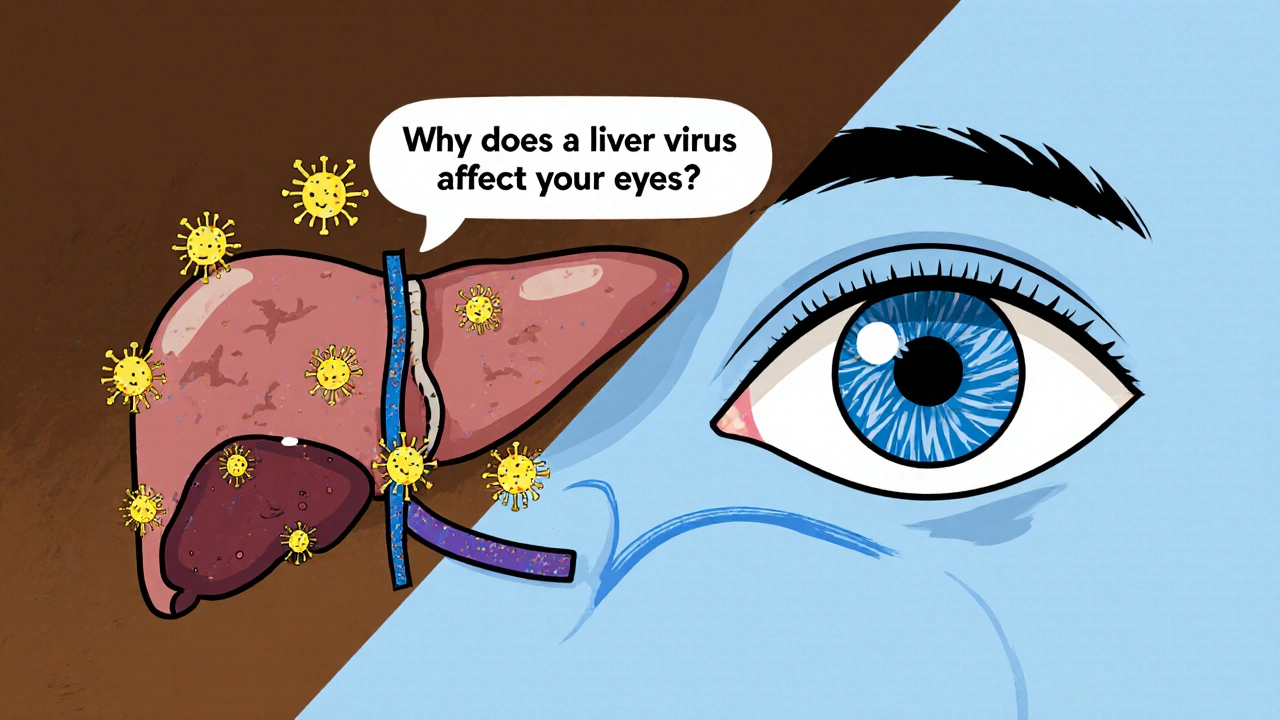
When dealing with HCV eye health, the impact of Hepatitis C virus on vision and ocular structures. Also known as Hepatitis C ocular complications, it can affect everything from the surface of the eye to the retina. Understanding these effects helps you spot problems early and get the right care.
Hepatitis C, a blood‑borne virus that primarily attacks the liver often reveals itself in the eye before any liver damage is obvious. The virus’s persistent presence, the body’s immune response, and chronic inflammation can all trigger ocular complications such as dry eye, cataracts, or retinal vasculitis. In short, HCV eye health reflects how a liver‑focused disease can spill over into vision, making eye exams a valuable early warning system.
Ocular complications, vision‑related issues linked to systemic diseases linked to HCV include peripheral retinal hemorrhages, optic neuritis, and uveitis. These conditions arise because the virus or the immune reaction damages tiny blood vessels that feed the retina and other eye structures. The damage can lead to blurred vision, floaters, or even sudden vision loss. Recognizing these red flags early can prevent permanent impairment.
One of the biggest drivers behind eye problems in HCV patients is the level of liver dysfunction. When the liver can’t filter toxins efficiently, waste products build up in the bloodstream and settle in the eye’s delicate tissues. This buildup can cause “yellow‑white” deposits on the cornea (known as Kayser‑Fleischer‑like rings) and contribute to cataract formation at a younger age. In short, liver disease influences eye health through toxin accumulation, altered blood flow, and reduced production of essential proteins.
Effective antiviral therapy can dramatically reduce eye‑related issues. Direct‑acting antivirals (DAAs) clear the virus in over 95 % of cases, which often leads to a rapid decline in retinal inflammation and a slower progression of cataracts. However, some older treatment regimens, especially those that included interferon, were notorious for causing dry eye and even optic neuropathy. Understanding which drugs are in use and monitoring side effects is essential for protecting vision during treatment.
The immune response itself can be a double‑edged sword. While the body fights off the virus, inflammatory cells may mistakenly attack ocular tissue, leading to vasculitis or macular edema. Patients with co‑existing conditions such as HIV or autoimmune disorders face an even higher risk because their immune systems are already on high alert. Managing systemic inflammation through lifestyle changes, nutrition, and, when needed, anti‑inflammatory medication can help keep the eyes safe.
Regular eye screening is the most practical prevention step. Comprehensive dilated exams let eye doctors see the retina, optic nerve, and blood vessels in detail. Imaging tools like optical coherence tomography (OCT) can spot subtle swelling before it becomes symptomatic. For anyone diagnosed with Hepatitis C, an annual eye check‑up is a smart rule of thumb, especially if liver function tests show moderate to severe impairment.
Beyond medical treatment, everyday habits matter. Staying hydrated, using preservative‑free artificial tears, and protecting the eyes from UV light with quality sunglasses can reduce dry‑eye symptoms and slow cataract formation. A balanced diet rich in omega‑3 fatty acids, lutein, and vitamin A supports retinal health, while limiting alcohol and smoking cuts down on additional liver stress that would otherwise aggravate eye problems.
The collection below dives deeper into each of these topics. You’ll find symptom checklists, treatment overviews, lifestyle tips, and the latest research on how Hepatitis C interacts with your vision. Use these resources to stay ahead of potential issues and keep your eyes as healthy as possible.
Explore how genotype 3 chronic hepatitis C can affect eye health, the symptoms to watch for, screening steps, and treatment options to safeguard vision.
read more