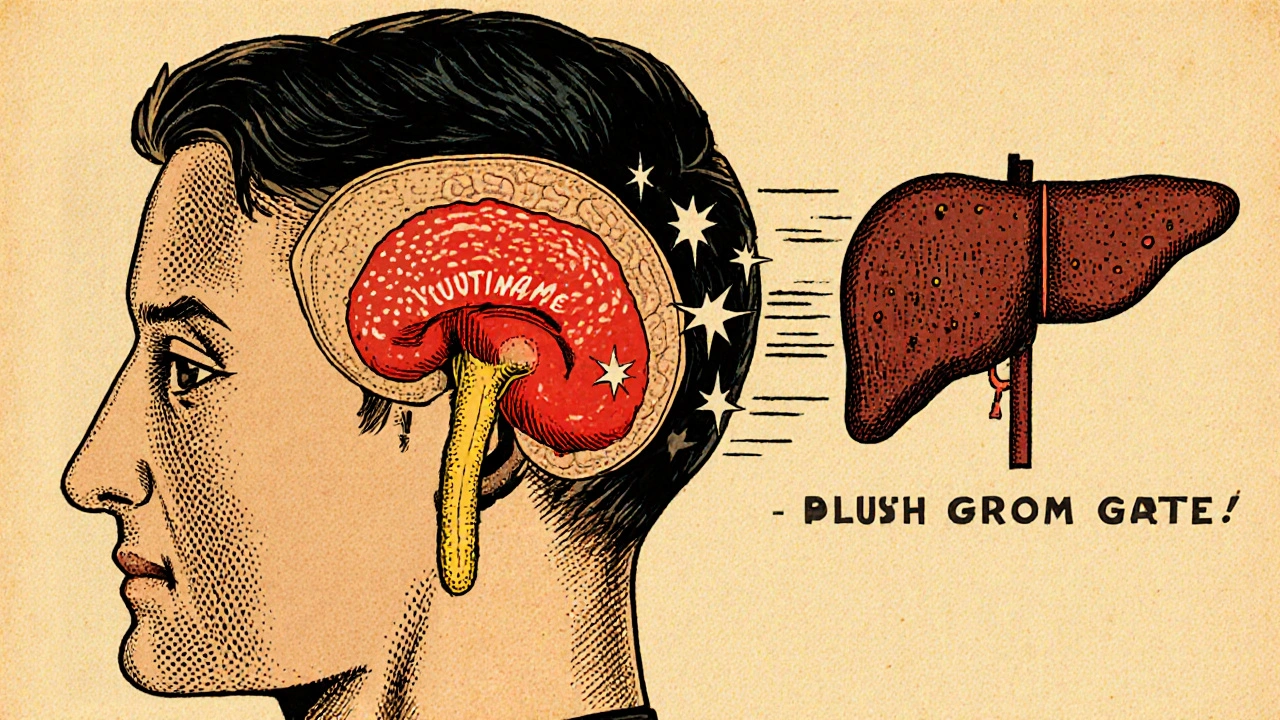
When dealing with growth hormone excess, a condition where the pituitary gland releases too much GH, leading to abnormal tissue growth. Also known as GH hypersecretion, it often stems from a pituitary adenoma, a benign tumor that overproduces hormones. The excess GH drives up levels of IGF-1, the insulin‑like growth factor that mediates most of GH’s effects on bones and organs. When this hormonal cascade persists into adulthood, it typically manifests as acromegaly, the characteristic enlargement of hands, feet, and facial features. If the overproduction starts before growth plates close, the result is gigantism, where overall stature skyrockets. In short, growth hormone excess encompasses a spectrum of disorders linked by the same hormonal driver, and understanding the role of the pituitary adenoma and IGF‑1 helps clinicians pinpoint the problem quickly.
Patients with GH excess often notice subtle changes first: ring sizes grow, shoes feel tighter, or facial features seem coarser. Headaches and visual disturbances can also appear if the adenoma presses on nearby structures. To confirm the diagnosis, doctors measure fasting IGF‑1 levels because they stay elevated even when GH pulses fluctuate. An oral glucose tolerance test (OGTT) is another tool; in healthy people, glucose suppresses GH, but in excess it stays high. Imaging, usually a high‑resolution MRI, locates the adenoma and assesses its size.
Treatment hinges on the cause. Small, well‑defined adenomas are often removed surgically, offering the best chance for cure. If surgery isn’t feasible or leaves residual disease, medication steps in. Somatostatin analogs (like octreotide) bind to receptors that curb GH release, while GH receptor antagonists (such as pegvisomant) block IGF‑1 production downstream. Radiation therapy is a third option, typically reserved for stubborn cases. Lifestyle tweaks—maintaining a balanced diet, staying active, and monitoring blood sugar—support overall health but don’t replace medical therapy.
The articles gathered below cover a wide range of medical topics, from drug comparisons and disease risk factors to practical health tips. Together they form a toolbox for anyone navigating hormone‑related disorders, medication decisions, or general wellness. Whether you’re looking for deeper insight into the diagnostic steps for GH excess, want to compare treatment options, or simply need a refresher on related conditions like acromegaly, the collection offers clear, actionable information. Dive in to explore the details that can help you or a loved one manage growth hormone excess effectively.
A clear, easy-to-follow guide on acromegaly covering symptoms, diagnosis steps, treatment options, and everyday management tips.
read more