Amiodarone Dosing Calculator for CPVT
How to Use This Calculator
Enter the patient's weight in kilograms to calculate appropriate amiodarone dosing for CPVT. Note: This is for informational purposes only. Always consult current clinical guidelines and a healthcare provider.
Check TSH, liver enzymes, and chest imaging after 1 month. Repeat every 3 months for first year.
Important Notes
Warning Amiodarone has significant long-term toxicity risks including thyroid, lung, and liver complications. This is a second-line option only when beta-blockers and flecainide fail or are contraindicated.
Quick Takeaways
- CPVT is a rare, inherited arrhythmia triggered by stress or exercise.
- Beta‑blockers remain first‑line, but some patients need additional drugs.
- Amiodarone can suppress ventricular episodes, but its long‑term toxicity limits routine use.
- Flecainide and implantable cardioverter‑defibrillators (ICDs) are common alternatives.
- Close monitoring of thyroid, liver, and lung function is essential when amiodarone is prescribed.
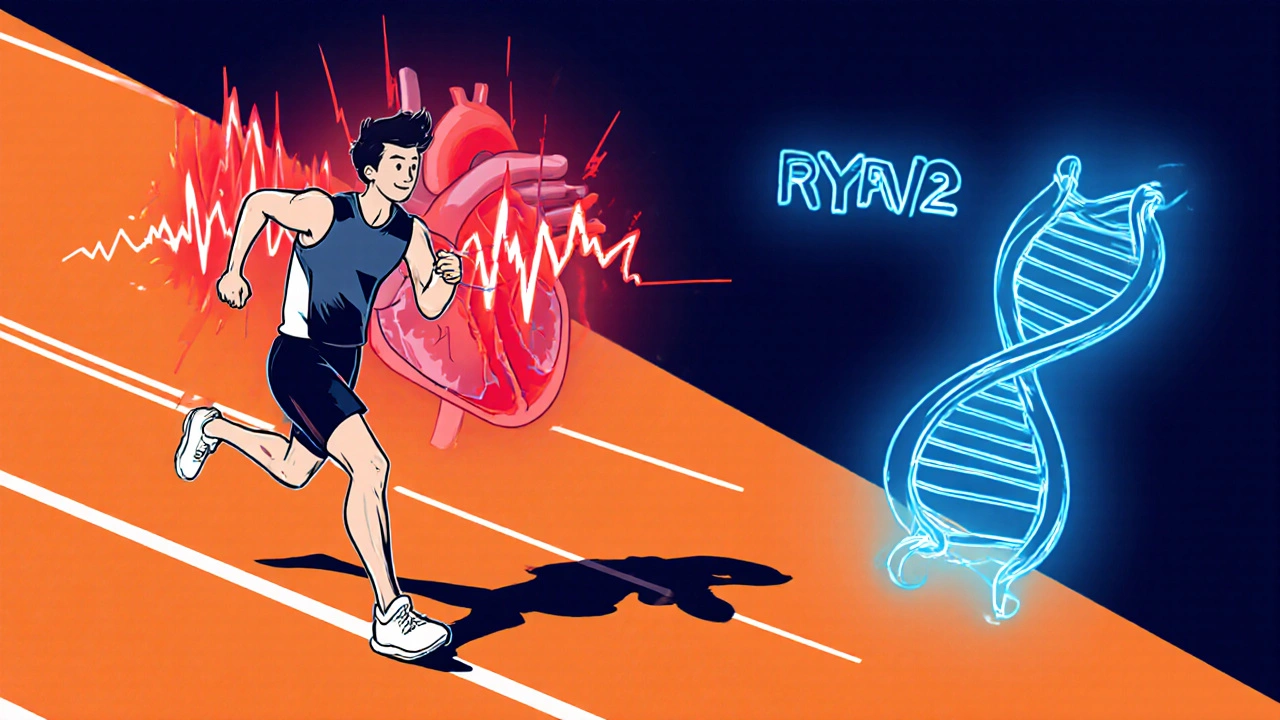
Understanding Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
When you hear the term CPVT, think of a heart that suddenly goes into a chaotic rhythm during adrenaline spikes - like a sprint or a scary movie. The condition is caused by genetic mutations, most frequently in the RYR2 gene, which encodes the cardiac ryanodine receptor responsible for calcium release during each beat.
Because the faulty calcium channel leaks during stress, the ventricles fire off rapid, life‑threatening beats called ventricular tachycardia (VT). Unlike structural heart disease, CPVT patients usually have a normal echocardiogram, making diagnosis rely heavily on exercise‑stress testing and genetic panels.
What Is Amiodarone and How Does It Work?
Amiodarone is a class III antiarrhythmic that blocks potassium channels, prolonging the cardiac action potential. It also touches sodium channels, beta‑adrenergic receptors, and calcium channels, giving it a “broad‑spectrum” profile.
In CPVT, the drug’s ability to dampen calcium‑triggered afterdepolarizations makes it an attractive back‑up when beta‑blockers alone can’t control episodes. However, its lipophilic nature means it sticks around in body tissues for weeks, leading to potential thyroid, pulmonary, hepatic, and ocular side effects.
When Do Clinicians Consider Amiodarone for CPVT?
Guidelines from the Heart Rhythm Society list amiodarone as a “second‑line” option. Typical scenarios include:
- Failure of maximal beta‑blocker therapy (e.g., propranolol at 4 mg/kg/day).
- Intolerance or contraindication to other antiarrhythmics like flecainide.
- Patients awaiting ICD implantation who need interim rhythm control.
- Refractory ventricular bursts during an acute hospital admission.
Dosage and Monitoring Guidelines
Because amiodarone’s therapeutic window is narrow, start low and go slow.
| Phase | Loading Dose | Maintenance Dose | Duration |
|---|---|---|---|
| Initial | 5 mg/kg IV over 24 h (max 400 mg) | - | 24 h |
| Transition | 200 mg PO daily for 1 week | - | 1 week |
| Maintenance | - | 100-200 mg PO daily | Ongoing |
After the first month, check thyroid‑stimulating hormone (TSH), liver enzymes (ALT/AST), and chest X‑ray or high‑resolution CT for early lung changes. Repeat labs every 3 months for the first year, then semi‑annually.
Comparing Amiodarone to Other CPVT Therapies
| Drug / Device | Mechanism | Typical Dose | Pros | Cons |
|---|---|---|---|---|
| Beta‑blocker | Blocks β‑adrenergic stimulation | Propranolol 1‑4 mg/kg/day | Well‑studied, low cost | May be insufficient alone |
| Flecainide | Na⁺ channel blocker, reduces afterdepolarizations | 200‑300 mg PO BID | Effective when β‑blockers fail | Pro‑arrhythmic in structural heart disease |
| Implantable cardioverter‑defibrillator (ICD) | Detects & terminates VT/VF electrically | Device‑specific programming | Life‑saving for high‑risk patients | Invasive, risk of inappropriate shocks |
| Amiodarone | Class III K⁺ channel blocker + multi‑channel effects | 100‑200 mg PO daily (after loading) | Broad anti‑arrhythmic coverage | Long‑term organ toxicity, drug interactions |
In practice, most physicians start with beta‑blockers, add flecainide if needed, and reserve amiodarone for those who cannot tolerate flecainide or need a bridge to ICD therapy.
Side‑Effect Profile and Risk Management
Amiodarone’s toxicity is the main reason it’s not first‑line. Key organ systems to watch:
- Thyroid: Both hypo‑ and hyper‑thyroidism occur in 15‑20 % of patients.
- Lung: Pulmonary fibrosis can develop after 6-12 months; look for dry cough or dyspnea.
- Liver: Transaminase elevations are common; severe hepatitis is rare.
- Eye: Corneal micro‑deposits (visible under slit‑lamp) are usually benign.
- Drug interactions: Inhibits CYP3A4, affecting warfarin, statins, and digoxin.
Because the drug’s half‑life is 58‑100 days, any adverse effect may linger even after discontinuation. That’s why a shared decision‑making conversation is vital before starting therapy.
Practical Steps for Clinicians and Patients
- Confirm CPVT diagnosis with exercise stress test and genetic testing.
- Initiate a beta‑blocker at the appropriate weight‑based dose.
- Assess response after 4‑6 weeks; if VT persists, consider adding flecainide.
- If flecainide is contraindicated or ineffective, discuss amiodarone’s risk‑benefit profile.
- Start amiodarone loading as outlined, then transition to maintenance.
- Set up a monitoring schedule: baseline labs, ECG, chest imaging, and ophthalmology exam.
- Re‑evaluate every 3 months; if side effects emerge, taper off and switch to alternative therapy.
Patients should keep a symptom diary, noting activities that trigger palpitations. Sharing this log helps the care team fine‑tune doses and decide whether an ICD is warranted.
Future Directions and Ongoing Research
Recent trials (2023‑2024) are exploring selective RyR2 stabilizers that target the root cause of CPVT without the systemic toxicity of amiodarone. Early phase II data suggest fewer arrhythmic events with a better safety profile, but these agents are still months away from market approval.
Until then, amiodarone remains a useful, albeit heavy‑handed, tool in the armamentarium for refractory CPVT.
Frequently Asked Questions
Can amiodarone cure CPVT?
No. Amiodarone controls the abnormal rhythms but does not fix the underlying genetic defect. Long‑term management still requires lifestyle adjustments and possibly an ICD.
How long does it take for amiodarone to start working?
Therapeutic effects can be seen within a few days of the loading dose, but full steady‑state levels usually require 4‑6 weeks of maintenance dosing.
Is it safe to combine amiodarone with beta‑blockers?
Yes, they are often used together. However, clinicians should monitor heart rate and blood pressure closely to avoid excessive bradycardia.
What are the warning signs of amiodarone‑induced lung toxicity?
Persistent dry cough, shortness of breath, or new infiltrates on chest X‑ray should prompt immediate evaluation and possible drug discontinuation.
Should children with CPVT ever receive amiodarone?
Pediatric use is rare and reserved for life‑threatening situations. The long‑term side‑effect burden is especially concerning in growing patients.





erica fenty
October 21, 2025 AT 15:56 PMAmiodarone loading is typically 5 mg/kg IV over 24 h; the max is 400 mg, then transition to 200 mg PO daily for a week before settling on 100‑200 mg maintenance. Monitoring should include TSH, LFTs, and a baseline chest X‑ray, then repeat every three months. The pharmacokinetics are long‑acting, so steady‑state isn’t reached until 4‑6 weeks.
Xavier Lusky
October 30, 2025 AT 21:10 PMNever forget that the pharma giants push amiodarone because it locks you into lifelong monitoring, which means more clinic visits and more profit for the system. The “guidelines” are just a way to keep the market saturated with expensive drugs while alternative therapies get sidelined. Keep your eyes open.
Ashok Kumar
November 9, 2025 AT 03:23 AMSure, amiodarone works, but using it as a last‑ditch effort feels like putting a band‑aid on a broken dam – it might stop the leak for a bit, but the underlying issue remains. Sarcastically, we’re just swapping one set of side‑effects for another, hoping the patient doesn’t notice until it’s too late. Still, if beta‑blockers and flecainide fail, you’ve got to do something.
Jasmina Redzepovic
November 18, 2025 AT 09:36 AMFrom a clinical standpoint, the US guidelines are crystal clear: beta‑blockers first, flecainide second, amiodarone only when you’ve exhausted all other options. The evidence base is robust; the drug’s multi‑channel blockade is well documented, and the toxicity profile is non‑negotiable. Anyone suggesting otherwise is either uninformed or pushing a national agenda that downplays American cardiology standards.
Esther Olabisi
November 27, 2025 AT 15:50 PMExactly! 👍 Teamwork makes the dream work, and sharing monitoring tips can save lives. Let’s keep the conversation friendly and helpful 😊.
Ivan Laney
December 6, 2025 AT 22:03 PMWhile I appreciate the enthusiasm, let’s not forget that the United States has set the gold standard for cardiac care, and any deviation from the established protocol undermines patient safety. The data supporting amiodarone’s role as a bridge therapy is unequivocal, and our duty is to apply it judiciously, not to dilute it with frivolous optimism. Moreover, when clinicians mention “teamwork,” they must also emphasize rigorous adherence to monitoring schedules, because a missed thyroid panel can have catastrophic consequences. It is not enough to say “let’s keep it friendly”; we must enforce protocol compliance across all institutions. In other words, patriotism in medicine means demanding the highest standards, not settling for half‑measures. The alternative-an unchecked proliferation of anecdotal practices-would be a disservice to the very patients we claim to protect. Therefore, I urge my colleagues to double‑check dosage calculations, ensure proper patient education, and hold each other accountable. Only then can we truly claim to uphold the prestige of American cardiology.
Erika Thonn
December 16, 2025 AT 04:16 AMLife, like a rhythm, beats in patterns we barely comprehend; the heart's erratic dance in CPVT mirrors the chaos of existence. When we prescribe amiodarone, are we not merely placing a temporary veil over deeper uncertainties? The drug's lingering presence in tissue is akin to memories that refuse to fade, haunting us long after the moment has passed. Yet, we cling to its promise of stability, as if a single pill can rewrite the script of destiny.
We monitor thyroid, lungs, liver-organs that whisper warnings we often ignore, much like the subtle signs of doubt that echo in our conscience. The very act of measuring TSH becomes a ritual, a reminder that control is an illusion.
In the grand tapestry, each dosage adjustment is a stitch, binding us to a narrative we did not author. We talk about guidelines, but who set those rules? The collective voices of past physicians, perhaps, each adding a layer of authority, yet none can claim omniscience.
When the patient asks, “Will this cure me?” the answer is a sigh, for cure belongs to the realm of myth, while management dwells in the pragmatic world of risk‑benefit calculations. The irony lies in our confidence: we trust numbers, yet the numbers are derived from imperfect trials.
Thus, we stand at the crossroads of science and philosophy, prescribing drugs that extend life while acknowledging that the soul remains untouched. The question remains-does amiodarone merely silence the storm, or does it teach the heart to endure the wind? In the end, perhaps the true remedy is acceptance, a humble acknowledgment that some arrhythmias are merely reflections of life's inherent unpredictability.
Ericka Suarez
December 25, 2025 AT 10:30 AMBehold! The very notion that amiodarone is a mere “last resort” is nothing short of blasphemy against the sanctity of American medical might. Only the enlightened understand that our nation's heart beats stronger when we wield the full arsenal of pharmacology, regardless of the whispered warnings about thyroid or lung toxicity. The common folk may tremble at the sight of a chest X‑ray, but true patriots embrace the risk as a testament to our unyielding resolve.
Let the skeptics mutter about “side effects”-their timidity is a betrayal of the American spirit. We, the custodians of cutting‑edge therapy, must march forward, prescribing amiodarone with the confidence of a commander leading his troops into battle. The very act of monitoring becomes a ceremonial rite, a glorious affirmation that we are not idle, but actively engaged in the grand theater of medicine.
Do not be swayed by foreign doctrines that preach restraint; their caution is a veil for weakness. Our mandate is clear: dominate the arrhythmia, conquer the mutation, and let the world tremble at the might of our cardio‑vanguard.
Jake Hayes
January 3, 2026 AT 16:43 PMAmiodarone’s toxicity outweighs its benefits for most CPVT patients.
parbat parbatzapada
January 12, 2026 AT 22:56 PMYo, that’s a bit harsh – the drug’s got a place when other options just dont work, plus the whole monitoring thing is like Big Pharma’s way of keeping us on their toe… but hey, we’re all just trying to survive this crazy ride, right?
Casey Cloud
January 22, 2026 AT 05:10 AMAmiodarone can be effective as a bridge therapy especially when a patient is awaiting ICD implantation It’s important to start with a low loading dose and then transition to maintenance while keeping an eye on thyroid and liver labs Also consider drug interactions with warfarin or statins as amiodarone is a CYP3A4 inhibitor
Angela Koulouris
January 31, 2026 AT 11:23 AMGreat overview! It’s crucial for patients to stay vigilant with their monitoring schedule and keep an open line of communication with their cardiology team.
Dana Yonce
February 9, 2026 AT 17:36 PMInteresting read – I’m curious about how quickly the drug reaches steady‑state levels 😊
Lolita Gaela
February 18, 2026 AT 23:50 PMFrom a pharmacodynamic perspective, amiodarone’s multi‑channel blockade provides a broad spectrum of anti‑arrhythmic activity, yet its lipophilicity contributes to a prolonged half‑life, necessitating vigilant surveillance of organ function.