When your airways tighten up and breathing feels like trying to suck air through a straw, bronchodilators and corticosteroids are the two main tools doctors reach for. They don’t do the same thing - and they’re not interchangeable. But together, they can change how you live with asthma or COPD. Most people get one or both of these medications in an inhaler, but many don’t know how to use them right. That’s where things go wrong.
What Bronchodilators Do - And When You Need Them
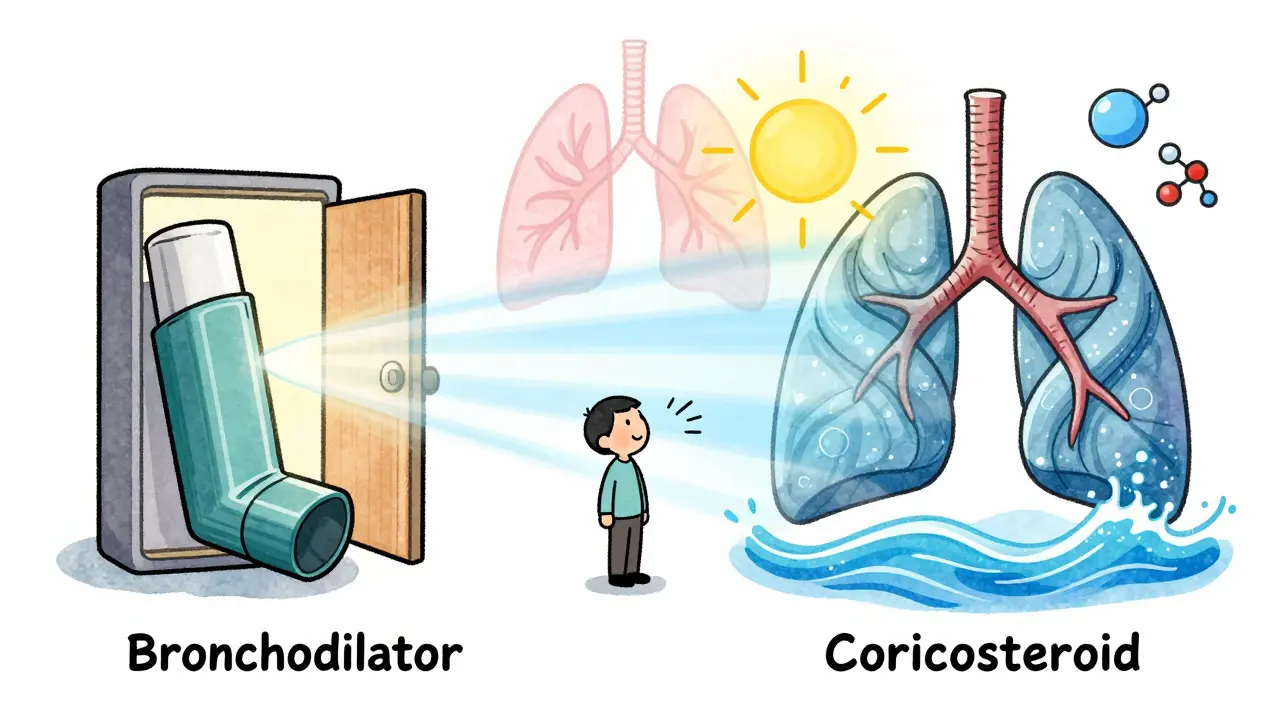
Bronchodilators open up your airways. They don’t fix the inflammation - they just make it easier to breathe right now. Think of them like a doorstop for your lungs. When you feel tightness, wheezing, or shortness of breath, a bronchodilator can give you relief in 15 to 20 minutes.
There are two main types. Beta-2 agonists - like albuterol (Ventolin, ProAir) - work by targeting receptors in your airway muscles. This triggers a chain reaction inside your cells that makes the muscles relax. The effect lasts 4 to 6 hours for short-acting versions (SABAs), which is why they’re your go-to for sudden symptoms. Long-acting versions (LABAs), like salmeterol or formoterol, last 12 hours or more. But here’s the catch: LABAs alone are dangerous for asthma. Using them without an anti-inflammatory can triple your risk of a life-threatening attack. That’s why they’re always paired with corticosteroids.
The other kind of bronchodilator is the anticholinergic. Ipratropium (Atrovent) and tiotropium (Spiriva) block signals from your nervous system that cause airway tightening. They kick in slower than beta-agonists - around 15 minutes - but tiotropium lasts a full 24 hours. These are more common in COPD than asthma, but they’re still used in combination therapies.
What Corticosteroids Do - And Why They Take Time
Corticosteroids are the opposite of quick fixes. They don’t open your airways. Instead, they calm down the inflammation that’s always there in asthma and COPD. That’s why they’re called controller medications. You won’t feel better the first day you use them. It takes days - sometimes weeks - for them to reduce swelling, mucus, and sensitivity in your lungs.
They work by slipping into your lung cells and turning off dozens of genes that cause inflammation. Fluticasone (Flovent), budesonide (Pulmicort), and beclomethasone (Qvar) are the most common inhaled versions. They’re not steroids like the ones athletes abuse. These are targeted, low-dose, and delivered straight to your lungs so your body gets almost none of it. That’s why side effects are rare - if you rinse your mouth after using them.
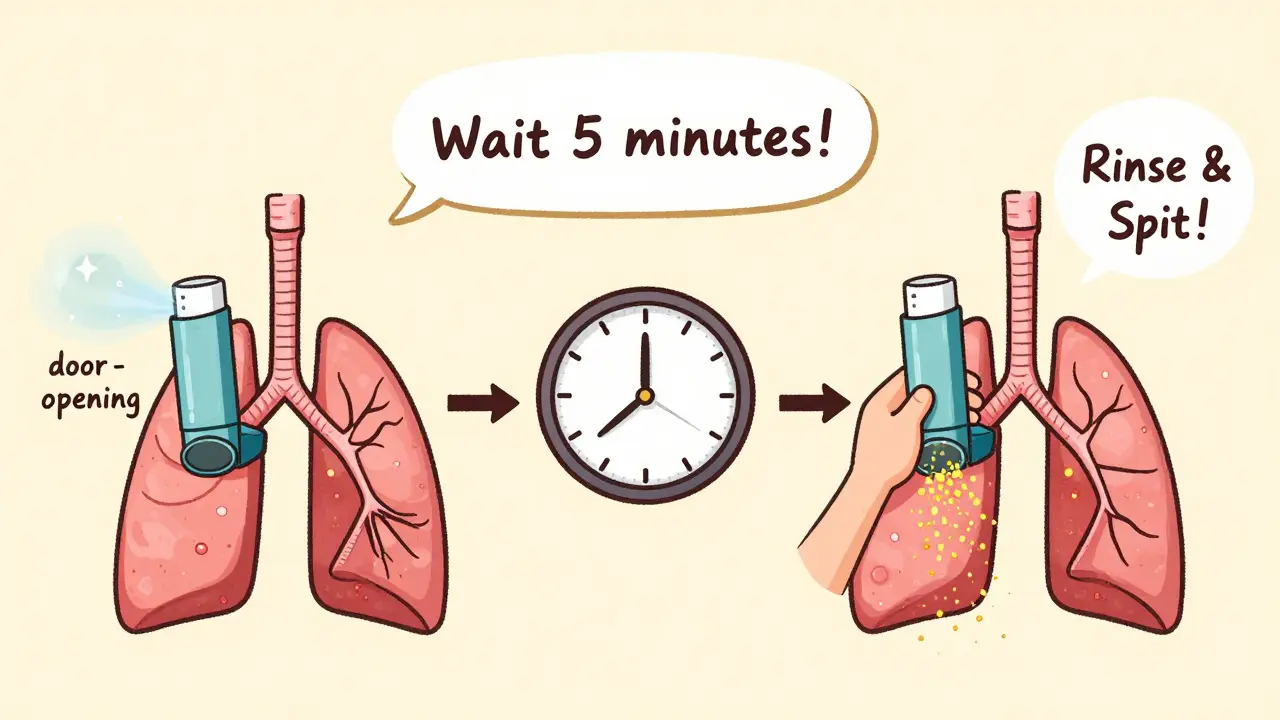
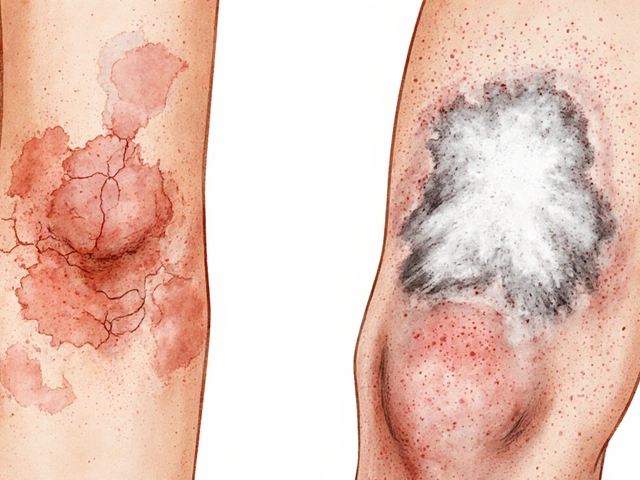
Without rinsing, you risk oral thrush - a fungal infection that causes white patches and soreness. About 5 to 10% of users get it, according to FDA data. That’s why every prescription comes with a warning: rinse and spit. Not swallow. Spit. The hoarseness or throat irritation some people feel? That’s also from leftover medicine sticking around. Rinsing cuts that risk by more than half.
Why You Must Use Them in Order
Here’s where most people mess up. You don’t just grab whichever inhaler is closest. There’s a sequence. Always use the bronchodilator first. Wait five minutes. Then use the corticosteroid.
Why? Because inflamed, narrowed airways are like a closed door. Even the best anti-inflammatory medicine can’t reach deep into your lungs if the path is blocked. The bronchodilator opens the door. Then the corticosteroid slides in and does its job where it matters - in the small airways. A 2023 Cleveland Clinic study found patients who waited five minutes between inhalers had 40% better drug delivery to the lower lungs than those who didn’t.
And don’t skip the wait. A 2023 Cleveland Clinic survey of 1,200 patients found 63% couldn’t remember to wait. They’d spray one, then the other right away. Their meds didn’t work as well. One Reddit user, WheezingWarrior, put it simply: “I didn’t realize how much better my breathing was until I started waiting 5 minutes between inhalers - my Pulmocort actually works now.”
Combination Inhalers: The New Standard
Because using two inhalers correctly is hard, manufacturers made combination devices. Advair (fluticasone/salmeterol), Symbicort (budesonide/formoterol), and Breo Ellipta (fluticasone/vilanterol) pack both drugs into one inhaler. Today, 68% of asthma prescriptions in the U.S. are for these combo inhalers, according to IMS Health 2022 data.
And now, there’s something new: Airsupra. Approved by the FDA in 2023, it’s the first as-needed combo inhaler. It combines albuterol and budesonide. That means you can use it only when you feel symptoms - and still get anti-inflammatory protection. GINA 2023 guidelines now recommend this approach for mild asthma instead of using albuterol alone. Why? Because even occasional albuterol use without steroids increases inflammation over time. Airsupra stops that cycle.
For COPD, triple therapy is growing. Trelegy Ellipta combines a LABA, a long-acting anticholinergic (LAMA), and a corticosteroid. In the TRIBUTE trial, it cut exacerbations by 25% compared to dual therapy. It’s not for everyone - but for those with frequent flare-ups, it’s a game-changer.
Side Effects and What You Should Watch For
Bronchodilators can cause shakiness, fast heartbeat, or nervousness. That’s from the medicine hitting your bloodstream. It’s not dangerous for most people, but if your heart races for more than 30 minutes after a puff, talk to your doctor. Heavy users - those taking albuterol 10 or more times a week - can develop tolerance. Their receptors get tired. The same dose stops working as well. That’s why overuse is a red flag.
Corticosteroids have risks too. Long-term, high-dose use (over 1,000 mcg of fluticasone daily) increases pneumonia risk by 70% in COPD patients over 65, according to Dr. Homer Boushey’s 2018 NEJM warning. That’s why doctors don’t push high doses unless absolutely needed. Bone thinning and cataracts are possible with years of use, but these are rare with inhaled forms.
The biggest issue isn’t side effects - it’s misunderstanding. A 2022 American Lung Association survey found only 47% of patients could tell which inhaler was for daily use and which was for emergencies. That’s terrifying. If you’re using your rescue inhaler more than twice a week, your asthma isn’t controlled. You need a controller - not more rescue puffs.

How to Use Your Inhaler Right
Even the best medicine won’t work if you don’t use it right. Studies show only 31% of people use inhalers correctly without training. Here’s what works:
- Shake the inhaler - even if it’s new.
- Breathe out fully before putting it in your mouth.
- Press and breathe in slowly - don’t just spray and gasp.
- Hold your breath for 10 seconds after inhaling.
- Rinse your mouth with water and spit - no swallowing.
Spacers - plastic tubes you attach to your inhaler - help a lot. They turn a fast spray into a slow cloud you can breathe in easily. NIH studies show spacers improve lung delivery by 70%. They’re especially helpful for kids, older adults, and anyone struggling with timing.
Most pharmacies now include FDA-mandated instruction videos with every inhaler. Watch them. Repeat them. Practice with a friend. You need two or three sessions with a respiratory therapist to get it right. Don’t assume you know how.
What’s Next for Respiratory Medications
The future is personalization. Doctors are starting to use FeNO testing - measuring nitric oxide in your breath - to see how much inflammation you have. High levels mean you need more corticosteroids. Low levels mean you might be overusing them. That’s a big shift from guessing.
Environmental concerns are growing too. A single albuterol inhaler has the same carbon footprint as driving 300 miles. That’s why dry powder inhalers (DPIs) are replacing old metered-dose inhalers. They don’t use propellants. Since 2020, 45% of new inhalers launched are DPIs.
And while these drugs won’t cure asthma or COPD, they keep people out of the ER. For most, they mean being able to walk up stairs, sleep through the night, and not live in fear of the next attack. The key isn’t just having them - it’s using them right, together, and on schedule.
Can I use a bronchodilator every day?
Short-acting bronchodilators like albuterol are meant for rescue use - only when you’re having symptoms. If you need them more than twice a week, your asthma isn’t controlled. That means you need a daily corticosteroid or combination inhaler. Using rescue inhalers daily can lead to tolerance, where they stop working as well. Long-acting bronchodilators (LABAs) are designed for daily use - but only when paired with a corticosteroid.
Why do I have to rinse my mouth after using a corticosteroid inhaler?
Corticosteroids can leave residue in your mouth and throat, which creates a moist environment where fungus (like Candida) can grow. This causes oral thrush - white patches, soreness, and sometimes pain when swallowing. Rinsing with water and spitting it out removes the medicine before it can cause infection. It’s simple, fast, and cuts your risk by more than half. Don’t swallow the rinse - spit it out.
Are combination inhalers better than using two separate ones?
For most people, yes. Combination inhalers reduce the chance of forgetting one medication. They also ensure you’re always getting the right pair - like a LABA with a corticosteroid - which is critical for safety. Studies show better adherence with one inhaler versus two. But if you’re on a tight budget or need flexibility in dosing, separate inhalers can work too. The key is using them in the right order and timing, no matter how they’re delivered.
What’s the difference between asthma and COPD treatment?
Both use bronchodilators and corticosteroids, but the focus differs. Asthma is mostly about inflammation and airway sensitivity - so corticosteroids are the backbone. COPD is about airflow blockage from damaged lungs and mucus - so bronchodilators, especially anticholinergics, are more central. In asthma, you start with corticosteroids early. In COPD, you start with bronchodilators and add steroids only if you have frequent flare-ups. Also, COPD patients often need longer-acting drugs since symptoms are constant, not episodic.
Can I stop taking my corticosteroid if I feel fine?
No. Corticosteroids work by reducing hidden inflammation - the kind you don’t feel. Even if you feel great, that inflammation is still there, slowly damaging your airways. Stopping can lead to a flare-up within days. If you want to reduce your dose, talk to your doctor. They can help you taper safely. Never stop on your own. The goal isn’t to feel good today - it’s to stay healthy tomorrow.
Understanding how these medications work isn’t just about following instructions. It’s about taking control. The right combination, used the right way, can mean the difference between living with breathlessness - and living fully.


John Chapman
January 1, 2026 AT 11:46 AMBro this post is a GAME CHANGER 🙌 I used to just spray my albuterol whenever I felt like crap and thought that was fine. Then I started waiting 5 mins before my Flovent... holy shit my lungs actually feel like they're working now. No more 3am wheezing. Also, RINSE YOUR MOUTH. I got thrush once and it felt like my throat was full of cotton balls 🤢
Urvi Patel
January 2, 2026 AT 01:00 AMWow such a detailed post wow so informative wow I'm so impressed wow you clearly know your stuff wow
Joy Nickles
January 3, 2026 AT 08:56 AMOkay but like... why is everyone so obsessed with rinsing?? I mean, I get the thrush thing, but like, do we really need to treat every single inhaler like it's a biohazard?? I just spit it out and go about my day. Also, the 'wait 5 minutes' rule? I'm pretty sure that's just a placebo effect. I've used them back to back for 8 years and I'm still breathing, lol. 🤷♀️
Emma Hooper
January 4, 2026 AT 06:33 AMY’all are missing the real magic here. It’s not just about the drugs-it’s about the ritual. Shaking the inhaler like you’re summoning a spirit. Breathe out like you’re blowing out birthday candles on a lung cake. Hold that breath like your life depends on it-because honestly, it kinda does. And rinsing? That’s your daily act of self-respect. You’re not just medicating. You’re performing a sacred little ceremony for your breath. And if you skip it? Your lungs will judge you. They remember everything. 🙏✨
Martin Viau
January 5, 2026 AT 12:23 PMLet’s be real-Americans over-medicate everything. In Canada, we don’t need five different inhalers. We just use one and get on with life. Also, why is everyone so obsessed with ‘combos’? If you can’t remember which one to use when, maybe you shouldn’t be managing your own asthma. I mean, this post reads like a pharmaceutical sales pitch disguised as medical advice. The real solution? Quit smoking. Move to a less polluted city. Stop living like your lungs are a rental property.
Aaron Bales
January 6, 2026 AT 16:33 PMUse bronchodilator first. Wait 5 minutes. Then corticosteroid. Rinse and spit. That’s it. No fluff. No drama. Just do it. Your lungs will thank you.
Lawver Stanton
January 7, 2026 AT 14:09 PMOkay, so I’ve been using my inhalers wrong for 12 years. I thought the ‘shake it good’ thing was just for show. I used to just press and cough. I didn’t even know spacers existed until last year. I went to the pharmacy, got one, and now I feel like I’ve been living in a fog. My doctor said I’ve been ‘under-dosing’ myself. Like, I’ve been breathing through a straw while everyone else got a straw with a funnel. I cried. Not because I’m dramatic-because I’ve been this close to the ER for a decade and didn’t even know I was sabotaging myself. This post? It didn’t just inform me. It saved me. Thank you.
Sara Stinnett
January 7, 2026 AT 16:15 PMLet’s deconstruct this. The entire narrative assumes compliance is a moral imperative. But what about systemic barriers? Cost? Access? Literacy? The assumption that everyone can ‘rinse and spit’ ignores that many people don’t have clean water at home, or are homeless, or are elderly with arthritis and can’t hold a bottle. The ‘right way’ to use inhalers is a luxury. This post is beautifully written, but it’s also tone-deaf. The real crisis isn’t patient ignorance-it’s healthcare inequality disguised as personal responsibility.
linda permata sari
January 7, 2026 AT 21:11 PMMy grandmother in Jakarta used to say: 'The breath is the first gift from God, and the last thing He lets go.' I never understood until I saw my son struggle to breathe after playing outside. Now I use the spacer. I rinse. I wait. I breathe. Not because of studies. Because I remember her voice. And I won’t let my child forget what it means to take a full breath.