When working with eye complications, any condition that harms the eye’s structures and impairs vision. Also known as ocular issues, they can arise from disease, injury, or medication side effects. Retinal disease, disorders affecting the light‑sensing layer at the back of the eye is a common subset, and glaucoma, pressure‑related optic nerve damage that leads to vision loss often sneaks up until it’s too late. Eye complications encompass retinal disease, and they frequently require timely diagnosis to prevent irreversible damage. Early signs such as blurred spots, halos around lights, or sudden loss of peripheral vision should prompt an eye‑doctor visit. Diagnostic tools like optical coherence tomography (OCT), visual field testing, and fundus photography let specialists map damage before it worsens. Understanding how systemic health intertwines with ocular health helps you spot problems early and act fast.
Another major player is cataract, clouding of the eye’s natural lens that blurs vision. While age is the biggest risk factor, diabetes, smoking, and prolonged steroid use accelerate its formation. diabetic retinopathy, damage to retinal blood vessels caused by chronic high blood sugar illustrates how a systemic disease can trigger eye complications, often presenting as floaters, blurred vision, or dark patches. Certain chemotherapy agents like cyclophosphamide and inhaled steroids such as fluticasone are known to cause ocular side effects ranging from dry eye to increased intra‑ocular pressure. Even common antihistamines or blood‑pressure meds can dry the surface of the eye, making it more vulnerable to infection. Because eye complications often require a multidisciplinary approach—ophthalmologists, endocrinologists, and primary‑care doctors coordinating care—treatment plans may include laser therapy, anti‑VEGF injections, prescription eye drops, or surgical lens replacement. When an eye condition is caught early, these interventions can preserve sight and improve quality of life.
Prevention starts with routine eye exams, especially if you have risk factors like diabetes, hypertension, or a family history of glaucoma. Lifestyle tweaks—wearing UV‑blocking sunglasses, staying hydrated, managing blood sugar, and quitting smoking—lower the odds of developing severe eye complications. Modern screening tools, such as swept‑source OCT and wide‑field retinal imaging, detect subtle changes that were invisible a decade ago. Most experts recommend a full dilated exam at least once every two years for adults, and more frequently for those with known risk. The articles below dive into related health topics, from medication comparisons to disease management, giving you a broader picture of how overall wellness influences ocular health. Whether you’re looking for signs of early retinal disease or guidance on medication‑induced eye issues, this collection equips you with practical insights. Keep reading to discover detailed explanations, treatment options, and tips that can help you safeguard your vision.
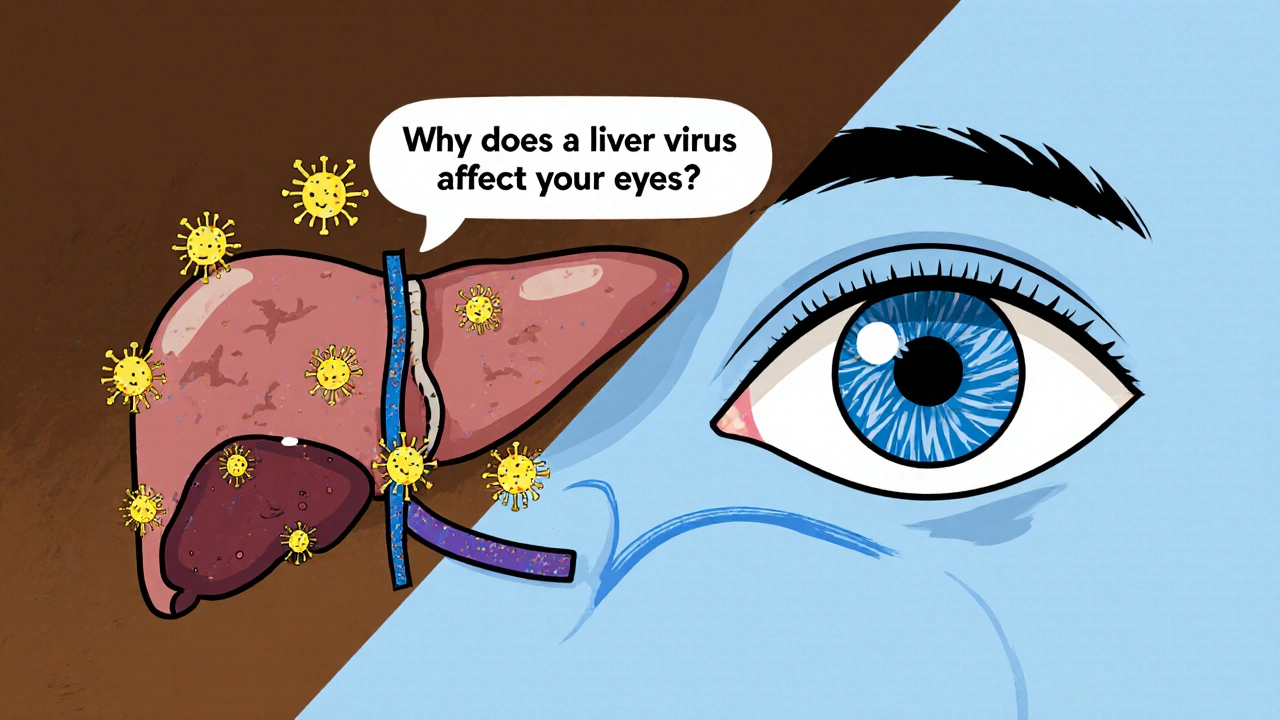
Explore how genotype 3 chronic hepatitis C can affect eye health, the symptoms to watch for, screening steps, and treatment options to safeguard vision.
read more