When digoxin toxicity, a dangerous buildup of the heart medication digoxin in the body that can disrupt rhythm and function. Also known as digitalis poisoning, it happens when the dose is too high or the body can’t clear it properly. Digoxin is used for heart failure and certain irregular heartbeats, but its safety window is narrow. Even small changes in kidney function, hydration, or other meds can push levels into the danger zone.
People on digoxin often don’t realize they’re at risk until symptoms show up. Common signs include nausea, vomiting, blurry yellow-green vision, confusion, and unusual heart rhythms — like a slow pulse or skipped beats. These aren’t just side effects; they’re red flags. Older adults, those with kidney problems, or people taking diuretics are especially vulnerable. Low potassium or magnesium levels, often caused by water pills, make digoxin more likely to cause harm. It’s not rare — studies show up to 20% of patients on long-term digoxin have levels that put them at risk, even if they’re taking the right dose.
What makes digoxin toxicity tricky is how easily it’s mistaken for something else. Nausea? Maybe it’s the flu. Vision changes? Maybe it’s aging. A slow heartbeat? Maybe you’re just tired. But when these show up together — especially in someone taking digoxin — it’s time to act. Blood tests can check digoxin levels and electrolytes, and stopping the drug quickly can prevent serious harm. Many of the posts below cover how other heart meds, like beta blockers or diuretics, interact with digoxin, and how to avoid dangerous combinations. You’ll also find guides on monitoring kidney function, recognizing early symptoms, and what to do if you miss a dose or take too much. This isn’t theoretical — these are real experiences from people managing chronic heart conditions, and the advice here can help you stay safe.
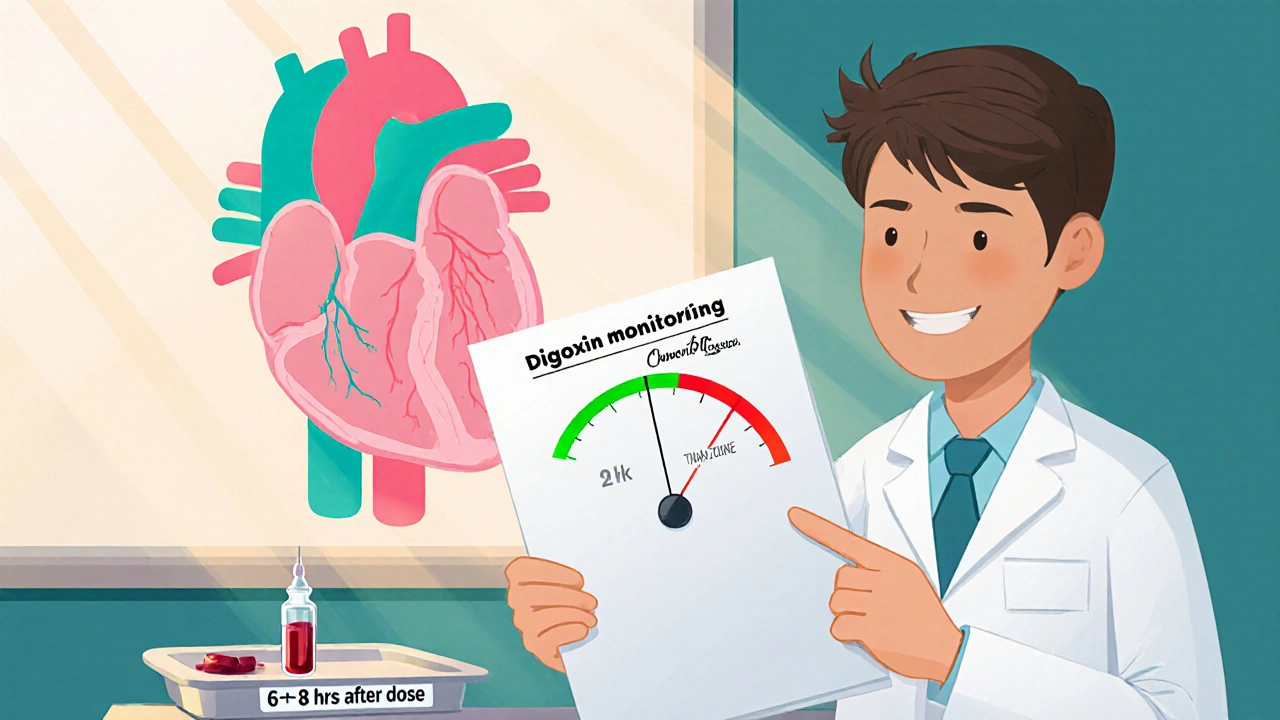
Learn why regular digoxin monitoring saves lives, how to interpret serum levels, and practical steps for safe dosing.
read more