When dealing with Acromegaly treatment, the set of medical, surgical, and radiation options that control excess growth hormone. Also known as GH excess therapy, it targets the underlying tumor and its hormonal output. Understanding the pieces of the puzzle helps you choose the right path and reduces the guesswork that often comes with chronic conditions.
Somatostatin analogs, drugs that mimic the natural hormone somatostatin to suppress growth hormone release are the workhorses of medical therapy. Acromegaly treatment often starts with these meds because they can lower IGF‑1 levels quickly and are taken as a simple injection. Common brands like octreotide and lanreotide are usually well‑tolerated; the most frequent side‑effects are mild stomach cramps and occasional gallstones. If you’re aiming for a non‑surgical route, these analogs are usually the first line.
For patients whose tumors don’t shrink enough with analogs, Pituitary surgery, a transsphenoidal operation that removes the growth‑hormone‑producing adenoma becomes the next step. The goal is to eliminate the source of excess hormone production. Success rates exceed 80 % for small, well‑defined tumors, and most surgeons perform the procedure through the nose, avoiding a craniotomy. Recovery is typically quick, but you’ll need post‑op hormone checks to confirm the surgery’s effect.
If surgery isn’t an option or the tumor is invasive, Radiotherapy, targeted radiation that shrinks residual tumor tissue over months to years can step in. Conventional fractionated radiotherapy or newer stereotactic radiosurgery (like Gamma Knife) delivers focused beams that gradually lower growth hormone levels. The trade‑off is a delayed response—often 1–3 years—plus a small risk of hypopituitarism, so doctors monitor pituitary function closely.
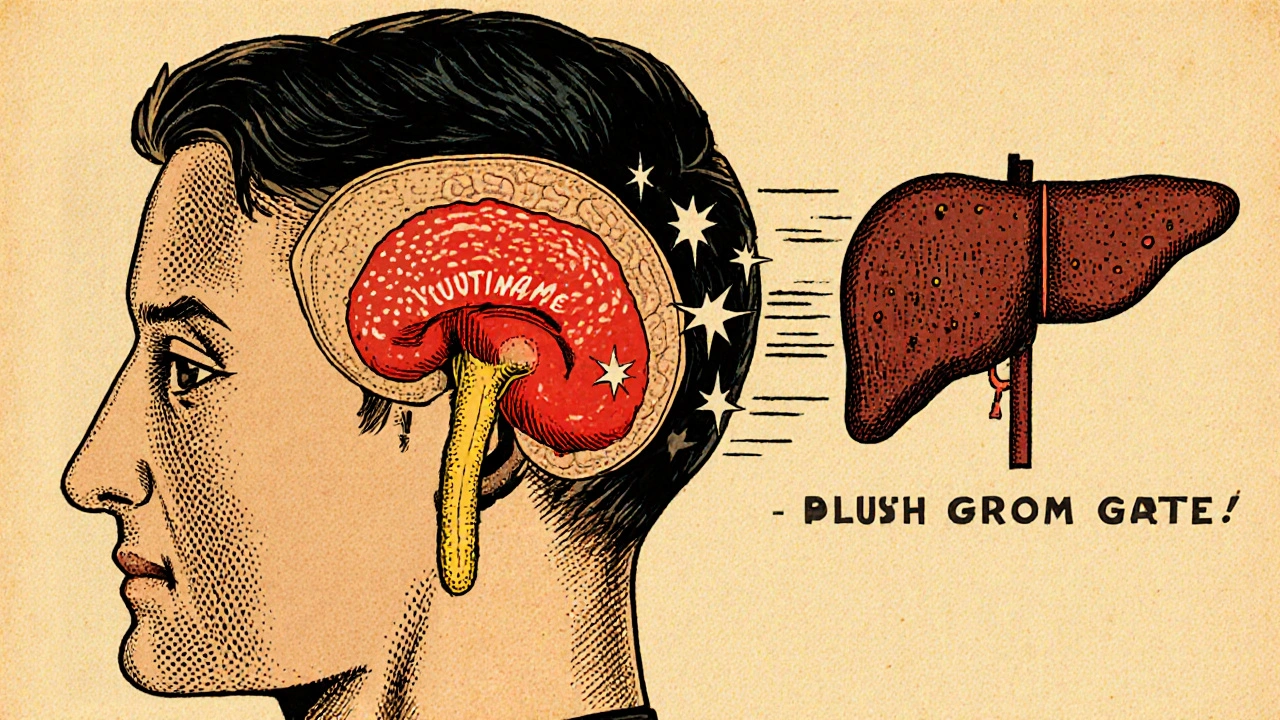
When both surgery and somatostatin analogs fall short, GH receptor antagonists, agents such as pegvisomant that block growth hormone receptors in the liver offer an alternate route. Instead of suppressing hormone production, they prevent the hormone from signaling, which drops IGF‑1 to normal levels. This class is especially useful for patients who develop resistance to somatostatin analogs. The main downside is the need for daily injections and regular liver‑function testing.
Beyond the core therapies, effective medical monitoring, regular blood tests for IGF‑1 and growth hormone, plus imaging to track tumor size ties everything together. Consistent monitoring tells you whether a medication dose needs tweaking, if a tumor is creeping back, or whether side‑effects are emerging. Most endocrinologists schedule IGF‑1 checks every 3–6 months and MRI scans annually for the first few years after treatment.
Managing side‑effects is another piece of the puzzle. For example, somatostatin analogs can cause gallbladder sludge, so an ultrasound may be recommended if you develop abdominal pain. GH receptor antagonists may affect liver enzymes, prompting routine blood work. Knowing what to watch for empowers you to speak up early and keep the treatment plan on track.
Putting it all together, acromegaly treatment usually follows a stepwise approach: start with medication, consider surgery if the tumor is accessible, add radiotherapy for residual disease, and use GH receptor antagonists when needed. Each step depends on tumor size, hormone levels, age, and personal health goals. Your care team will weigh these factors to craft a plan that balances effectiveness with quality of life.
Below you’ll find a curated set of articles that dig deeper into each of these options, compare drug profiles, explain surgical techniques, and share patient‑focused tips for living with acromegaly. Whether you’re just learning what treatment looks like or you’re fine‑tuning an existing plan, the collection offers practical insights you can apply right away.
A clear, easy-to-follow guide on acromegaly covering symptoms, diagnosis steps, treatment options, and everyday management tips.
read more